| Author | Affiliation |
|---|---|
| Matthew Silver, MD | Kaiser Permanente, San Diego Medical Center, Department of Emergency Medicine, San Diego, California |
| Steven Kohler, MD | Kaiser Permanente, San Diego Medical Center, Department of Emergency Medicine, San Diego, California |
A previously healthy 14-year-old male presented to the emergency department (ED) complaining of 2 days of subacute onset, right-anterior pleuritic chest pain. He reported an associated dry cough, but denied fever, sputum, hemoptysis, shortness of breath, orthopnea, leg swelling, weight loss or night sweats. The patient had no known sick contacts, and had no identifiable cardiac or thromboembolic risk factors. We obtained a 2-view chest radiograph, which revealed an indeterminate 1.3 cm focal density in the right upper lobe (Figure 1). The patient was discharged on oral analgesics with a plan for follow-up imaging.
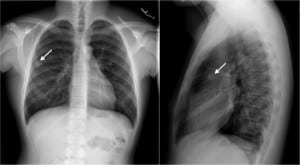
Anterior-Posterior chest radiograph on index visit showing a 1.3 cm right upper lobe density (arrows).
Six days after symptom onset the patient returned to the ED with worsening pain despite oral analgesics, a low-grade fever and a worsening dry cough. On physical examination the patient was well appearing and in no apparent distress. His temperature was 99.8 °F; his blood pressure was 105/72; his heart rate was 95 beats/minute; and his oxygen saturation on room air was 99%. A previously planted PPD was read as negative. We obtained a repeat chest radiograph, which revealed a wedge-shaped consolidation in the inferior segment of the right upper lobe (Figure 2). The patient was treated with an oral cephalosporin as an outpatient with complete resolution of his symptoms.
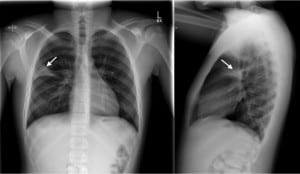
Anterior-Posterior chest radiograph on day 6 showing consolidation of the inferior segment of the right upper lobe (arrows).
Round pneumonia is primarily seen in children and adolescents. In one study, 75% of patients were under 8 years of age, and 90% under 12.1 It is postulated that round pneumonias occurs more often in children as they have poorly developed pathways of collateral ventilation, more closely apposed lung connective tissue septa and smaller alveoli, when compared to adults. These factors combine to form more compact areas of infiltrate, which can appear as round lesions on chest radiography.2Round pneumonias are most often caused by Streptococcus pneumoniae, and resolution after treatment, rather than progression to lobar pneumonia, is the rule.1,3 In addition to infection, the differential diagnosis of a round lesion on a pediatric chest radiograph includes primary lung neoplasm, congenital bronchogenic consolidation, and Wilms tumor.2 The majority of round lesions in children, however, are nonneoplastic, and advanced imaging with computed tomography or magnetic resonance imaging is not typically indicated unless symptoms suggest an alternative diagnosis.4
Footnotes
Address for Correspondence: Matthew Silver, MD, Kaiser Permanente San Diego Medical Center, Department of Emergency Medicine, 4647 Zion Avenue, San Diego, CA 92120., Email: matthew.a.silver@kp.org. 11 / 2013; 14:643 – 644
Submission history: Revision received July 12, 2013; Accepted July 15, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Kim YW, Donnelly LF Round pneumonia: imaging findings in a large series of children. Pediatr Radiol. 2007; 37:1235-1240
2. McLennan MK Clinical Challenge: Radiology Rounds. Can Fam Phys. 1998; 44:757-759
3. Franquet T Imaging of Pneumonia: Trends and Algorithms. Euro Rad J. 2001; 18:196-208
4. Camargos PA, Ferreira CS On Round Pneumonia in Children. Pediatr Pulmonol. 1995; 20:194-195


