| Author | Affiliation |
|---|---|
| Sanober B. Shaikh, MD | Inova Fairfax Hospital, Falls Church, Virginia |
| David A. Jerrard, MD | University of Maryland, School of Medicine, Baltimore, Maryland |
| Michael D. Witting, MD | University of Maryland, School of Medicine, Baltimore, Maryland |
| Michael E. Winters, MD | University of Maryland, School of Medicine, Baltimore, Maryland |
| Michael N. Brodeur, BS | University of Maryland, School of Medicine, Baltimore, Maryland |
ABSTRACT
Introduction:
Our goal was to evaluate patients’ threshold for waiting in an emergency department (ED) waiting room before leaving without being seen (LWBS). We analyzed whether willingness to wait was influenced by perceived illness severity, age, race, triage acuity level, or insurance status.
Methods:
We conducted this survey-based study from March to July 2010 at an urban academic medical center. After triage, patients were given a multiple-choice questionnaire, designed to ascertain how long they would wait for medical care. We collected data including age, gender, race, insurance status, and triage acuity level. We looked at the association between willingness to wait and these variables, using stratified analysis and logistic regression.
Results:
Of the 375 patients who were approached, 340 (91%) participated. One hundred seventy-one (51%) were willing to wait up to 2 hours before leaving, 58 (17%) would wait 2 to 8 hours, and 110 (32%) would wait indefinitely. No association was found between willingness to wait and race, gender, insurance status, or perceived symptom severity. Patients willing to wait >2 hours tended to be older than 25, have higher acuity, and prefer the study site ED.
Conclusion:
Many patients have a defined, limited period that they are willing to wait for emergency care. In our study, 50% of patients were willing to wait up to 2 hours before leaving the ED without being seen. This result suggests that efforts to reduce the percentage of patients who LWBS must factor in time limits.
INTRODUCTION
In 2008 an estimated 124 million patients sought emergency care in the United States.1This number grows every year. Unfortunately, as patient volume increases, crowding and emergency department (ED) boarding of patients waiting to be admitted to the hospital increase as well.1 This leads to prolonged wait times for many patients seeking emergency care.
The ED functions as a healthcare “safety net,” providing full-time services for the general public.2 Patients come to the ED for evaluation of emergent or urgent conditions, for after-hours medical care, or by referral from their primary physician. In striving to fulfill this vital role, EDs across the country struggle to balance demand and capacity.
Previous studies have shown that the longer patients wait, the more likely they are to leave without being seen (LWBS).3 Studies have also shown that a significant portion of patients who LWBS are classified as needing emergent or urgent medical care.4 The question of interest to our group was this: How long are patients willing to wait before they choose to LWBS by a health care provider?
Our study sought to evaluate patients’ threshold for waiting before they choose to leave the ED waiting room without being seen by an ED provider. We also sought to determine whether willingness to wait was influenced by factors such as illness severity, age, or insurance status. Knowing the limits to which patients will wait may be useful in tailoring strategies to reduce wait times.
METHODS
Settings and Participants
Between March and July 2010, we approached patients waiting for emergency medical care in an urban academic center with approximately 46,000 adult patients annually. Patients were approached after triage but before being seen by a physician. Survey were administered between 8am and 10 pm. Patients were eligible for the study if they were between 18 and 89 years of age and had an emergency severity index (ESI) level of 3, 4, or 5. We excluded patients triaged with a higher acuity level (ESI 1 or 2) because they were taken immediately into the ED for care, without spending any time in the waiting room. We excluded prisoners, as well as patients presenting with psychiatric emergencies, including those arriving on emergency petition. Non-English-speaking patients were not excluded. Patients completed the survey by reading the questions and recording their responses on the survey form. Patients had the option of having the survey questions read to them.
Data Collection
Ten research assistants (first- and second-year medical students) collected data throughout the enrollment period. They received uniform training on survey administration and data recording. Research assistants worked in 4-hour shifts according to the following schedule: 8am to 12pm, 2 to 6pm, and 6 to 10pm. When they approached the patient, the assistants briefly explained the purpose of the study and informed the patient that the survey was anonymous and that participating or not participating in the study would not affect care. Upon enrollment, data were collected using a standardized, multiple-choice questionnaire (Appendix). We gave the patients an information sheet describing the aims of the study and listing contact information that they could use if they had any concerns. Consent was obtained using a brief oral script. The institutional review board approvd this study .
After the survey was administered, we collected the following information: patient age, gender, race, insurance status, employment status, phone status (absence suggesting lower socioeconomic status), triage acuity level, chief complaint, and triage time using the patients’ electronic health record. We also collected this information from those who declined to participate. The time of survey administration and how long the patient had waited prior to being approached were recorded as well.
Data Analysis
We compared demographic variables between respondents and non-respondents to assess the potential for selection bias. Based on the distribution of responses, we dichotomized willingness to wait into groups defined by more than 2 hours versus 2 hours or less. We assessed univariate associations of categories of predictor variables, including strata of ordinal variables versus willingness to wait more than 2 hours. Other ordinal variables were dichotomized as appropriate. We used a stratified analysis to assess for interaction between the following variables and the relationship between acuity and willingness to wait: insurance status, phone status (surrogate for lower socioeconomic status), wait thus far, age category, and need for this ED. We defined potential interaction as a Broselow-Day significance < 0.05.
We prepared a multivariable logistic model that included acuity and any other variables associated with willingness to wait more than 2 hours at significance < 0.1. We removed variables from the model as long as they did not change the model coefficient for acuity by more than 10%, did not decrease the precision for this estimate by more than 10%, or had significant adjusted associations with willingness to wait at P < 0.05.
RESULTS
Of the 375 patients eligible to participate, 340 (91%) consented to complete the questionnaire. One participant answered all of the questions except how long he/she was willing to wait. Characteristics of the study population are shown in Table 1. Figure 1indicates the distribution of stated willingness to wait times, which was bimodal, with 171 (51%) indicating willingness to wait up to 2 hours and 110 (32%) indicating they would be willing to wait indefinitely. The remaining 58 (17%) were willing to wait various times between 2 and 8 hours before leaving. The 35 patients who refused to participate were similar to participants in age distribution, gender, race, insurance status, phone status, acuity level, and wait time prior to contact.
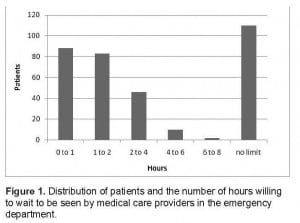
Distribution of patients and the number of hours willing to wait to be seen by medical care providers in the emergency department.

Descriptive data for 340 patients wating for emergency care.
Associations between predictor variables and willingness to wait are shown in Tables 2 and and 3. Among social and demographic factors, including insurance status, race, gender, and age; only age greater than 25 years was independently associated with a willingness to wait longer to be seen. Although patients’ subjective concern for symptoms and severity of symptoms were not statistically associated with willingness to wait, patients with a higher acuity, as indicated by the triage-assigned acuity (ESI level 3), were more willing to wait, by both crude and adjusted analyses. Preference for the study site ED also predicted increased willingness to wait.
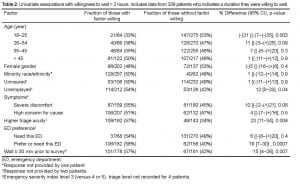
Univariate associations with willingness to wait > 2 hours. Includes data from 339 patients who indicates a duration they were willing to wait.
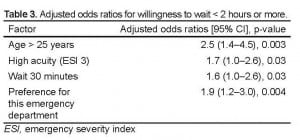
Adjusted odds ratios for willingness to wait < 2 hours or more.
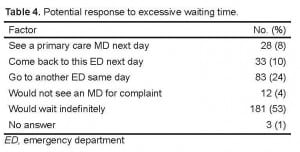
Table 4 displays patients’ responses when asked what they would do next if they decided to leave the waiting room without being seen. The vast majority of patients, 96%, indicated that they would seek care for their health concern elsewhere.
DISCUSSION
Much has been written in the past decade about the large number of patients leaving the nation’s EDs without being seen by a physician.2,3 Wait times for patients desiring to be seen by an emergency physician can stretch for hours. Additionally, the annual census of the nation’s EDs continues to be well above 100 million patient visits.
At a certain time, patients may decide that waiting longer to see a physician in the ED waiting room is beyond what they can tolerate.5–7 Our study evaluated the length of time that patients stated they were willing to wait before leaving without being seen and what variables may be associated with a willingness to wait longer. Of the 340 patients who participated, 171 (51%) had a threshold of 2 hours. Among demographic factors, only age above 25 years was independently associated with a willingness to wait more than 2 hours. Previous studies looking at characteristics of patients who left without being seen had also found that younger patients have a higher uncompleted visit rate compared with older individuals.4,8 Those studies made no mention of when the patients left or how long they waited.
Our study found that patients whose conditions were deemed to be of higher acuity by the triage nurse were more willing to wait beyond 2 hours. This disconnect might have been due in part to conveyance to the patient by the triage nurse, purposeful or not, as to the level of severity of his/her presenting illness. This might have influenced the patient’s decision. Interestingly, we did not find the same willingness to wait among patients who classified themselves as being in severe discomfort and/or having a high level of concern for their symptoms.
A preference for the study site ED also was associated with a willingness to wait beyond 2 hours. Although we did not explore the specific reasons for this preference when the study was conducted, we feel that the effect of ED preference on a patient’s willingness to wait is plausible and not surprising. Every ED has its core group of patients who return for treatment of varying illnesses. For reasons of convenience (access, location) and/or comfort with the care they have received in the past at the facility, a preference develops and is likely to mitigate perceived or actual wait times. Additionally, given that our study site is a tertiary care facility, some patients may require specialty care at our hospital and may feel they cannot receive the same care at other hospital EDs.
An encouraging finding in our study was that in response to excessive wait times, 96% of our cohort would continue to seek the services of a healthcare provider for their illness. They could find this help by seeing their primary care physician the following day, going to another ED that same day, returning to the same ED later in the day, or just waiting indefinitely at the survey site ED.
LIMITATIONS
Our major limitation is that we did not survey patients from 10pm to 8am. Patients who present during the overnight hours may be more inclined to wait because they have limited alternative care options. In addition, our study population consisted of ED patients presenting to an inner city, academic, tertiary care referral center. The study group was predominantly African-American. Over 50% of patients surveyed preferred our ED. These patients may have been more inclined to wait because of the inconvenience of going to another ED or because of their familiarity with the study site ED. Patients’ willingness to wait may be different in a community, non-academic setting.
Half of the participants revealed that 2 hours was the limit they would wait. We did not retrospectively review to see how many of these patients stayed true to their initial survey response. There might be a difference between how long patients say they are willing to wait and how long they actually wait. Comparing their initial response with the actual duration of time they decided to stay would have provided additional information regarding willingness to wait. A final limitation involves the exclusion of ESI 1 and 2 patients. Thus, a large group of patients might be excluded from the applicability of the study’s findings.
CONCLUSION
Decreasing the number of patients who LWBS is an important goal for hospitals across the country. The ED has an important role in the country’s healthcare system, providing emergency services as well as care for patients with urgent concerns after hours or with limited access to medical care. Half of the patients we surveyed were willing to wait as long as 2 hours before leaving the ED waiting room without being seen. This finding could be used as a guide to support capacity management decisions, recognizing that the risks and lost revenue from patients leaving without being seen are defined by time constraints. Despite lengthy wait times, it is reassuring that few patients presenting to the ED for evaluation will forego the services of a physician completely. Patients seem to be intent on receiving care for their particular illness, but many have a defined, limited period that they are willing to wait in the ED waiting room.
Footnotes
The authors would like to acknowledge the work of Heather Riggle, Allison Lindell, Ian Rossfrye, Krystle Shafer, Karan Chopra, Howard Fishbein, Fraser Mackay, Erin Knepp, Gelane Gemechisin collecting data for this study. The manuscript was copyedited by Linda J. Kesselring, MS, ELS,the technical editor/writer in the Department of Emergency Medicine at the University of Maryland School of Medicine.
Supervising Section Editor: Jeffrey Druck, MD
Submission history: Submitted September 14, 2011; Revisions recieved Febuary 23, 2012; Accepted March 23, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.3.6895
Address for Correspondence: Sanober B. Shaikh, MD, Department of Emergency Medicine, INOVA Fairfax Hospital, 3300 Gallows Road, Falls Church, VA 22042
Email: sanober1@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Emergency Department Visits. Atlanta, Georgia: Centers for Disease Control and Prevention; Feb 18, 2011. Available at www.cdc.gov/nchs/fastats/ervisits.htm. Accessed on September 14, 2011.
2. Morris D, Gordon J. The role of the emergency department in homeless and disadvantaged populations. Emerg Med Clin North Am. 2006;24:839–48. [PubMed]
3. Baker DW, Stevens CD, Brook RH. Patients who leave a public hospital emergency department without being seen by a physician: causes and consequences. JAMA.1991;266:1085–90. [PubMed]
4. Ding R, McCarthy ML, Li G, et al. Patients who leave without being seen: their characteristics and history of emergency department use. Ann Emerg Med.2006;48:686–93. [PubMed]
5. Derlet RW, Richards JR, Kravitz RL. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med. 2001;8:151–5. [PubMed]
6. Derlet RW, Richards J. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35:63–8. [PubMed]
7. General Accounting Office Hospital Emergency Departments: Crowded Conditions Vary Among Hospitals and Communities. Washington, DC: United States General Accounting Office; 2003. GAO-03-460.
8. Goodacre S, Webster A. Who waits longest in the emergency department and who leaves without being seen? Acad Emerg Med. 2003;22:93–6.