| Author | Affiliation |
|---|---|
| Dave W. Lu, MD, MBE | Northwestern University Feinberg School of Medicine, Department of Emergency Medicine, Chicago, Illinois |
| Scott Dresden, MD, MS | Northwestern University Feinberg School of Medicine, Department of Emergency Medicine, Chicago, Illinois |
| Colin McCloskey, MD | Northwestern University Feinberg School of Medicine, Department of Emergency Medicine, Chicago, Illinois |
| Jeremy Branzetti, MD | University of Washington School of Medicine, Department of Emergency Medicine, Seattle, Washington |
| Michael A. Gisondi, MD | Northwestern University Feinberg School of Medicine, Department of Emergency Medicine, Chicago, Illinois |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Burnout is a syndrome of depersonalization, emotional exhaustion and sense of low personal accomplishment. Emergency physicians (EPs) experience the highest levels of burnout among all physicians. Burnout is associated with greater rates of self-reported suboptimal care among surgeons and internists. The association between burnout and suboptimal care among EPs is unknown. The objective of the study was to evaluate burnout rates among attending and resident EPs and examine their relationship with self-reported patient care practices.
Methods
In this cross-sectional study burnout was measured at two university-based emergency medicine residency programs with the Maslach Burnout Inventory. We also measured depression, quality of life (QOL) and career satisfaction using validated questionnaires. Six items assessed suboptimal care and the frequency with which they were performed.
Results
We included 77 out of 155 (49.7%) responses. The EP burnout rate was 57.1%, with no difference between attending and resident physicians. Residents were more likely to screen positive for depression (47.8% vs 18.5%, p=0.012) and report lower QOL scores (6.7 vs 7.4 out of 10, p=0.036) than attendings. Attendings and residents reported similar rates of career satisfaction (85.2% vs 87.0%, p=0.744). Burnout was associated with a positive screen for depression (38.6% vs 12.1%, p=0.011) and lower career satisfaction (77.3% vs 97.0%, p=0.02). EPs with high burnout were significantly more likely to report performing all six acts of suboptimal care.
Conclusion
A majority of EPs demonstrated high burnout. EP burnout was significantly associated with higher frequencies of self-reported suboptimal care. Future efforts to determine if provider burnout is associated with negative changes in actual patient care are necessary.
INTRODUCTION
Burnout is a triad of emotional exhaustion, depersonalization and reduced sense of personal accomplishment that produces decreased effectiveness at work.1 Physician burnout is widespread, with almost half of all physicians reporting high levels of burnout.2 Among all specialties, emergency medicine (EM) experiences the highest levels of physician burnout at over 60%.2,3
High levels of burnout may negatively impact the quality of care physicians provide to patients. Prior work in select medical specialties suggests that burnout is associated with self-reported medical error (e.g., medication errors) and suboptimal care (e.g., failure to adhere to practice standards, lower patient satisfaction).4-14 Burnout may also contribute to job turnover, absenteeism, low morale, and deterioration of provider health.3,15-26 Although emergency physicians (EPs) report some of the highest levels of burnout, to our knowledge the relationship between EP burnout and patient care has not been studied. Our study evaluated rates of burnout among attending and resident EPs and examined the relationship between their levels of burnout and self-reported patient care practices.
METHODS
Study Design
A cross-sectional survey of EPs measured provider levels of burnout and self-reported rates of suboptimal care.
Study Setting and Population
All attending and post-graduate year (PGY) 2–4 resident EPs, except the study authors, at two university-based PGY 1–4 training programs were eligible for this study conducted in September 2013. PGY-1 residents were excluded from the study because the survey asked respondents to rate their perception of patient care over the past year, and PGY-1 residents at the time of the study had only been in their positions for three months.
Study Protocol
An anonymous electronic survey was emailed to all eligible subjects. The invitation did not mention burnout, depression, or suboptimal care and subjects were blinded to any specific hypothesis of the study. Subjects consented to the voluntary study by completing the anonymous survey on an online and secure platform (REDCap). Up to two reminder emails were sent to non-responders. The human subjects review boards at both institutions approved the study.
Measurements
The survey included 39 items taken from previously described instruments on provider burnout, depression, and suboptimal care. Burnout was measured through the Maslach Burnout Inventory (MBI), a 22-item questionnaire that is a standard tool for measuring burnout.1,27 The MBI evaluates the three dimensions of burnout: depersonalization, emotional exhaustion, and sense of low personal accomplishment. Consistent with prior work, burnout was defined by high scores in the depersonalization or emotional exhaustion subscales of the inventory.27 In addition to burnout and depression, we evaluated quality of life (QOL) and career satisfaction. Provider depression was screened using the first two items of the Primary Care Evaluation of Mental Disorders instrument.28 A “yes” response to either question was considered a positive screen for depression. We measured QOL by a single-item linear analog scale assessment: “How would you rate your overall quality of life over the past week?”29 We assessed career satisfaction by a single-question: “If given the opportunity to revisit your career choice, would you choose to become a physician again?”30 Responses of “likely” and “very likely” on a 5-point Likert scale were categorized as positive for career satisfaction.
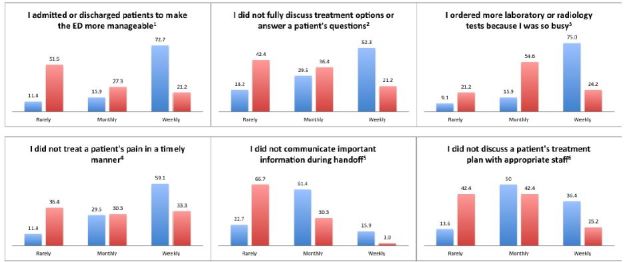
We measured suboptimal care with a series of six statements adapted from prior work that investigated self-reported patient care among internal medicine resident physicians.8 A group of board-certified EPs modified the statements to present EM-focused patient care practices that are common, relevant and important to a practicing EP. The six statements were (1) “I admitted or discharged patients to make the emergency department (ED) more manageable;” (2) “I did not fully discuss treatment options or answer a patient’s questions;” (3) “I ordered more laboratory or radiology tests because I was so busy;” (4) “I did not treat a patient’s pain in a timely manner;” (5) “I did not communicate important information during handoff to an ED colleague or admitting service;” and (6) “I did not discuss a patient’s treatment plan with the patient’s appropriate nursing or ancillary staff.” EPs were asked if they performed these acts of suboptimal care rarely, monthly or weekly over the past year.
To encourage study participation and honest reporting, we collected limited demographic information (Table 1) so that subject responses could not be easily identified. We did not obtain information regarding the subject’s work or training institution.
| N (77) | % | |
|---|---|---|
| Female | 29 | 37.7 |
| Attendings | 54 | 70.1 |
| Years in practice | ||
| <1 yr | 8 | 10.4 |
| 1–4 yr | 13 | 16.8 |
| 5–10 yr | 17 | 22.1 |
| 11–20 yr | 8 | 10.4 |
| 21+ yr | 8 | 10.4 |
| Residents | 23 | 29.9 |
| Post-graduate year | ||
| 2 | 7 | 9.1 |
| 3 | 7 | 9.1 |
| 4 | 9 | 11.7 |
| % effort to clinical practice (attendings) | ||
| 0–25% | 0 | 0 |
| 26–50% | 12 | 22.2 |
| 51–75% | 19 | 35.2 |
| 76–100% | 23 | 42.6 |
| Primary practice site setting (attendings) | ||
| Academic | 47 | 87.0 |
| Community | 7 | 13.0 |
| Primary practice site annual patient volume | ||
| <25,000 | 0 | 0 |
| 25,001–50,000 | 8 | 10.4 |
| 50,001–75,000 | 24 | 31.1 |
| 75,001–100,000 | 35 | 45.5 |
| >100,000 | 10 | 13.0 |
Data Analysis
We categorized burnout data as described above, and burnout was dichotomized and defined as meeting the MBI criteria of high emotional exhaustion or high depersonalization.27 Burnout, depression, career satisfaction, QOL, and rates of self-reported suboptimal care were compared to career stage (resident versus attending). We then compared burnout to depression, career satisfaction, and self-reported suboptimal care. Comparisons were made using Fischer’s exact test for categorical variables, and Student’s t-test was used for continuous variables. We performed data analysis using STATA version 13 (College Station, TX).
RESULTS
A total of 91 out of 155 (58.7%) subjects responded to the survey with 77 completed responses included in the analyses (49.7%). Respondents were primarily attending EPs at a university hospital (61.0%), followed by residents (29.9%), and attending EPs at a community hospital (9.1%) (Table 1). EPs reported a burnout rate of 57.1%, with no statistically significant difference between attending and resident physicians. Residents, however, were more likely to report higher scores on the depersonalization subscale than attendings (73.9% vs 38.9%, p=0.011). There were no associations between burnout and gender and year in practice or training. Residents were more likely to screen positive for depression (47.8% vs 18.5%, p=0.012) and report lower QOL scores (6.7 vs 7.4 out of 10, p=0.036) than attendings (Table 2). Attendings and residents reported similar rates of career satisfaction (85.2% vs 87.0%, p=0.744). EP burnout was significantly associated with a positive screen for depression (38.6% vs 12.1%, p=0.011) and lower career satisfaction (77.3% vs 97.0%, p=0.02) (Table 3).
| Attending (%) | Resident (%) | Total (%) | |
|---|---|---|---|
| Burnout | 27 (50.0) | 17 (73.9) | 44 (57.1) |
| EE Median (IQR) | 20 (12–26) | 20 (13–24) | 20 (13–26) |
| Low | 21 (38.9) | 7 (30.4) | 28 (36.3) |
| Intermediate | 21 (38.9) | 12 (52.2) | 33 (42.9) |
| High | 12 (22.2) | 4 (17.4) | 16 (20.8) |
| DP Median (IQR) | 10 (7–14) | 17 (12–21) | 12 (7–19) |
| Low | 13 (24.1) | 4 (17.4) | 17 (22.1) |
| Intermediate | 20 (37.0) | 2 (8.7) | 22 (28.5) |
| High | 21 (38.9)* | 17 (73.9)* | 38 (49.4) |
| PA Median (IQR) | 41 (37–44) | 43 (41–44) | 42 (38–44) |
| Low | 6 (11.1) | 0 (0) | 6 (7.8) |
| Intermediate | 13 (24.1) | 4 (17.4) | 17 (22.1) |
| High | 35 (64.8) | 19 (82.6) | 54 (70.1) |
| Depression | 10 (18.5)^ | 11 (47.8)^ | 21 (27.3) |
| Career satisfaction | 46 (85.2) | 20 (87.0) | 66 (85.7) |
| Quality of life (median, IQR) | 7.4 (6.4–8.1)# | 6.7 (5.8–7.3)# | 7.2 (6.1–8.0) |
Maslach Burnout Inventory subscales: EE, emotional exhaustion; DP, depersonalization; PA, personal accomplishment *p=0.011. ^p=0.012. #p=0.036.
| Depression | Career satisfaction | |
|---|---|---|
| Burnout | ||
| Yes (%) | 17 (38.6) | 34 (77.3) |
| No (%) | 4 (12.1) | 32 (97.0) |
| p=0.011 | p=0.020 | |
EPs with high levels of burnout were significantly more likely to report performing suboptimal care practices with greater frequency in all six domains (Figure 1): (1) admitting or discharging patients early (p<0.001); (2) not discussing options or answering questions (p=0.012); (3) ordering more tests (p<0.001); (4) not treating patients’ pain (p=0.019); (5) not communicating important handoffs (p<0.001); and (6) not discussing plans with staff (p=0.009). There were no significant associations between rates of suboptimal care and depression, QOL or career satisfaction.
DISCUSSION
To our knowledge this is the first study to examine the relationship between physician burnout and patient care practices in emergency medicine. Burned-out EPs were more likely to report performing on a more frequent basis all of our queried suboptimal patient care practices. Most prior studies on improving patient safety and quality in emergency medicine have focused on system-level issues rather than individual-level factors.31,32 Our results suggest that addressing physician factors such as emotional distress and burnout may be important in efforts to improve patient care.
Burnout was common among EPs, with 57% of attending and resident physicians experiencing burnout, a figure that is consistent with studies dating back to 1996.3,24,33 Our study showed no significant difference in levels of burnout between attending and resident EPs. This is similar to a prior study of EPs, which demonstrated that PGY 2–4 residents exhibited burnout rates comparable to those of attending physicians (49–64% vs 60%).3 Our findings demonstrate that at least half of EPs suffer from burnout in as early as the second year of residency training. We did not expect burnout rates among attending EPs to be significantly different than those noted in prior studies, since to our knowledge no large organized effort has been made to improve the working conditions of practicing EPs. However, despite efforts to improve resident working conditions, including work hour restrictions, resident burnout has not changed over the last two decades.33,34
Although our study did not investigate specific causes of EP burnout, previous studies may provide insights into possible explanations for the high rate of EP burnout. Emergency medicine is challenging physically and emotionally.35 An unpredictable workload, frequent disruptions to circadian rhythms, and caring for high acuity and high complexity patients in a high stakes environment all potentially contribute to burnout. A national survey of physicians across all specialties found that burnout was highest not just in EM but also in other “front line” disciplines such as general internal medicine and family medicine.2 Our results suggest that resident physicians in as early as the PGY-2 level may suffer high levels of burnout similar to those of attending physicians. This may be the result of their socialization in the “hidden curriculum,” a phenomenon in which physicians in training acquire and model the attitudes and habits of other physicians.36,37 In this sense direct interaction and long hours spent with burned-out EPs may lead to a “contagious” spread of burnout to trainees.
Resident physicians in our study were significantly more likely to report high scores in the depersonalization subscale of the MBI than attending physicians. This is consistent with prior work among residents and attendings across multiple specialties.38 Depersonalization is characterized by negative, cynical and dehumanized attitudes and feelings about patients.39 We suspect EM residents may experience higher rates of depersonalization due to the fact they on average work more clinical hours than EM attendings at the two sampled academic training sites. In addition resident physicians at these sites are charged with the role of interfacing primarily with admitting services, consultants and ancillary staff to a greater extent than attending physicians. As such resident physicians may experience greater exposure to negative, cynical or dehumanized attitudes about patients.
Our results showed that a positive screen for depression was significantly associated with higher rates of burnout. Burnout is related to depression, although the two are not synonymous.40,41 Whereas depression affects an individual globally, burnout is specifically related to one’s work. While research on rates of depression among EM residents is limited, our rates of depression among attending physicians are comparable to those in prior studies of EPs.42-44 Our rates of career satisfaction among EPs were also similar to those reported in previous work,45,46 as was our study’s demonstrated significant association between burnout and low career satisfaction.3,33 Interestingly, we did not find significant relationships between suboptimal care and EP rates of depression, QOL or career satisfaction. Although related studies showed associations between various aspects of provider wellness (e.g. burnout, depression, QOL) and physician self-reported medical error,4-6 only burnout demonstrated a significant relationship with suboptimal care in a similar study of internal medicine trainees.8 We theorize that burnout may be a unique and pervasive condition that not only adversely impacts the occurrence of discrete and perhaps more salient medical errors but also the less apparent aspects of quality care (e.g. empathy, professionalism) that physicians provide to patients.
LIMITATIONS
Our subject population was a convenience sample of EM attending and resident physicians at two academic programs. As such, our results may not be generalizable to EPs in non-academic settings. Approximately 50% of eligible subjects were included in the final analysis, which could allow for response bias. We were unable to compare characteristics of respondents with non-respondents due to the anonymous nature of the survey methodology. Specifically we do not know if non-respondents suffered higher levels of burnout, for example, and therefore did not choose to participate in the study. Still, our rates of burnout are consistent with those reported in prior studies of both academic and non-academic EPs.2,3,24,33 Although our questions measuring self-reported suboptimal care were modeled after prior work8 and have face validity, their criterion and construct validity as well as reliability have not been examined. In addition we are unable to ascertain if these self-reported frequencies of suboptimal care translate into actual practice. It also remains unclear if burned-out EPs report higher rates of suboptimal care as a result of their higher levels of burnout.5,6 Despite these limitations, our results are consistent with prior work in other specialties demonstrating that provider wellness, one aspect of which is professional burnout, may significantly impact the quality of care received by patients.4-8,12,13,47-50
CONCLUSION
A majority of EPs reported high levels of burnout. EP burnout was also significantly associated with higher frequencies of self-reported suboptimal care. Future efforts to determine if provider burnout is associated with negative changes in actual patient care are necessary.
Footnotes
Section Editor: Kenneth S. Whitlow, DO
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Dave W. Lu, MD, MBE, Northwestern University Feinberg School of Medicine, Department of Emergency Medicine, 211 E. Ontario Street, Suite 200 Chicago, IL 60611. Email: dave.lu@northwestern.edu. 12 / 2015; 16:996 – 1001
Submission history: Revision received June 26, 2015; Submitted September 3, 2015; Accepted September 24, 2015
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 1996.
2. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377-85.
3. Goldberg R, Boss RW, Chan L, et al. Burnout and its correlates in emergency physicians: four years’ experience with a wellness booth. Acad Emerg Med. 1996;3:1156-64.
4. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995-1000.
5. West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296:1071-8.
6. West CP, Tan AD, Habermann TM, et al. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302:1294-300.
7. Prins JT, van der Heijden FM, Hoekstra-Weebers JE, et al. Burnout, engagement and resident physicians’ self-reported errors. Psychol Health Med. 2009;14:654-66.
8. Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358-67.
9. de Oliveira GS, Chang R, Fitzgerald PC, et al. The Prevalence of Burnout and Depression and Their Association with Adherence to Safety and Practice Standards: A Survey of United States Anesthesiology Trainees. Anesth Analg. 2013.
10. Mache S, Vitzthum K, Klapp BF, et al. Surgeons’ work engagement: Influencing factors and relations to job and life satisfaction. Surgeon. 2013.
11. Mache S, Vitzthum K, Klapp BF, et al. Improving quality of medical treatment and care: are surgeons’ working conditions and job satisfaction associated to patient satisfaction?. Langenbecks Arch Surg. 2012;397:973-82.
12. Williams ES, Manwell LB, Konrad TR, et al. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manage Rev. 2007;32:203-12.
13. Halbesleben JR, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev. 2008;33:29-39.
14. Argentero P, Dell’Olivo B, Ferretti MS. Staff burnout and patient satisfaction with the quality of dialysis care. Am J Kidney Dis. 2008;51:80-92.
15. Shanafelt T, Sloan J, Satele D, et al. Why do surgeons consider leaving practice?. J Am Coll Surg. 2011;212:421-2.
16. Shanafelt TD, Raymond M, Kosty M, et al. Satisfaction with work-life balance and the career and retirement plans of US oncologists. J Clin Oncol. 2014;32:1127-35.
17. Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146:54-62.
18. van der Heijden F, Dillingh G, Bakker A, et al. Suicidal thoughts among medical residents with burnout. Arch Suicide Res. 2008;12:344-6.
19. Oreskovich MR, Kaups KL, Balch CM, et al. Prevalence of alcohol use disorders among American surgeons. Arch Surg. 2012;147:168-74.
20. Toker S, Shirom A, Shapira I, et al. The association between burnout, depression, anxiety, and inflammation biomarkers: C-reactive protein and fibrinogen in men and women. J Occup Health Psychol. 2005;10:344-62.
21. Melamed S, Shirom A, Toker S, et al. Burnout and risk of cardiovascular disease: evidence, possible causal paths, and promising research directions. Psychol Bull. 2006;132:327-53.
22. Melamed S, Shirom A, Toker S, et al. Burnout and risk of type 2 diabetes: a prospective study of apparently healthy employed persons. Psychosom Med. 2006;68:863-9.
23. Schmoldt RA, Freeborn DK, Klevit HD. Physician burnout: recommendations for HMO managers. HMO Pract. 1994;8:58-63.
24. Estryn-Behar M, Doppia MA, Guetarni K, et al. Emergency physicians accumulate more stress factors than other physicians-results from the French SESMAT study. Emerg Med J. 2011;28:397-410.
25. Eckleberry-Hunt J, Lick D, Boura J, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009;84:269-77.
26. Dewa CS, Loong D, Bonato S, et al. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14:325.
27. Dyrbye LN, West CP, Shanafelt TD. Defining burnout as a dichotomous variable. J Gen Intern Med. 2009;24:440.
28. Whooley MA, Avins AL, Miranda J, et al. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12:439-45.
29. Shanafelt TD, Novotny P, Johnson ME, et al. The well-being and personal wellness promotion strategies of medical oncologists in the North Central Cancer Treatment Group. Oncology. 2005;68:23-32.
30. Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250:463-71.
31. The future of emergency care in the United States health system. Ann Emerg Med. 2006;48:115-20.
32. Camargo CA, Tsai CL, Sullivan AF, et al. Safety climate and medical errors in 62 US emergency departments. Ann Emerg Med. 2012;60:555-63.e20.
33. Kimo Takayesu J, Ramoska EA, Clark TR, et al. Factors Associated With Burnout During Emergency Medicine Residency. Acad Emerg Med. 2014;21:1031-5.
34. Ahmed N, Devitt KS, Keshet I, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg. 2014;259:1041-53.
35. Kellermann AL, Hsia RY, Yeh C, et al. Emergency care: then, now, and next. Health affairs. 2013;32:2069-74.
36. West CP, Shanafelt TD. The influence of personal and environmental factors on professionalism in medical education. BMC Med Educ. 2007;7:29.
37. Bennett N, Lockyer J, Mann K, et al. Hidden curriculum in continuing medical education. J Contin Educ Health Prof. 2004;24:145-52.
38. Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443-51.
39. Maslach CJ, Susan E, Leiter , Michael P. Maslach Burnout Inventory Manual. 1996.
40. Iacovides A, Fountoulakis KN, Kaprinis S, et al. The relationship between job stress, burnout and clinical depression. J Affect Disord. 2003;75:209-21.
41. Ahola K, Honkonen T, Isometsa E, et al. The relationship between job-related burnout and depressive disorders–results from the Finnish Health 2000 Study. J Affect Disord. 2005;88:55-62.
42. Burbeck R, Coomber S, Robinson SM, et al. Occupational stress in consultants in accident and emergency medicine: a national survey of levels of stress at work. Emerg Med J. 2002;19:234-8.
43. Gallery ME, Whitley TW, Klonis LK, et al. A study of occupational stress and depression among emergency physicians. Ann Emerg Med. 1992;21:58-64.
44. Lloyd S, Streiner D, Shannon S. Burnout, depression, life and job satisfaction among Canadian emergency physicians. J Emerg Med. 1994;12:559-65.
45. Cydulka RK, Korte R. Career satisfaction in emergency medicine: the ABEM Longitudinal Study of Emergency Physicians. Ann Emerg Med. 2008;51:714-22.e1.
46. Leigh JP, Kravitz RL, Schembri M, et al. Physician career satisfaction across specialties. Arch Internal Med. 2002;162:1577-84.
47. Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336:488-91.
48. Firth-Cozens J, Greenhalgh J. Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44:1017-22.
49. Garman AN, Corrigan PW, Morris S. Staff burnout and patient satisfaction: evidence of relationships at the care unit level. J Occup Health Psychol. 2002;7:235-41.
50. Kushnir T, Greenberg D, Madjar N, et al. Is burnout associated with referral rates among primary care physicians in community clinics?. Fam Pract. 2014;31:44-50.


