| Author | Affiliation |
|---|---|
| Kapil R. Dhingra, MD, MBA | University of California, Davis Medical Center, Department of Emergency Medicine |
ABSTRACT
This case report describes an atypical presentation of an atypical disease entity: Emphysematous Cystitis, a rapidly progressive, ascending urinary tract infection, in an emergency department (ED) patient whose chief complaint was abdominal pain and who had a urinalysis not consistent with the diagnosis of cystitis.
INTRODUCTION
Emphysematous Cystitis (EC) is an uncommon, rapidly progressive bacterial infection whereby fermentation of albumin or glucose by the urinary pathogen results in gas formation in the bladder wall and lumen. Although it is an uncommon clinical entity, when present it is seen commonly in diabetic patients. Early recognition of EC in the emergency department (ED) can prevent morbidity and mortality resulting from progression of the infection to Emphysematous Pyelonephritis and Urosepsis.
CASE REPORT
A 59-year-old female presented to the ED with a chief complaint of abdominal pain. Her abdominal pain began three hours before presentation and had awoken her from sleep. This abdominal pain was described as “achy,” 5/10, intermittent, and located in the left lower quadrant without radiation. She denied nausea or vomiting and had no diarrhea or blood in her stools. Review of systems revealed that the patient had symptoms of dysuria for one day and left-sided flank pain along with her abdominal pain. She denied fevers or chills. She stated that, despite taking her prescribed insulin injections, her blood sugars have been persistently elevated above 400 with her personal glucometer. Her past medical history was significant for insulin-dependent diabetes mellitus (DM), hypertension, and prior cerebrovascular accident. She denied ever having any surgeries. She used regular insulin, Lantus (insulin glargine), and Ibuprofen. Her family history was noncontributory, and she denied alcohol, tobacco, or illicit drug use.
Physical exam revealed a temperature of 36.5° C, respiratory rate of 18 breaths per minute, heart rate of 93 beats per minute, blood pressure of 166/81 mm Hg, oxygen saturation of 99% on room air, and capillary blood glucose of 447 mg/dL. She was awake, alert, and interacting appropriately. Her pupils were equally round and reactive to light. The cardiac exam was normal and lungs were clear with breath sounds bilaterally. The abdomen was soft with minimal tenderness to palpation in the left periumbilical and left lower quadrant. There was no guarding or rebound. Extremities were warm and well-perfused. The neurological exam revealed no deficit.
The metabolic panel revealed sodium of 132 mEq/L (normal 135–145), BUN of 45 mg/dL (normal 8–22), Creatinine of 2.0 mg/dL (normal 0.5–1.3), glucose of 473 mg/dL, and an anion gap of 8.0. A CBC revealed a white blood cell count of 12.0 K/MM3 (normal 4.5–11.0) and a manual differential with 10.10 K/MM3 Neutrophils (normal 0.80–7.70). The hepatic panel was remarkable for an alkaline phosphatase of 189 U/L (normal 35–115). The urine was visibly clear and non-turbid. Urinalysis was leukocyte esterase and nitrate negative, but revealed large occult blood, glucosuria, protein of 300 mg/DL, and 3–6 WBC/HPF (normal 0–3).
While laboratory studies were pending, the patient received one liter IV normal saline, four mg of morphine sulfate IV for pain, and 10 units of regular insulin. Despite fluid administration and analgesia, the patient continued to have worsening 6/10 abdominal pain. Given the patient’s presentation of undifferentiated abdominal pain without clear etiology and her immunocompromised state, a non-contrast computed tomography (CT) scan of the abdomen was ordered. The CT scan revealed significant air in the bladder wall and lumen consistent with EC, severe left hydroureter and hydronephrosis without evidence of stones, and significant left perinephric stranding without gas in the renal parenchyma (Figure 1).
A gram of Ceftriaxone and 500 mg of Gentamycin were started empirically along with a repeat fluid bolus and placement of a Foley catheter. While awaiting consultation and admission to the Urology service, the patient complained of increased abdominal pain and was increasingly tender in the left lower quadrant and suprapubic region. Her heart rate was persistently tachycardic (in the 130s), and she developed a fever to 39.4°C. In light of developing urosepsis and the potential for rapid progression to Emphysematous pyelonephritis, Interventional Radiology (IR) was consulted and placed a left nephrostomy tube to relieve the functional obstruction of the urinary tract just eight hours after the patient presented to the ED. After nephrostomy tube placement by IR, the patient was admitted to the ICU for close monitoring. The urine culture grew out Klebsiella pneumoniae and the patient was continued on IV antibiotics. Three days after admission, the nephrostomy tube was removed as the patient was able to void without use of a foley catheter and was able to control her pain. She was subsequently discharged and given a prescription for Levofloxacin 500 mg every day for fourteen days.
DISCUSSION
EC, or “Cystitis Emphysematosa”, is a potentially fatal necrotizing infection that can begin in the bladder and rapidly ascend to the renal parenchyma.1,2 The etiology of EC is multifactorial and involves: gas-forming bacteria, decreased tissue perfusion, and elevated serum glucose in the context of an immunocompromised host such as a diabetic patient.1,4 The mixed fermentation process of substrates such as glucose and albumin within the urinary tract by bacteria results in the formation of H2 and CO2 gas both within the urinary tract and within the luminal mucosa.2 In addition, bacterial endotoxin release may contribute to the inflammatory process by inducing paralysis of the urinary tract and thus urinary stasis. In this case, left ureteral stasis resulted in urine reflux into the renal parenchyma with hydroureter and hydronephrosis. Ultimately, this patient required placement of nephrostomy tubes to relieve the functional urinary obstruction.
Both the prevalence and the incidence of the spectrum of Emphysematous urinary tract infections are unknown, but patient demographics are significant for a predilection for middle-aged, diabetic women as was the patient that presented in this report.3 In general, patients with DM have an increased risk of complicated urinary tract infection due to more atypical isolated urinary pathogens which thrive in the presence of an immunocompromised host.5,6 It is likely that the frequency of diagnosis is increasing as the prevalence of DM and use of CT scanning for undifferentiated abdominal pain is also increasing.
The spectrum of presentation of EC is broad; however, it is commonly associated with fever, chills, nausea, emesis, dysuria, and pneumaturia.7,8 Any patient with air in the bladder, not necessarily complicated by an inflammatory process or infection, will require inquiry regarding past surgical history. Both prior urologic procedure, such as cystoscopy, and/or enterovesicular fistula secondary to Diverticulitis or Crohn’s disease are known to cause air in the bladder and bladder wall.
Although the diagnosis of urinary tract infection is made primarily based on patient history and urinalysis results, the diagnosis of EC is made via clinical suspicion and plain films and/or CT scan, which carries high sensitivity for the diagnosis.9 As in this case, the urinalysis was relatively negative and had mild pyuria without bacteriuria lessening concern for urinary tract infection. However, clinical suspicion for a complicated UTI was raised in this diabetic patient with undifferentiated abdominal pain and dysuria who later developed fever and chills. The CT scan will demonstrate presence of air within the bladder lumen and within the bladder wall. In addition, CT can confirm presence alternate sources of intraluminal gas such as an enterovesicular fistula.
Management of EC is correlated with disease severity. As in this case, empiric broad-spectrum intravenous antibiotics to cover gram-negative and anaerobic urinary pathogens was necessary to prevent disease. In rapidly progressive cases of EC, pathogens release endotoxins that create functional obstruction of the urinary tract via ureteral stasis and retrograde flow of urine into the renal parenchyma causing hydroureter and hydronephrosis. As a result, urinary drainage via cystectomy or nephrostomy tube placement may be necessary. Alternatively, there has been a case report of hyperbaric oxygen therapy as an adjunctive measure to the mainstays of antibiotics, urinary drainage, and fluid resuscitation in a case of EC.10
As reported, the mortality rate of EC is 7%, but rapidly progressive forms that result in Emphysematous Pyelonephritis can lead to nephrectomy and carry mortality rates between 19–75%.11,12
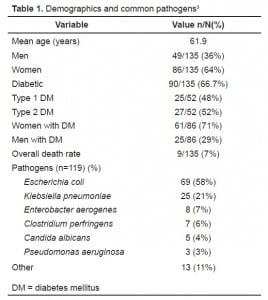
Demographics and common pathogens
CONCLUSION
The rapid progression of EC from a lower urinary tract infection to a complicated upper urinary tract infection warrants recognition of this disease entity by the emergency physician. Prior to the development of EC, an immunocompromised patient with an uncomplicated urinary tract infection may be treated with outpatient oral antibiotics. However, symptoms of abdominal pain or persistent dysuria in immunocompromised patients with a recently-treated, uncomplicated UTI or with a new presentation of symptoms should be worked up as undifferentiated abdominal pain of an unknown origin. The presentation of EC can be insidious and may present as undifferentiated abdominal pain as in this report without initial evidence of urinary tract infection as seen in the screening urinalysis. In susceptible patient populations, such as in diabetic and immunocompromised patients, inclusion of EC in the emergency physician’s differential diagnosis will reduce morbidity and mortality of this disease entity.
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Submission history: Submitted October 31, 2007; Revision Received January 11, 2008; Accepted January 21, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Kapil R. Dhingra, MD, MBA, UC Davis Medical Center, Department of Emergency Medicine, 4150 V Street, PSSB Suite 2100, Sacramento, CA 95817
E-mail: kapil.dhingra@ucdmc.ucdavis.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Bailey H. Cystitis emphysematosa: 19 cases with intraluminal and interstitial collections of gas. Am J Roentgen. 1961;86:850–862.
2. Hawtrey CE, Williams JJ, Schmidt JD. Cystitis emphysematosa. Urology. 1974;3:612–614. [PubMed]
3. Thomas AA, Lane BR, Thomas AZ, Remer EM, Campbell SC, Shoskes DA. EC: a review of 135 cases. BJU International. 2007 Jul;100(1):17–20. [PubMed]
4. Wessells H, McAninch JW. Urological Emergencies: A Practical Guide. 2005. pp. 128–133.
5. Patterson JE, Andriole VT. Bacterial urinary tract infections in diabetes. Infect Dis Clin North Am. 1997;11:735–750. [PubMed]
6. Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002;113(1):5–13. Supplement 1.
7. Mokabberi R, Ravakhah K. Emphysematous Urinary Tract Infections: Diagnosis, Treatment and Survival. Am J Med Sci. 2007;333(2):111–116. [PubMed]
8. Taussig AF. Pneumaturia with report of a case. Boston Med Surg J. 1997;156:769–74.
9. Bohlman ME, Sweren BS, Khazan R. Emphysematous pyelitis and Emphysematous pyelonephritis characterized by computerized tomography. South Med J. 1991;84:1438–43. [PubMed]
10. McCabe JB, Mc-Ginn Merrit W, Olsson D, Wright V, Camporesi EM. EC: rapid resolution of symptoms with hyperbaric treatment: a case report. Undersea Hyperb Med.2004;31:281–4. [PubMed]
11. Huang JJ, Chen KW, Ruaan MK. Mixed acid fermentation of glucose as a mechanism of Emphysematous urinary tract infection. J Urol. 1991 Jul;146(1):148–51. [PubMed]
12. Michaeli J, Mogle P, Perlberg S, et al. Emphysematous pyelonephritis. J Urol. 1984 Feb;131(2):203–8. [PubMed]



