| Author | Affiliation |
|---|---|
| Tetsuji Suzuki, EMT-P, MA | Graduate School of Health Information Science Teikyo Heisei University, Department of Pre-hospital Emergency Medical Care |
| Masamichi Nishida, MD, PhD | Teikyo University, School of Medicine, Emergency Medicine |
| Yuriko Suzuki, RN | Kyoto Kujo Hospital, Department of Nursing |
| Kunio Kobayashi, MD, PhD | Graduate School of Health Information Science Teikyo Heisei University, Department of Pre-hospital Emergency Medical Care |
| S. V. Mahadevan, MD | Stanford University School of Medicine, Division of Emergency Medicine |
ABSTRACT
Introduction:
This report aims to illustrate the history and current status of Japanese emergency medical services (EMS), including development of the specialty and characteristics adapted from the U.S. and European models. In addition, recommendations are made for improvement of the current systems.
Methods:
Government reports and academic papers were reviewed, along with the collective experiences of the authors. Literature searches were performed in PubMed (English) and Ichushi (Japanese), using keywords such as emergency medicine and pre-hospital care. More recent and peer-reviewed articles were given priority in the selection process.
Results:
The pre-hospital care system in Japan has developed as a mixture of U.S. and European systems. Other countries undergoing economic and industrial development similar to Japan may benefit from emulating the Japanese EMS model.
Conclusion:
Japan has the potential to enhance its current pre-hospital care system, but this will require greater collaboration between physicians and paramedics, increased paramedic scope of medical practice, and greater Japanese societal recognition and support of paramedics.
INTRODUCTION
Emergency medical services (EMS) in Japan have developed primarily from emergency transportation services, historically emphasizing transporting patients to the most appropriate medical facility as soon as possible. Although this is an important aspect of EMS, it no longer accurately reflects the current state of pre-hospital care in Japan.
In 1991 Japan officially established national paramedic systems that enabled emergency personnel to work similarly to paramedics in the United States.1 Before this time ambulance personnel were not allowed to use defibrillators Only as recently as April 2006 were Japanese paramedics given permission to administer adrenaline to patients in cardiac arrest.2
Japan is a world leader in communication technology, including standard and cellular telephone services and dispatch systems. This technological advantage, combined with well-organized emergency medical services, has enabled Japanese ambulances to arrive within six minutes of emergency “119” calls (national average in 2006).3 However, the Japanese EMS system as a whole has yet to achieve paramedicsystems maximum success because of various legal restrictions on paramedic scope of practice. This paper introduces the current Japanese system of pre-hospital care and compares it to the systems used in the U.S. and Europe. Adopting effective aspects of Western EMS systems could lead to improved medical care and patient outcomes in Japan.
METHODS
Government and academic publications on the Japanese system of emergency medical services were reviewed. Japanese articles were selected from Ichushi (Japana Centra Revuo Medicina), using keywords such as emergency medicine/care, pre-hospital care, emergency transport systems, and emergency medical response. Government publications, journal articles, and book chapters that were most recent or peer reviewed were prioritized. English articles were selected by searching PubMed, using the same key terms, for study of the U.S., European, and international emergency care and pre-hospital care systems. Again, the most recent or peer reviewed articles were given highest priority.
Measures of improvements are proposed based on the collective experiences and research results of the authors and other relevant researchers.
RESULTS
Japanese Emergency Service System and its History
The existing system for emergency medical services in Japan depends on two distinct entities: the fire department, which is responsible for transporting patients, and the emergency medical system, which is responsible for actual medical care.
Emergency transport service in Japan is mostly performed by the fire department in each local government district/locale. Although not originally a responsibility of the fire department, emergency transport service has been performed by local fire stations since 1986, when it became required by national law.4 As a natural extension, pre-hospital care is considered a major responsibility of local government.
Japanese emergency medical service is based on two national systems: the emergency notification system, which began in 1964, and a supplementary system, which began in 1977. A partial amendment of the Fire Protection Law of 1986 states: “Patients with life threatening conditions and/or with disease that has possibility of severe worsening, and without any method of appropriately transporting [themselves] immediately to places such as medical facilities are the subjects of emergency medical services.” This amendment established and legally acknowledged emergency transport as the responsibility of fire departments in the modern system of emergency medical service in Japan. Of note, this service was intended for transportation, and not for pre-hospital medical care.
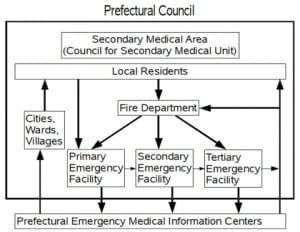
In December 1997, based on the report from the Emergency Medical Service System Basic Problem Commission, the national emergency medical system (Figure 1) was established.5 This system has three layers of service: the primary, secondary, and tertiary emergency medical systems (Table 1). The primary emergency medical system provides what is commonly called primary (or basic) medical care. These medical facilities are often the first point of contact for patients in the system and are responsible for handling relatively mild cases. At the end of 2003, 509 holiday and night-time urgent care centers were operating, and 686 areas with on-call private practitioners were registered.
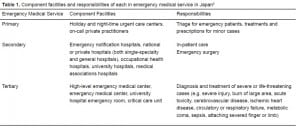
Component facilities and responsibilities of each in emergency medical service in Japan
The secondary emergency medical system is the focus of Japan’s emergency medical services; it provides care to patients who need hospitalization or emergency surgery. Emergency notification hospitals, national or private hospitals (both single-specialty and general hospitals), occupational health hospitals, university hospitals, and medical association hospitals comprise this system. Hospitals in various regions take turns providing such emergency medical services. However, in areas that have adequate medical resources (i.e., Tokyo), certain hospitals are permanently assigned to provide secondary emergency medical services as part of the holiday and night-time medical services of local governments. In areas where hospitals take turns providing secondary emergency medical services, pre-hospital transport times may vary widely based on the hospital’s location, and hospitals with fewer resources may be overwhelmed when they are “on duty.”
The tertiary emergency medical system provides 24-hour care for patients with serious and potentially fatal conditions such as cerebrovascular events, cardiac events, and severe injuries. The highest level of medical care is provided in this system, which is supported by specialists and supervisory physicians of the Japanese Association for Acute Medicine.
In response to the 2000 Ministry of Welfare report on pre-hospital care and rescue commission, emergency medical care centers were positioned as regional centers for pre-hospital care at the local level. They were expected to establish medical control systems and provide local paramedics with instruction, guidance, and post-event evaluations. By November 2004, there were 173 emergency medical care centers throughout Japan, and new small-scale centers called “mini ERs” are planned for each secondary emergency medical system district.6
An important issue that has arisen is the wide variability in quality of care between populous and financially -stable major cities (such as Tokyo) and rural regions. While major cities can meet most of the criteria for establishing emergency departments (EDs) in hospitals, many of the regional hospitals have not yet met official standards. Many hospitals have been forced to quickly establish EDs in response to government calls for increased emergency facilities.7 According to a survey conducted in Fukuoka prefecture, only four of 28 hospitals were certified by the Japanese Association of Acute Medicine, and only nine had certified acute care physicians.8 Fukuoka has a population of 1.32 million (2005) and is considered one of Japan’s large cities; however, the staffing in its hospitals was found to be inadequate. The researchers who conducted this study concluded that many Japanese EDs were seriously understaffed, even in large cities.
Another fundamental issue is the absolute shortage of both medical personnel and available hospital beds. Ambulances may travel long distances (mean transport time in 2006 was 57 minutes9) to reach an appropriate or designated hospital but may not find a readily available hospital bed. In 2007 two similar incidents in the Nara prefecture captured national attention because ambulances transporting pregnant women in critical condition were unable to find hospital EDs with available beds and qualified physicians. 10,11 These incidents prompted improvement in communication between local hospitals and emergency dispatchers, and led to increases in hospital staff with obstetric-specific training.12
The Role and Issues of Paramedics in Japan
In 1991 Japan officially established the role of the paramedic and enacted related regulations, designating its workers as medical professionals and establishing that emergency medical services encompasses both medical care at the scene and transport to medical facilities.1 Paramedics are nationally licensed, not as part of the certification within fire departments, but as a new medical profession in its own right.
The U.S. has highly trained paramedics that provide high-level emergency medical care. One difference between paramedics in the U.S. and Japan is the amount of training required. In the U.S. the classification, Emergency Medical Technician (EMT)-Paramedic, indicates that the individual has taken approximately 1200 hours of required coursework and training.13 The EMT-Paramedic National Standard Curriculum recommends 500–600 hours of classroom/practical laboratory, 250–300 hours of clinical training, and 250–300 hours of field internship.14 In Japan, most paramedics have a firefighter background. The paramedic job requirements include a minimum of five years of employment as ambulance personnel, approximately 509 hours of lecture, and 406 hours of hospital training or simulation in a designated training facility. This represents a total of approximately 915 hours of training; however, on-the-job training with currently certified paramedics is not required.15 In addition, there is no system for relicensing or renewal in Japan, and continuing education is up to each individual.
Another difference between the U.S. and Japanese paramedic profession is that most Japanese paramedics belong to the department as public civil servants and only a minority work as paramedics for private entities. U.S. paramedics may be either civil servants or private citizens. Patients in the U.S. are responsible for the costs associated with pre-hospital care, which forms much of the business of emergency medical services. Calling for an ambulance for minor conditions or when transportation to the hospital is unavailable occurs routinely in Japan but infrequently in the U.S.
Doctor Car Service
France utilizes a different EMS system in which traditionally hospital-based medical providers such as physicians may provide care outside of the hospital.16 The French system, called “SAMU,” evolved because French physicians felt they were most qualified to perform resuscitation procedures in the pre-hospital setting. Pre-hospital medical professionals, including physicians, initiate medical care at the site of the incident. The system is nationally organized by the Ministry of Health of the French government. Although commonly referred to as a “Doctor Car,” the arriving medical team may not include a physician, especially for cases deemed not life-threatening. This system is independent of the fire safety service and emphasizes the independence of EMS. France, Germany, and Italy have the most established system of sending doctors in ambulances.17
In April 1991 the Japanese Lower House Social and Labor Commission Conference Minutes emphasized the introduction of “European styles of paramedic systems that routinely send physicians to the site of incident,” and encouraged the evaluation of a SAMU-like system.16 In Japan, doctor cars can operate in three different ways. The first is the “docking method,” which is used in the Aizu and Osaka Emergency and Life-Support Centers.18 When an emergency call is received, an ambulance is dispatched from the fire department and a doctor car is dispatched from a hospital; the two meet on the way to arrive together at the event site. The second is the “rendezvous method,” in which the two arrive separately at the event site. The last method is the “Funabashi System,” which was adopted by the city of Funabashi and permanently stations a doctor car in the fire house through the support of the local medical association. As an extension to this doctor car service, the Congresses passed the helicopter service law in June 2007, as a result of the success of introducing helicopters in nine base hospitals throughout Japan. The law was passed partly in response to the current shortage of physicians, especially in rural areas.16
Supporting Others in the Process of Development
Although the Japanese system is still evolving, not having yet achieved maximal efficiency or quality of care, Japan has been a leader in assisting other nations with the process of developing their emergency medical systems. One of the most notable efforts has been in Vietnam, where the Japan International Cooperation Agency has provided cars for use as ambulances as well as other emergency equipment since 1994.19 Because of increases in the number of victims from road traffic accidents in major Vietnamese cities, the lack of an adequate EMS system has became a serious issue. Japan has experienced similar issues in its process of economic and industrial development. Japanese emergency care professionals are assisting the Vietnamese in strengthening their “115” system and are encouraging the development of Vietnamese emergency care professionals.
DISCUSSION
For pre-hospital medical care in Japan to advance, there needs to be increased cooperation and communication between paramedics and physicians, support for an increased scope of practice for paramedics and increased societal support for the emergency medical healthcare workers.
Efforts made by Nara prefecture in assigning trained dispatchers to facilitate communication between hospitals and ambulances may enable a change in the system in increasing efficiency. Also, appointing a permanent facility to provide emergency medical system services would increase the experience levels of healthcare workers. From the perspective of specific facilities and staffing levels, national or public hospitals are the best choices as permanent facilities. The challenge that needs to be overcome is administrative, political and cultural resistance to such a change.5
One of the methods considered as collaboration between physicians and paramedics is to delegate more procedures to trained paramedics. The more advanced skills and role of U.S. paramedics have evolved from the idea that physicians and other medical professionals consider it better to delegate routine jobs to other health professionals who have received the necessary training and who specialize in such services.20 However, delegating what have traditionally been doctors’ jobs is culturally at odds with many Japanese professionals, who feel that the idea of delegation intrudes into another professional’s work. Such acts are considered as lacking respect for other professions. Despite such a background, modern Japanese society has embraced other Western technologies and cultures. This issue could be solved with time as other new ideas gradually became accepted in Japan.
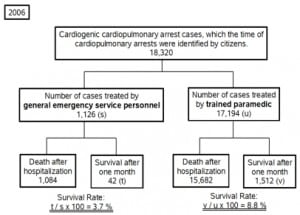
Despite the new laws and regulations, the current status of the Japanese paramedic remains far from that of paramedics in the U.S. and Europe, who enjoy respect and social recognition and who can proactively perform medical procedures at event sites. U.S. and European systems are based on the concept that emergency medicine begins at the site of the accident or event. It is evident that trained paramedics who can perform more procedures on site contribute to better survival of patients compared with patient survival when emergency service personnel have only minimal or basic training. In a report by the Ministry of Internal Affairs and Communications, the survival rate after one month of cases of cardiopulmonary arrest reported by citizens was double when patients were treated by trained paramedics versus by general emergency service personnel (Figure 2).21
Bringing about change in the Japanese system to give paramedics more authority and training is largely a political issue and will require collaboration among the Japanese Medical Association, the Ministry of Health, Welfare, and Labor, and the Japanese Society for Emergency Medicine (JSEM). These groups have made initial efforts, with the JSEM in its 2003 annual symposium proposing to remove the restriction on paramedics that prohibits them from performing procedures only after an ambulance has arrived for patient transport. Hopes are high that with increased societal recognition and patient awareness, paramedics can have a larger role in emergency patient care and can be a more active medical profession.
To solve political and regulatory issues, members of the healthcare professions must gain public support. Healthcare professionals in emergency medicine and pre-hospital care have to inform the governments or community about what is needed – including increases in the number of staff and other resources, such as beds and more facility spaces. Traditionally, Japanese healthcare professionals have not been vocal in asking for their needs to be filled, since they are considered helping-professionals and therefore not the ones to ask for help. But to garner societal support both emergency medical doctors and paramedics should raise the issues that they face, despite the cultural hesitations to do so.
Therefore, we would like to recommend: 1) More collaboration and cooperation between physicians and paramedics, because better results can be expected from delegating specific jobs to appropriately trained professionals. 2) Advocacy and increased recognition for the role of Japanese paramedics to provide greater support in establishing and expanding their role and training to achieve the level of paramedics in the U.S. 3) Increased societal support for emergency medical personnel and their work, needed to address the inadequate number of physicians, hospital beds, and communication professionals.
CONCLUSION
Japan has the technology to support an advanced emergency dispatch system, and doctors and paramedics are capable of performing necessary procedures. Currently, there are two methods operating in Japan: one similar to the U.S. system, in which trained paramedics arrive at site, and another similar to the European model, in which medical doctors arrive at site. However, Japanese paramedics have not yet achieved the level of ability and recognition of their U.S. and European counterparts. Other related issues of emergency medicine in Japan include shortages of emergency medical care professionals and hospital beds. The solution must address both political and cultural aspects; however, information and advocacy from medical professionals may be able to improve the situation. Future improvements lie in greater collaboration between physicians and paramedics, along with greater societal support and recognition of the paramedic profession.
Footnotes
Supervising Section Editor: Chris Mills, MD
Submission history: Submitted November 8, 2007; Revision Received March 12, 2008; Accepted March 15, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Tetsuji Suzuki, EMT-P, MA, Dept of Pre-hospital Emergency Medical Care, Graduate School of Health Information Science, Teikyo Heisei University, 2-51-4 Higashi-Ikebukuro, Toshima-ku, Tokyo 170-8445 Japan
Email: cpr119@coral.ocn.ne.jp
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Tanigawa K, et al. Emergency medical service systems in Japan: Past, present, and future. Resuscitation. 2006;69:365–370. [PubMed]
2. Fire Disaster Management Agency. [Accessed February 26, 2008];2007 White Paper.Available at: http://www.fdma.go.jp/html/hakusho/h18/h18/html/id100000.html.
3. Department of Fire Safety. 2006 Outline of Emergency Services. 2007. Ministry of Internal Affaires and Communications.
4. Harita T, et al. A discussion for emergency transportation system, Byouin Kanri (Hospital Management) J Japan Hosp Manag Assoc. 2001;39:25.
5. Kondo S. Emergency Medical System. In: Yamamoto Y, editor. The Multiple Approaches for Emergency Medicine – Theory and Application. Japan: Medical Journal Co. Ltd.; 2003.
6. Abe Y, et al. Shinryou to chiryou/kyukyuiryou (Care and Treatment/Emergency Medicine) 2003;91 extra number issue.
7. Ezaki T, et al. Current status of Japanese emergency medicine based on a cross-sectional survey of one prefecture. Emergency Medicine Australasia. 2007;19:523–527.[PubMed]
8. Ezaki T, et al. Emergency medicine in Japan: A look at a current university hospital and the problems faced. Emergency Medicine Australasia. 2007;19:296–299. [PubMed]
9. Miwa M, et al. The effect of the development of an emergency transfer system on the travel time to tertiary care centres in Japan. Intl J Health Geograph. 2006;5:25.
10. Chunichi shinbun; May 24, 2007.
11. Mainichi Shinbun; August 27, 2007.
12. Outline of Nara Prefecture Board Meeting of Survey on Issues in August 2007 Emergency Transportation of Pregnant Women Incident. Prefecture of Nara; October 5, 2007.
13. Suzuki T. The Mission and Reality of Private Paramedic. Japan: Chigensha; 2004.
14. US Department of Transportation, National Highway Traffic Safety. EMT Paramedic National Standard Curriculum.
15. Shigeta M, Maeda K. Kyukyutaiin. Kyukyu kyumeishi kyoiku (ambulance crew and paramedic education) Rinsho to Kyoiku (Clinical Activities and Education) 2000:77.
16. Morimura H. (Dispatching emergency crew to the site of incident – French System of supporting out of hospital emergency medical care, SAMU) Japan Traffic and Welfare Association, Asuka. 2002;21:44.
17. Mashiko K. Trauma system in Japan: History, present status and future perspectives.J Nippon Med Sch. 2005;72:194–202. [PubMed]
18. Hirama H. Kyukyuigaku (Emergency Medicine) Japan: Herusu Publishing; 1997. Investigation on docking method doctor car system in Aizu General Hospital.
19. Department of Fire Safety, Ministry of Internal Affaires and Communication. Effects on survival results from emergency medical procedures under various circumstances.Japan: 2007.
20. Fleischmann T, et al. Emergency medicine in modern Europe. Emergency Medicine Australasia. 2007;19:300–302. [PubMed]
21. Kuroiwa Y. Kyukyu iryou ni mess (Dissecting Emergency Medicine) Information Center Publishing Division. 1990