| Author | Affiliation |
|---|---|
| Michael J. Drescher, MD | Hartford Hospital/University of Connecticut, Division of Emergency Medicine, Hartford, Connecticut |
| Shannon Marcotte, MD | University of Connecticut Integrated Residency in Emergency Medicine, Hartford, Connecticut |
| Robert Grant, MD | St Mary’s Hospital, Department of Emergency Medicine, Waterbury, Connecticut |
| llene Staff, PhD | Hartford Hospital, Department of Research Administration, Hartford, Connecticut |
ABSTRACT
Introduction:
A family history of appendicitis has been reported to increase the likelihood of the diagnosis in children and in a retrospective study of adults. We compare positive family history with the diagnosis of acute appendicitis in a prospective sample of adults.
Methods:
We conducted a prospective observational study of a convenience sample of 428 patients. We compared patients with surgically proven appendicitis to a group without appendicitis. The latter were further grouped by their presenting symptoms: those presenting with a chief complaint of abdominal pain and those with other chief complaints. Participants answered questions regarding their family history of appendicitis. Family history was then compared for the appendicitis group versus the nonappendicitis group as a whole, and then versus the subgroup of patients without appendicitis but with abdominal pain. The primary analysis was a χ2 test of proportions and the calculation of odds ratio (OR) for the relationship between final diagnosis of appendicitis and family history.
Results:
Of 428 patients enrolled, 116 had appendicitis. Of those with other diagnoses, 158 had abdominal pain and 154 had other complaints. Of all patients with appendicitis, 37.9% (confidence interval [Cl] = 29.1–46.8) had positive family history. Of those without appendicitis, 23.7% (Cl = 19.0–28.4) had positive family history. In the subgroup without appendicitis but with abdominal pain, 25.9% (Cl = 19.1–32.8) had positive family history. Both comparisons were significant (P = 0.003; OR = 1.97; 95% Cl = 1.2–3.1; and P=0.034; OR = 1.74; 95% Cl = 1.04–2.9, respectively). By multivariate logistic regression analysis across the full sample, family history was a significant independent predictor (P = 0.011; OR = 1.883) of appendicitis.
Conclusion:
Adults presenting to the emergency department with a known family history of appendicitis are more likely to have this disease than those without.
INTRODUCTION
Background
Appendicitis is a common cause of acute abdominal pain, for which surgical intervention is required, and has been recognized as one of the most common causes of the acute abdomen worldwide. In the United States, there are approximately 250,000 cases of appendicitis per year, with an incidence of 1.1 cases per 1,000 people per year.1 The diagnosis hinges on an index of suspicion based on a careful history and physical examination. “Textbook” cases often require no imaging studies and go straight to the operating room; however, many patients do not present with classic symptoms and have nonspecific features, including indigestion, a sense of not feeling well, or nonlocalized pain. The diagnosis of appendicitis can be especially challenging in women and patients older than 60 years owing to the presence of other possible pelvic inflammatory causes in the former and often delayed presentation in the latter.2
Family history is an important factor in the risk stratification of various diseases. Studies done in the late 1970s and 1980s showed a correlation between a positive family history and appendicitis in children.3,4 In a more recent study, Gauderer et al5 performed a prospective case-control study assessing the importance of family history in a pediatric population. In that study children with appendicitis were twice as likely to have a positive family history when compared to controls with right lower quadrant pain that had a diagnosis other than appendicitis. The authors also found that children with appendicitis were 3 times as likely to have a positive family history as controls without abdominal pain. A recent chart review of 2,670 patients reported that a family history of appendicitis increased the likelihood of disease by threefold.6
Importance
To date there is no prospective case control study in adults examining the ability of family history to predict appendicitis in adults.
If it can be shown that family history increases the likelihood for the disease in adults as well as children, it will enhance the ability of the clinician to make the diagnosis on clinical grounds more confidently. This is important since patients for whom the diagnosis cannot be made or ruled out with confidence require further diagnostic testing, usually by computed tomography (CT), with increased costs in time, money, and radiation exposure. The risks of missing the diagnosis with attendant medical and surgical complications are well known. Better risk stratification may ultimately reduce the number of scans performed and improve clinical accuracy.
Objective
The objective of our study was to determine if family history is a risk factor for appendicitis in the adult population and thus, if it can be used as a predictor for the clinical diagnosis of appendicitis.
METHODS
Study Design
We enrolled a convenience sample of patients presenting to the emergency department (ED) into a prospective case-control study. We recruited equivalent numbers of subjects (1:1:1) in case groups and control groups 1 and 2. Sample sizes of 115 in the case group and 115 in the each of the control groups (230 in the combined nonappendicitis group) were calculated to achieve 80% power, to detect a difference of 16% between the null hypothesis, stating that positive family history is present in all groups at a proportion of 14%, and the alternative hypothesis, stating that the proportion in the case group is 30% (an odds ratio [OR] of 2.63), by using a 2-sided χ2 test with continuity correction and with a significance level of 0.05. The study was approved by the institutional review board.
Setting and Population
The setting was a tertiary urban teaching referral center. Patients were enrolled on a convenience basis, both with and without appendicitis, and based on availability of a researcher. Cases and controls were not individually matched. Patients with a diagnosis of appendicitis were identified from hospital admission records by admitting diagnosis, which was confirmed at surgery, and the patients were enrolled during the same admission. Patients were excluded if they were younger than 18 years, adopted, unaware of their family history, critically ill, or had a prior appendectomy.
Study Protocol
All patients were interviewed in person by using a standard data collection form. They were asked specifically whether or not the patient’s parents, brothers, sisters, grandparents, or children had had appendicitis. Gender, age, and ethnicity were also noted. Data were statistically analyzed with SPSS 14.0 (IBM, Armonk, New York).
Measurements
Patients were categorized according to final diagnosis: those with surgically proven appendicitis and those who were otherwise diagnosed. Patients in the latter group were further categorized by their presenting symptoms: those presenting with a chief complaint of abdominal pain and those with other symptoms. A patient was considered to have a positive family history if any first-degree relative or grandparent was known to have had appendicitis. If the patient did not know of a diagnosis of appendicitis in the family, this was taken to be a negative family history.
Data Analysis
The primary analysis was a χ2 test of proportions and the calculation of OR and 95% confidence intervals (95% CI) for the relationship between final diagnosis of appendicitis and family history. We did this to answer the general question of whether patients with appendicitis are more likely to have a positive family history than patients with all other diagnoses. We also, following a previously published methodology, wanted to try and answer a subsidiary question: Are patients with appendicitis more likely to have a positive family history than those patients presenting specifically with abdominal pain but eventually found NOT to have appendicitis? We therefore further compared the appendicitis group to the subgroup of patients without appendicitis who presented with abdominal pain. Logistic regression was used to examine family history in the prediction of the final diagnosis, while controlling for demographic factors.
Outcome Measure
We measured whether the proportion of patients having appendicitis and a positive family history was larger than the proportion of patients in control groups with positive family history.
RESULTS
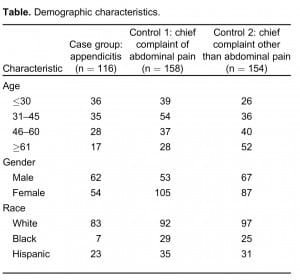
We enrolled 428 patients, 116 of whom had appendicitis and 312 who did not. Among the nonappendicitis group, a subgroup of 158 patients presented with abdominal pain (from another diagnosis) The demographic comparison among the groups is shown in the Table. Significant differences were found in age (P = 0.04), gender (P = 0.005), and race (P =0.04), with younger, male, and white patients more likely to be in the appendicitis group.
Of the 116 patients with appendicitis, 44 (37.9%; CI = 29.1–46.8) had a positive family history. Of all 312 patients without appendicitis, 74 (23.7%; CI = 19.0–28.4) had a positive family history. In the subgroup of 158 patients who presented with abdominal pain but did not have appendicitis, 41 (25.9%; CI= 19.1–32.8) had positive family history. Both comparisons were significant (P=0.003; OR= 1.97; 95% CI= 1.2–3.1; and P =0.034; OR = 1.74; 95% CI = 1.04–2.9, respectively).
Given the presence of significant relationships between diagnosis and demographics in the current data set, we ran a multivariate logistic regression analysis. Family history was a significant independent predictor of a diagnosis of appendicitis among the full sample of patients presenting to the ED (P = 0.011; OR = 1.883; 95% CI=–1.16 to 3.06). When those with appendicitis are compared only to the smaller sample without appendicitis but presenting with abdominal pain, the result, while similar (OR = 1.612; 95% CI = 0.932–2.788), does not reach statistical significance.
DISCUSSION
In our study, patients who presented to the ED with appendicitis were more likely to have a positive family history than those presenting with other diagnoses, whether or not they had abdominal pain. This difference was statistically significant in all comparisons except when using logistic regression analysis and limiting the comparison to those presenting with abdominal pain. The OR in this comparison was similar to the odds ration when comparing all patients (OR, 1.61 vs OR, 1.88). When using a smaller sample, it is more difficult to show statistical significance; in light of the rest of our results, this is likely to account for the discrepancy.
A previous retrospective study of patients taken to the operating room for appendectomy, which compared those having appendicitis to those without, showed an increased incidence of family history in patients with appendicitis versus those without, with a greater difference in those younger than 20 years, for which family history was positive in 45% of cases with appendicitis versus 17% of cases without.7 This study did not apply statistical methodology to its results and was potentially subject to various biases, including work-up bias; however, it was done in an area of India where clinical diagnosis is the sole determinant for surgery, and its findings are consistent with ours.
On its own, the increased likelihood of appendicitis among those with a positive family history is not enough to diagnose or rule out the disease. However, this element—the history of the present illness—will help inform the pretest likelihood of a given patient’s having appendicitis, as the clinician determines the threshold for further testing. The concept of constructing a pretest likelihood from various relatively nonspecific risk factors to determine further testing is well known from the diagnostic algorithms for diseases such as pulmonary embolism and deep vein thrombosis.8,9 We think that taken in the context of the rest of the clinical signs and symptoms, a family history will add modestly to the clinical gestalt of the patient when there is diagnostic uncertainty, especially when CT is not routinely unavailable.
LIMITATIONS
Our study was a convenience sample of patients who presented to a single emergency department. Given this sampling approach, it is not known whether the resulting sample was representative of all adults presenting to ED or whether factors, such as day of week or time of day, or indeed the specific population using this ED, led to any bias. Thus, the resulting sample could be nonrepresentative, and this limits the external validity of the conclusions. The possibility that there were any confounding differences between the groups could limit the internal validity as well. Multivariate regression was used to ameliorate the possible limitations to internal validity, but it is not possible to know how completely this was accomplished. Data were collected during a 4-year period owing to the availability of staff to enroll patients in our study. Recall bias is another potential limitation of our study. Our results relied solely on the patient’s knowledge of their family history. We did not verify whether or not their recall was correct. One may ask whether our study suffers from “work-up bias.” Work-up bias occurs whenever a test is performed and a “gold standard” (reference) validation is not performed for each patient, and accuracy of the test is reported for only patients with reference validation. This is particularly apt to occur when the gold standard involves an invasive procedure.10 In our study, if one takes the gold standard as surgery for probable appendicitis, it is true that not all our patients underwent that procedure in order to definitively rule in (or rule out) the diagnosis. If there were a large group within our sample that had appendicitis but were not taken to surgery, then this might be a confounding factor. However, it is unlikely that our diagnostic test was used to determine which patients would go to surgery. As one source put it, “… we have observed lack of work-up bias only in settings in which a surgeon does not believe in the test or ignores it for purposes of decision making .. .”10
CONCLUSION
This study suggests that, as with other disease processes, knowledge of family history of appendicitis can assist the physician in determining the likelihood of the diagnosis. Given the difficulty in diagnosing appendicitis clinically, this information could be useful in the ED setting.
Footnotes
Supervising Section Editor: Eric R. Snoey, MD
Submission history: Submitted November 29, 201 0; Revision received February 23, 2011; Accepted June 15, 2011
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources,
and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
DOl: 1 0.5811fwestjem.2011.6.6679
Address for Correspondence: Michael J. Drescher, MD, Hartford Hospital/University of Connecticut, Division of Emergency Medicine, 80 Seymour St, Hartford, CT 06102
E-mail: mdresch@harthosp.org
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Addiss DG, Shaffer N, Fowler BS, et al. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910–925. [PubMed]
2. Pittman-Waller VA, Myers JG, Stewart RM, et al. Appendicitis: why so complicated? Analysis of 5755 consecutive appendectomies. Am Surg. 2000;66:548–554. [PubMed]
3. Andersson N, Griffiths H, Murphy J, et al. Is appendicitis familial? Br Med J.1979;2:697–698. [PMC free article] [PubMed]
4. Brender JD, Marcuse EK, Weiss NS, et al. Is childhood appendicitis familial? Am J Dis Child. 1985;139:338–340. [PubMed]
5. Gauderer MW, Vrane MM, Green JA, et al. Acute appendicitis in children: the importance of family history. J Pediatr Surg. 2001;36:1214–1217. [PubMed]
6. Ergul E, Ucar AE, Ozgun YM, et al. Family history of acute appendicitis. J Pak Med Assoc. 2008;58:635–637. [PubMed]
7. Salati SA, Rather AA. Importance of family history and genetics for prediction of acute appendicitis. Internet J Emerg Medicine. 2009;5(2)
8. Wells PS, Owen C, Doucette S, et al. Does this patient have deep vein thrombosis? JAMA.2006;295:199–207. [PubMed]
9. Carpenter CR, Keim SM, Seupaul RA, et al. Differentiating low-risk and no-risk PE patients: the PERC score. J Emerg Med. 2009;36:317–322. [PubMed]
10. Blackstone EH, Lauer MS. Caveat Emptor: the treachery of workup bias. J Thorac Cardiovasc Surg. 2004;128:341–344. [PubMed]