Archives
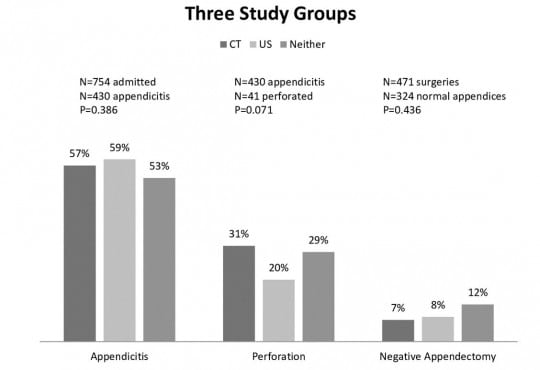
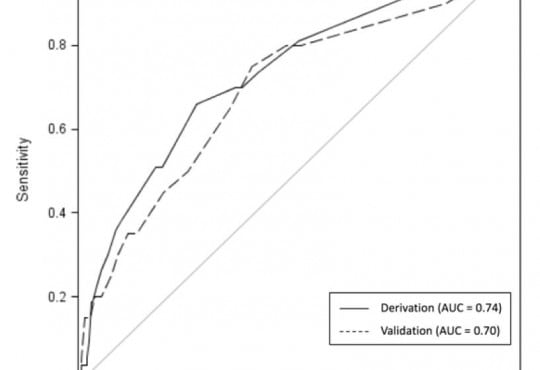
Treatment Protocol Assessment
Abdominal CT Does Not Improve Outcome for Children with Suspected Acute Appendicitis
Westjem Read More
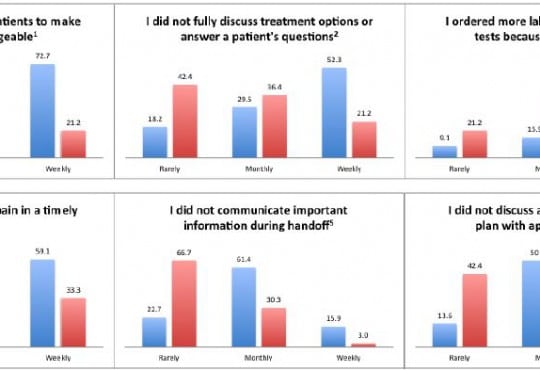
Healthcare Utilization
Achieving the Triple Aim Through Informed Consent for Computed Tomography
Westjem Read More
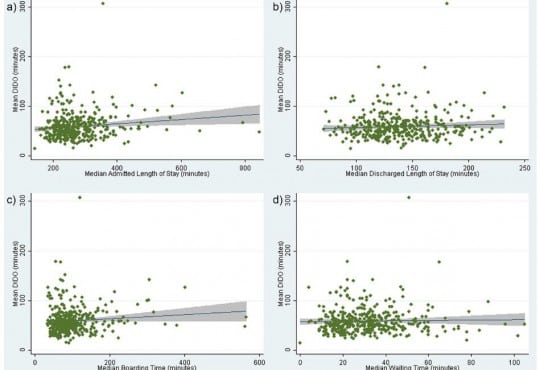
Societal Impact on Emergency Care
The Changing Use of Intravenous Opioids in an Emergency Department
Westjem Read More
Societal Impact on Emergency Care
Transformative Leadership: Emergency Physicians Lead AOA and AMA
Westjem Read More
Patient Communication