| Author | Affiliation |
| Benjamin A. White, MD | Massachusetts General Hospital, Department of Emergency Medicine, Boston, Massachusetts |
| Yuchiao Chang, PhD | Massachusetts General Hospital, Department of Emergency Medicine, Boston, Massachusetts |
| Beth G. Grabowski, MBA | Massachusetts General Hospital, Department of Emergency Medicine, Boston, Massachusetts |
| David F.M. Brown, MD | Massachusetts General Hospital, Department of Emergency Medicine, Boston, Massachusetts |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
While emergency department (ED) crowding has myriad causes and negative downstream effects, applying systems engineering science and targeting throughput remains a potential solution to increase functional capacity. However, the most effective techniques for broad application in the ED remain unclear. We examined the hypothesis that Lean-based reorganization of Fast Track process flow would improve length of stay (LOS), percent of patients discharged within one hour, and room use, without added expense.
Methods
This study was a prospective, controlled, before-and-after analysis of Fast Track process improvements in a Level 1 tertiary care academic medical center with >95,000 annual patient visits. We included all adult patients seen during the study periods of 6/2010-10/2010 and 6/2011-10/2011, and data were collected from an electronic tracking system. We used concurrent patients seen in another care area used as a control group. The intervention consisted of a simple reorganization of patient flow through existing rooms, based in systems engineering science and modeling, including queuing theory, demand-capacity matching, and Lean methodologies. No modifications to staffing or physical space were made. Primary outcomes included LOS of discharged patients, percent of patients discharged within one hour, and time in exam room. We compared LOS and exam room time using Wilcoxon rank sum tests, and chi-square tests for percent of patients discharged within one hour.
Results
Following the intervention, median LOS among discharged patients was reduced by 15 minutes (158 to 143 min, 95%CI 12 to 19 min, p<0.0001). The number of patients discharged in <1 hr increased by 2.8% (from 6.9% to 9.7%, 95%CI 2.1% to 3.5%, p<0.0001), and median exam room time decreased by 34 minutes (90 to 56 min, 95%CI 31 to 38 min, p<0.0001). In comparison, the control group had no change in LOS (265 to 267 min) or proportion of patients discharged in <1 hr (2.9% to 2.9%), and an increase in exam room time (28 to 36 min, p<0.0001).
Conclusion
In this single center trial, a focused Lean-based reorganization of patient flow improved Fast Track ED performance measures and capacity, without added expense. Broad multi-centered application of systems engineering science might further improve ED throughput and capacity.
INTRODUCTION
Emergency department (ED) crowding remains a national crisis, and a multitude of studies have demonstrated myriad negative effects on patient care efficiency, quality, and safety.1-20 Moreover, the burden of capacity constraints on United States EDs is predicted to worsen in the future.20
In addition, while multiple studies and governing bodies, including the Institute of Medicine (IOM),20 have suggested increased use of systems engineering and improvement science to combat this growing problem, only recently has the emergency medicine literature started to demonstrate the successes that many similarly complex industries discovered long ago.21-24 Still, there remains significant opportunity to refine the use and application of these tools across EDs in an effort to continue to optimize care, especially with respect to streamlining processes and improving throughput, and thus creating much needed capacity.25-30 For example, Lean methodologies, originally designed for use in process improvement in the manufacturing industry, represent one potential tool for use in improving systems of care and throughput in the ED.31-33 While much interest has been generated recently in other settings, these tools have been only minimally studied in health care as a whole, and less so in the ED specifically.34-37
Finally, in terms of systems improvement opportunities, emergency medicine is somewhat unique in that, in most instances, increased patient care efficiency not only decreases waste and costs, but also improves, rather than just maintains, quality. This occurs through effects on the IOM domains of timeliness, efficiency, effectiveness, and safety.20 In addition, the Centers for Medicare & Medicaid Services (CMS) have recently added publically-reported ED performance metrics to their clinical quality measures, including ED length-of-stay (LOS) for admitted and discharged patients (NQF 0495 & 0496), and the door to diagnostic evaluation by medical personnel (NQF 0498).38,39
In this study, our ED used Lean-based systems engineering tools to reorganize patient flow through the Fast Track area, with the goal of improving capacity without added expense or resources. Drawing on multiple systems engineering theories, including queuing theory, the theory of constraints, and demand-capacity matching, we sought to optimize patient care given available resources, and begin to quantify the value of such an intervention.
METHODS
Study Design
This prospective controlled before-and-after analysis of Fast Track (FT) process improvements compared performance measures over two six-month periods (June-October, 2010 and June-October, 2011). We chose the period of six months to provide adequate sample size, and we chose the identical months to avoid any seasonal effect. The ED staff and all participants were unaware of the data collection or analysis, but could not be blinded to the intervention. The intervention occurred over the winter of 2010-2011, and was completed by May 2011. This was a quality assurance project examining internal operations, specifically our new triage system. We reviewed administrative data, but not individual patient medical records. As such the study was exempted from full Istitutional Review Board review.
Study Setting and Population
The study was performed in a large, urban, academic ED with an annual census of approximately 95,000. The ED serves as a Level I trauma center for adult and pediatric patients, as well as a regional burn center. The admission rate is approximately 26%, and approximately 31% of all visits arrive by ambulance. Patient flow in the ED follows a relatively standard course with triage, registration, evaluation in a care area, and disposition. Our ED has six separate care units, differentiated largely by the acuity or age of the patients in each unit. Patients triaged to Fast Track are of the lowest acuity, and consist of chief complaints similar to other EDs (e.g. lacerations, minor injuries, isolated extremity fractures, simple cellulitis, etc). The patient population seen in the control area, Supplemental Triage and Rapid Treatment (START), are of medium acuity (e.g. abdominal pain, flank pain, dizziness, etc). These patients are initially examined by an MD/PA team in dedicated “screening” (exam) rooms, and then cared for in a large internal waiting and treatment area. This process has been described previously.40,41 We used the screening exam room time of START patients as a comparison, as there were no changes made to this process flow during the study period.
Selection of Participants
We included all adult patients triaged to the FT (i.e. non-emergent), and START areas during the study periods in the analysis.
Data collection and processing
We obtained data from an electronic patient tracking system (EDIS) regarding individual throughput data in both the pre-intervention period and the post-intervention period. EDIS is a software program developed specifically for our ED by our institution. Data points included age, sex, hospital visit level (E/M code), disposition, and time stamped data, including ED LOS and time spent in an exam room. Our ED does not use Emergency Severity Index.
Intervention
The intervention was a focused Lean-based reorganization of patient flow through existing FT rooms, based in systems engineering science and modeling, including queuing theory, demand-capacity matching, and Lean methodologies.
As is common with Lean interventions, we began by modeling the current state of patient flow through the FT area of our ED. Patients are directed to the Fast Track area after triage (by an experienced RN) and registration; this process was not altered. Upon arrival to Fast Track, patients were directed to a waiting room, where they were then escorted to an exam room or stretcher space for evaluation. Evaluation was performed by an RN, PA, resident MD, attending MD, or some combination thereof, and often in serial. (All patients are seen by the attending MD in our ED.) There was no change to the staffing model or caregiver types during the study period. Following evaluation, patients received further diagnostic testing and treatment, including procedures, and often spent the time waiting for these serial process steps in an exam room. If the patient was discharged, this process was also frequently completed by staff in the exam room.
After modeling the system, we collected and analyzed baseline data regarding our patient flow, including input-throughput-output, and standard ED performance metrics including ED LOS. We also stratified the patient population by needs to determine how best to ration our most limited “bottleneck” resources of rooms, MD time, and RN time. Using medians, we determined that we see approximately 68 patients per day in the Fast Track area, five (7%) of whom are admitted to an inpatient care unit, and three (4%) of whom are admitted to an ED-based observation unit. While FT is open 24 hours per day, peak arrivals occur between 11am-8pm, with approximately 4-7 patients per hour, and resulting in a steadily increasing peak census of 12-20 patients present from noon-10pm. Of those patients, all receive an exam, and approximately 53% receive some form of nursing intervention or treatment, and 32% have a procedure performed (e.g., laceration repair, abscess incision and drainage). We created a rudimentary model based on estimated cycle times of exams and various procedures, and predicted resources needed, and determined the best use of our limited treatment room space. We also investigated the most common diagnoses seen in the FT area, and collected baseline data on LOS and disposition.
Next, we reviewed the relevant systems engineering theory that might apply to our planned future state. These included Lean methodologies, Six Sigma, Queuing theory, demand/capacity management, the Theory of Constraints, managing variation, forecasting and scenario analysis. With that background in mind, we developed clear goals for the future state, including:
1) Simplify whenever possible
2) Reduce waste, especially of limited resources (e.g.,
staff, exam rooms)
3) Maintain forward progress at all times
4) Support and plan for inherent behaviors of both staff
and patients
5) Plan capacity to meet demand, and exceed it if possible
6) Draw on successes & test new ideas, with an aim to the
future state
7) Develop a culture of continuous quality improvement
(“Kaizen”)
As such, our specific intervention focused on decreasing time to MD exam, and thus order entry; decreasing non-value added room time; maintaining throughput at all process steps; eliminating bottlenecks when identified; and planning capacity to meet demand.
The crux of the intervention was a re-organization of room use and patient flow, in which three of the seven treatment rooms were re-allocated as “exam-only” rooms, and four rooms optimized as “procedure rooms.” In the new patient flow (Figure), patients are met by a greeter RN, triaged, and registered in an identical fashion as prior to the intervention (1). They are then directed to an exam room (2) on arrival to FT and seen by the MD/PA team, unless there is a queue, in which case they are directed to the waiting room (4). If patients have an obvious diagnosis requiring a procedure, such as an actively bleeding wound or fracture, they are directed to a procedure room or a previously existing optimized orthopaedics room (3). Following the exam, the patient is either directed to a procedure room if intravenous therapy or a procedure is indicated (3), directed to the results waiting area (4), directed to a stretcher space if needed (5), or discharged (6). If the patient requires admission, they are admitted from any of the above locations.
 Figure. Lean patient flow intervention with associated change in text.
Figure. Lean patient flow intervention with associated change in text.
Regarding optimizing room turnaround time, “procedure carts” were created in each of the procedure rooms, such that providers would not have to leave the room each time to gather supplies, and based on Lean “5S” methodology a workplace organization system (i.e., sorting, setting in order, systematic cleaning, standardizing, and sustaining) was set up. Paper roll dispensers were also installed in each of the exam rooms to decrease room turnover time. Finally, the patient chart/paperwork system was re-designed in order to simplify its organization, and such that a patient’s information was no longer tied to the room they were occupying (given the rapidity with which it was predicted that the room would change).
There were no changes to staffing or resources added during this intervention. In addition, there were no other significant and identifiable operations changes affecting FT patient flow between the two study periods.
Methods of measurement
The primary outcomes measured were FT LOS, defined as the time interval between patient registration in the ED and leaving the ED, percentage of patients discharged in less than one hour, and exam room time, defined as the time interval during which a patient was physically in a room, as measured by our computerized tracking system (EDIS). Patient characteristics, LOS, and percentage of patients discharged in less that one hour were also measured in a control patient care area in which the intervention was not applied. This medium acuity patient care area, called START, did not undergo any significant operational changes during the study periods.
Primary Data Analysis
We summarized patient characteristics between the two time periods using mean and standard deviation for continuous variables and percentage for categorical variables. ED LOS and exam room time were summarized with medians and inter-quartile ranges, and compared between groups using Wilcoxon rank sum test since the distribution for LOS was usually skewed. We used bootstrap sampling methods to calculate the 95% CI for the difference in medians. The percentage of patients discharged within one hour was presented with 95% confidence intervals and compared between groups using Chi-squared test. Two-sided p-values ≤ 0.05 were considered statistically significant. We did all analyses using SAS version 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
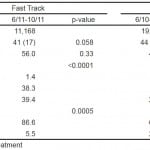
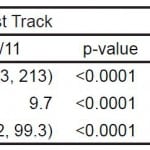
The total FT patient volume was 11,185 during the pre-intervention period, and 11,168 during the post-intervention period. Patient volumes in the control area (START) were 19,065 pre-intervention and 18,269 post-intervention. We included all of these patient visits in the analysis, and patient characteristics, including age, sex, hospital visit level, and disposition, were similar across the two groups (Table 1), despite the statistical significance due to the large sample size.
Table 1. Patient characteristics.
START, Supplemental Triage and Rapid Treatment
Following the intervention, median LOS among discharged patients in the FT area was reduced by 15 minutes (158 to 143 min, 95%CI 12 to 19 min, p<0.0001) (Table 2). The number of patients discharged in <1 hr increased by 2.8% (from 6.9% to 9.7%, 95%CI 2.1% to 3.5%, p<0.0001), and median exam room time decreased by 34 minutes (90 to 56 min, 95%CI 31 to 38 min, p<0.0001). In comparison, patients seen in START had no change in median LOS (265 to 267 min) or in proportion of patients discharged in <1 hr (2.9% to 2.9%), and a significant increase in median exam room time (28 to 36 min, p<0.0001).
Table 2. Before and after intervention results.
START, Supplemental Triage and Rapid Treatment; LOS, length of stay
DISCUSSION
In this single center trial, a focused Lean-based reorganization of patient flow decreased discharged patient LOS by 15 minutes, and exam room time by 34 minutes, without added expense and with very little resource use. If confirmed in other studies and settings, our results have important implications. First and foremost, these results exemplify the potential value of applying systems engineering and improvement science to create capacity in the ED. Consider that for a capacity-constrained ED, creating 34 minutes of room capacity over 11,168 patients is the equivalent of creating 6,328 hours of room capacity, or approximately 35 hours per day. This is equivalent to building 1.5 new rooms in the ED, but without any added expense.
In addition, while the intervention required moderate effort in the modeling and data collection phase, the operational benefits gained far outweighed the resources spent on this project. This is a common experience with systems engineering solutions, and Lean methodologies specifically, and often leads to cultural change towards continuous quality improvement and improved staff satisfaction, resulting in a self-propagating positive feedback loop of process improvement and synergistic effects with upstream and downstream processes.31-37 Another benefit of this approach is the team-oriented and multidisciplinary fashion with which these systems are modeled and improved. This not only encourages solution sharing and broad “buy-in,” but also decreases the likelihood of the intervention(s), creating unintended bottlenecks or workflow imbalances.
In an era of increasing ED crowding nationwide, solutions that have the potential to increase throughput and reduce LOS, and thus increase efficiency and capacity, with minimal associated costs, may represent the most readily achievable gains for emergency medicine administrators.
LIMITATIONS
There are limitations with this study as performed. Most importantly, as with any before-after study, while the outcomes measured may have proved association, they do not confirm causality.
In addition, this study was performed at a single institution, and thus the findings might not be generalizable to EDs with markedly different demographics, or without a FT area. However, given that improvement science is by definition broadly applicable, our findings should be of value to most ED administrators on some level.
Thirdly, participants were not able to be blinded to the intervention, raising the possibility of contribution of the Hawthorne effect to study outcomes. However, the fact that the post-intervention study period occurred months after the intervention was initiated should serve to mitigate this effect, in that study participants had ample time to become familiar with the new system, and were less likely to alter their actions as if they were being observed.
Other known contributors to prolonging ED LOS, such as patient volume, did not change significantly in the intervention group during the period studied. A small change in percentage of level 2 and level 3 patients was noted following the intervention, as was a very small decrease in the percentage of admitted patients, and the degree to which this contributed to the results is unknown. It is also possible that the new, Lean-focused system slightly altered the overall treatment, documentation, and coding of patient visits, which may have altered the visit level as noted, especially given the visit levels in START did not change during the study period. In addition, while boarding inpatients is an issue in our ED, there was no significant change in boarding burden during the study period.
While there was a small decrease in patient volume in the control group during the post intervention phase, based on prior experience and extant literature, we would expect this to decrease LOS. However, LOS and exam room time actually increased slightly in the control group during the post-intervention phase, further emphasizing the significance of our results.
Finally, the intervention studied actually consisted of a number of smaller systems improvements grouped into a single process change. While this is more practically feasible and frequently the case with systems engineering and redesign, our study design does not permit interpretation of each component’s individual contribution to the results.
We were otherwise unable to identify any other major systems or operations changes in the ED process flow during this time period, but other contributing factors cannot be fully excluded, such as differences in individual productivity, or subtle differences across the patient population studied.
CONCLUSION
In this single center trial, a focused, Lean-based reorganization of patient flow improved ED performance measures and capacity, without added expense. Broad, multi-centered application of systems engineering science might further improve ED throughput and capacity.
Footnotes
Supervising Section Editor: Jeffery Druck, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Benjamin A. White, MD, Department of Emergency Medicine, Massachusetts General Hospital, Zero Emerson Place-3b, Boston, MA 02114. Email: bwhite3@partners.org.
Submission history: Submitted January 31, 2014; Accepted August 8, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61:605-611.
- Pines JM, McCarthy ML. The Crowding-Effectiveness Link: It doesn’t matter how fast we deliver care if we don’t deliver it right. Ann Emerg Med. 2011;57:201-202.
- Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16:1-10.
- Miro O, Antonio MT, Jimenez S, et al. Decreased health care quality associated with emergency department overcrowding. Eur J Emerg Med. 1999;6:105-107.
- Croskerry P, Sinclair D. Emergency medicine: A practice prone to error? CJEM. 2001;3:271-276.
- Schull MJ, Vermeulen M, Slaughter G, et al. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med. 2004;44:577-585.
- Cowan RM, Trzeciak S. Clinical review: Emergency department overcrowding and the potential impact on the critically ill. Crit Care. 2005;9:291-295.
- Fee C, Weber EJ, Maak CA, et al. Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Ann Emerg Med. 2007;50:501-9, 509.e1.
- Hwang U, Richardson L, Livote E, et al. Emergency department crowding and decreased quality of pain care. Acad Emerg Med. 2008;15(12):1248-55.
- Hwang U, Richardson LD, Sonuyi TO, et al. The effect of emergency department crowding on the management of pain in older adults with hip fracture. J Am Geriatr Soc. 2006;54:270-275.
- Magid DJ, Asplin BR, Wears RL. The quality gap: Searching for the consequences of emergency department crowding. Ann Emerg Med. 2004;44:586-588.
- Pines JM, Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:1-5.
- Pines JM, Hollander JE, Localio AR, et al. The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Acad Emerg Med. 2006;13:873-878.
- Pines JM, Iyer S, Disbot M, et al. The effect of emergency department crowding on patient satisfaction for admitted patients. Acad Emerg Med. 2008;15:825-831.
- Baker DW, Stevens CD, Brook RH. Patients who leave a public hospital emergency department without being seen by a physician, causes and consequences. JAMA. 1991;266:1085-1090.
- McCarthy ML, Zeger SL, Ding R, et al. Crowding delays treatment and lengthens emergency department length of stay, even among high-acuity patients. Ann Emerg Med. 2009;54(4):492-503.
- Barrett TW, Schriger DL. Annals of emergency medicine journal club, emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:6-7.
- Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust. 2006;184:213-216.
- Sprivulis PC, Da Silva JA, Jacobs IG, et al. The association between hospital overcrowding and mortality among patients admitted via western Australian emergency departments. Med J Aust. 2006;184:208-212.
- Institute of Medicine, Committee on the Future of Emergency Care in the United States Health System. Hospital-based emergency care: At the breaking point. 2006. Available at http://www.iom.edu.
- Hogan B, Rasche C, Braun von Reinersdorff A. The first view concept: introduction of industrial flow techniques into emergency medicine organization. Eur Journal Emerg Med. 2012;19:136-139.
- Eitel DR, Rudkin SE, Malvehy MA, et al. Improving service quality by understanding emergency department flow: a white paper and position statement prepared fro the american academy of emergency medicine. J Emerg Med. 2010;38:70-79.
- Hoot NR, Aronsky D. Systematic review of emergency department crowding: Causes, effects, and solutions. Ann Emerg Med. 2008;52:126-136.
- Han JH, Zhou C, France DJ, et al. The effect of emergency department expansion on emergency department overcrowding. Acad Emerg Med. 2007;14:338-343.
- Storrow AB, Zhou C, Gaddis G, et al. Decreasing lab turnaround time improves emergency department throughput and decreases emergency medical services diversion: A simulation model. Acad Emerg Med. 2008;15:1130-1135.
- Asplin BR, Magid DJ, Rhodes KV, et al. A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42:173-180.
- Holroyd BR, Bullard MJ, Latoszek K, et al. Impact of a triage liaison physician on emergency department overcrowding and throughput: A randomized controlled trial. Acad Emerg Med. 2007;14:702-708.
- Han JH, France DJ, Levin SR, et al. The effect of physician triage on emergency department length of stay. J Emerg Med. 2010;39:227-233.
- Weintraub B, Hashemi T, Kucewicz R. Creating an enhanced triage area improves emergency department throughput. J Emerg Nurs. 2006;32:502-505.
- Asaro PV, Lewis LM, Boxerman SB. The impact of input and output factors on emergency department throughput. Acad Emerg Med. 2007;14:235-242.
- Graban M. Lean Hospitals: Improving Quality, Patient Safety, and Employee Satisfaction. Productivity Press, 2008.
- Dickson, EW, Singh S, Cheung DS, et al. Application of Lean Manufacturing Techniques in the Emergency Department. J Emerg Med. 2009;37:177-82.
- Dart RC. Can lean thinking transform American health care? Ann Emerg Med. 2011;57:279-281.
- Holden RJ. Lean thinking in emergency departments: a critical review. Ann Emerg Med. 2011;57:265-278.
- Decker, WW, and Stead, LG. Application of Lean Thinking in Health Care: A Role in Emergency Departments Globally. Int J Emerg Med. 2008;1.3:161-2.
- Dickson, EW, Anguelov Z, Vetterick D, et al. Use of Lean in the Emergency Department: A Case Series of 4 Hospitals. Ann Emerg Med. 2009;54:504-10.
- Parks, JK, Klein J, Frankel HL, et al. Dissecting Delays in Trauma Care using Corporate Lean Six Sigma Methodology. J Trauma. 2008;65:1098-1104.
- The Healthcare Imperative: Lowering Costs and Improving Outcomes – Workshop Series Summary – Institute of Medicine. Available at http://www.iom.edu/Reports/2011/The-Healthcare-Imperative-Lowering-Costs-and-Improving-Outcomes.aspx.
- Clinical Quality Measures for CMS’s 2014 EHR Incentive Program for Eligible Hospitals: Release Notes: 2012. Available at http://www.cms.gov.
- White BA, Brown DF, Sinclair J, et al. Supplemented Triage and Rapid Treatment (START) improves performance measures in the emergency department. J Emerg Med. 2012;42:322-8.
- Rogg J, White BA, Biddinger PD, et al. A long term analysis of physician screening in the emergency department. Acad Emerg Med. 2013;20:374-380.