| Author | Affiliation |
|---|---|
| Jana L. Anderson, MD | Mayo Clinic, Department of Emergency Medicine, Rochester, Minnesota |
| Kharmene Sunga, MD | Mayo Clinic, Department of Emergency Medicine, Rochester, Minnesota |
| Annie Sadosty, MD | Mayo Clinic, Department of Emergency Medicine, Rochester, Minnesota |
A 68-day-old former 30-week infant presented with listlessness, apnea and bradycardia. The patient was intubated for airway protection. After intubation, breath sounds were auscultated bilaterally and a Pedi-Cap carbon dioxide detector had color change from purple to yellow. A nasogastric tube (NGT) was placed and a post-procedural chest radiograph was obtained (Figure).
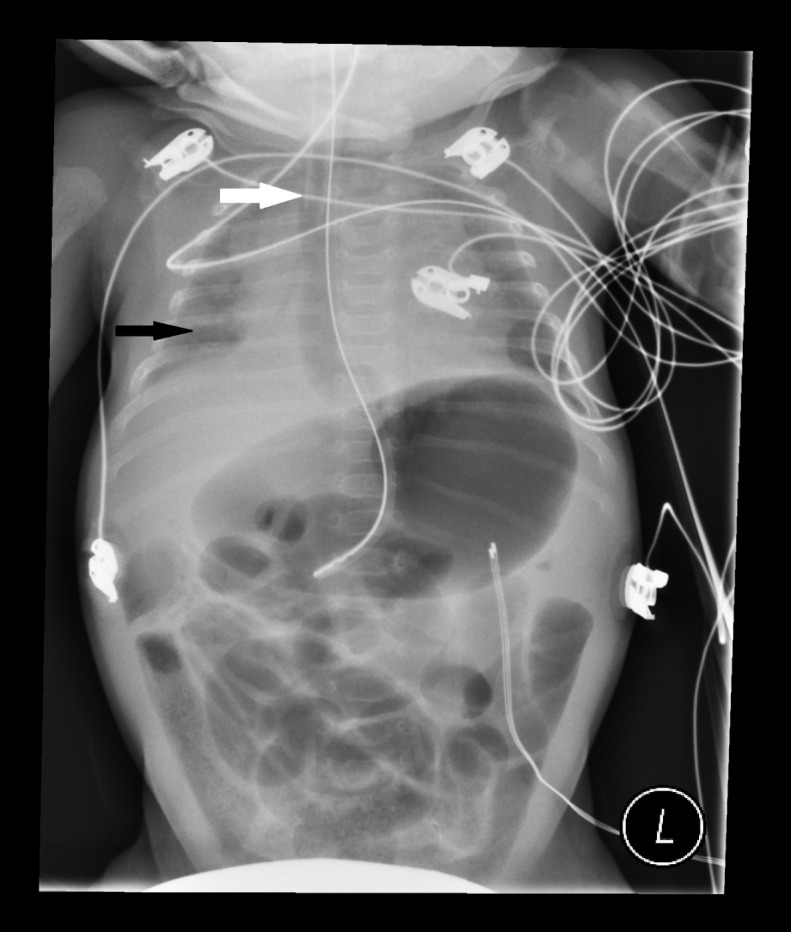
There are several features of esophageal intubation: low lung volumes, esophageal and gastric distention despite NGT placement and juxtaposition of the endotracheal tube (ETT) relative to the NGT.1-2 Other findings of esophageal intubation not seen here are identification of the ETT distal to the carina or outside of the tracheal-bronchial air column.3 Due to high success rates of endotracheal intubation in the emergency department,4-5 these findings are rare and may be overlooked. In this case, misleading clinical evidence was obtained through auscultation of bilateral breath sounds, visualization of endotracheal tube condensation, positive change on the carbon dioxide colorimeter and post-procedural hemodynamic and oxygenation stability. Previous literature, however, has demonstrated false-positive colorimetric change from swallowed air with pre-intubation positive pressure ventilation,6-7 hence the importance of radiographic identification of ETT location. In this patient, esophageal intubation was recognized after continuous capnography revealed absence of waveform.
Footnotes
Section Editor: Sean O. Henderson, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Jana L. Anderson, MD, Mayo Clinic, Department of Emergency Medicine, 200 1st SW, Rochester, MN 55905. Email: anderson.jana@mayo.edu. 7 / 2015; 16:575 – 576
Submission history: Revision received February 26, 2015; Accepted April 6, 2015
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Bagshaw O, Gillis J, Schell D. Delayed recognition of esophageal intubation in a neonate: role of radiologic diagnosis. Crit Care Med. 1994;22(12):2020-2023.
2. Dittrich KC. Delayed recognition of esophageal intubation. CJEM. 2002;4(1):41-44.
3. Salem MR, Baraka AS. Confirmation of endotracheal intubation. Benumof and Hagberg’s Airway Management. 2013:657-682.
4. Sagarin MJ, Barton ED, Chng YM, et al. Airway management by US and Canadian emergency medicine residents: a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med. 2005;46(4):328-336.
5. Walls RM, Brown CA, Bair AE, et al. Emergency airway management: a multi-center report of 8937 emergency department intubations. J Emerg Med. 2011;41(4):347-354.
6. Gomes SB, Mychaskiw G. Failure of the Easy Cap II CO2 detector to indicate esophageal intubation. J Clin Anesth. 2012;24(4):352-353.
7. Hughes SM, Blake BL, Woods SL, et al. False-positive results on colorimetric carbon dioxide analysis in neonatal resuscitation: potential for serious patient harm. J Perinatol. 2007;27(12):800-801.


