| Author | Affiliation |
|---|---|
| Rebecca K. Jeanmonod, MD | St. Luke’s Hospital and Health Network, Bethlehem, PA |
| Donald Jeanmonod, MD | St. Luke’s Hospital and Health Network, Bethlehem, PA |
| Sara Damewood, MD | Palmetto Health Richland, Columbia, SC |
| Cheryl Perry, MD | Cape Fear Valley Medical Center, Fayetteville, NC |
| Marwan Powers, MD | Cape Fear Valley Medical Center, Fayetteville, NC |
| Vicky Lazansky, DO | St. Luke’s Hospital and Health Network, Bethlehem, PA |
ABSTRACT
Introduction:
This study sought to investigate the patterns of injury resulting from a punch mechanism and to investigate the associated psychopathology present in patients with these injuries.
Methods:
Retrospective analysis of patients with hand radiographs ordered from the emergency department allowed for identification of patients with a punch mechanism. We recorded injury patterns and queried patients’ medical records for associated psychopathology.
Results:
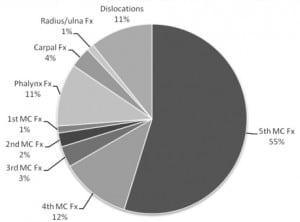
1,292 patients underwent hand radiographs during a one-year time period; 172 patients (13%) were radiographed following an intentional punch injury, identifying 76 fractures in 70 patients. Males contributed a greater proportion of patients presenting with punch injury when compared to females (80% vs. 20%). Males were more likely to sustain fracture from a punch mechanism (48% vs. 11%, OR 7 [95% CI 2.3–20.9]), but were less likely to have preexisting documented psychiatric disease (23% vs. 49%, OR 3.1 [95% CI 1.4–6.7]). Of all fractures, 61% were to the fifth metacarpal, 21% were to the remainder of the metacarpals, and the remaining were fractures to phalanges and bones of the wrist.
Conclusion:
Women are less likely to present with punch injury and are less likely to sustain a fracture when they do present but have more associated psychiatric disease. Both men and women presenting with punch injuries have a higher prevalence of psychiatric disease than the background incidence in the population as a whole. Although punch injuries result in a significant number of boxer fractures, a number of other injuries are associated with punch mechanisms.
INTRODUCTION
Injuries of the hand and wrist are among the most common traumatic injuries seen in emergency departments (EDs), accounting for up to 15% of all injuries.1,2 Many of these injuries are fractures, with metacarpal and phalangeal fractures the most common.2 Although seemingly minor, these injuries have the potential to affect the function of the patient’s hand in both the short- and long-term, causing significant morbidity.
Although most hand injuries are unintentional, a large number occur intentionally, as the result of a closed fist striking a hard immovable object. Closed fist or punch injuries are usually associated with fractures of the fifth metacarpal neck (classic boxer’s fracture), but this mechanism is also responsible for a variety of other injury patterns. Like other hand injuries, punch injuries have the potential for considerable morbidity. This makes them of even greater significance, as the highest risk population is young males 15–24 years old, and these injuries may impact their ability to work or even permanently disable them.3,8 Indeed, young men have been found to incur 60% of all hand injuries and more than 90% of all boxer’s fractures.4,9–11
Substantial psychopathology is believed to be associated with intentional boxer’s fractures, including depression, anxiety and personality disorders. In a small study of 14 patients with boxer’s fractures, it was found that patients with these injuries have higher levels of anti-social traits, anxiety and self-defeating traits than patients with other types of fractures or normal controls.12 These patients are also believed to have a high rate of injury recidivism, with studies reporting a repeat injury rate of up to 27%.4,13
Although several studies in Europe and the United States have discussed the epidemiology of hand and wrist fractures, most of them are nonspecific regarding the mechanism of injury leading to specific fracture types. In addition, although there have been some studies looking specifically at boxer’s fractures occurring from all mechanisms, none have examined the spectrum of bony injuries incurred from a mechanistic point of view, specifically intentional punch injuries. Our objective was to look at injury patterns sustained secondary to a punch mechanism, as we hypothesized that there might be many bony injuries beyond boxer’s fractures that occur from intentionally striking a person or object. We also sought to further delineate the presence of psychiatric co-morbidity associated with punch injury and the incidence of injury recidivism in men and women.
METHODS
Study Design and Setting
This is a retrospective study performed at an academic Level I trauma center with an annual volume of 72,000. The study protocol was reviewed and approved by the Institutional Review Board. We included all ED patients who underwent a radiographic study of their hands for intentional punch injuries from July 1, 2007 to June 30, 2008. We excluded children under the age of 13 and patients for whom a confirmatory electronic medical record could not be located. Research associates queried the electronic Picture ArChiving Communication System (PACS) for patients who had hand films performed during the study period and then identified the mechanism of injury through the radiology requisition form and the electronic medical record for that visit. Mechanism of injury was chosen from a closed list of mechanisms (for example, “punch,” “fall,” “atraumatic,” etc). The presence or absence of a fracture or dislocation, the location of the fracture, and the presence of old or healing fractures was noted from the radiology report.
We used the PACS to ascertain if the patient had had previous ED hand radiographs for punch injuries. The electronic medical record was also queried for details regarding the patient’s ED visit, including age at time of visit, gender, psychiatric history and final diagnosis. If the radiographic result was unclear, we used the final clinical diagnosis on the chart to determine presence or absence of fracture.
Psychiatric disease was defined as Axis I (major psychiatric disorders), Axis 2 (pervasive personality disorders) and substance abuse disorders listed on the patient’s chart either as part of his/her past medical history or listed in the final diagnoses. If a patient was intoxicated, but was not listed as having alcoholism as a medical problem, he/she was not placed under the categorization of possessing a psychiatric disorder. If the patient had an older chart listing mental illness, but none on the current chart being queried, the patient was not placed under the categorization of possessing a psychiatric disorder.
Intentional punch injuries were defined as report by the patient of striking a person or object with a closed fist. If a patient stated he/she was in an altercation but didn’t know how the injury occurred, the injury was not counted as an intentional punch injury and was instead categorized as “trauma, other.” Additionally, if a patient had a closed fist injury (for example, falling on a closed fist) but was not in the act of striking something or someone, the injury was not categorized as an intentional punch injury, but was categorized by how it occurred (for instance, “fall,” or “motor vehicle crash”).
We determined injury recidivism by the presence of previous hand radiographs performed for punch injuries in the PACS system. Recidivism was also reported if the patient reported previous punch-related injuries in the setting of old injuries noted on the radiograph from the study period. We did not count reported prior injuries with no radiographic corroboration of injury.
Research associates recorded all data and entered them into a standardized Excel spreadsheet. All items in the spreadsheet were entered from pull-down menus of closed lists. We calculated interobserver reliability among research associates and used descriptive statistics to analyze the data. We used the Fisher Exact Test to determine differences between male and female patients.
RESULTS
During the 12-month study period, 1,292 patients underwent 1,514 hand radiographs from the ED (1.8% of all patients). Four patients had no dictated ED chart and were therefore excluded from further analysis. One hundred seventy-two patients sought medical attention after intentionally striking an object with a closed fist and underwent 192 radiographs. The remaining radiographs were for the following indications: falls (286 films), major trauma (276 films), crush injuries (171 films), other known trauma, such as sports injuries (349 films), rule-out foreign body (86 films), atraumatic hand pain (98 films) and patients with unknown mechanism (52 films). Of the patients with unknown mechanism, seven reported being involved in altercations at the time of the incident, but could not recall how their hands were injured.
Of the 172 patients identified with a closed fist injury, 35 (20%) were women. Of women seen for punch injury, 17 (49%) had previous psychiatric diagnoses documented (Table 1). Ten (29%) had been seen in the ED on previous occasions for punch injuries. Four (11%) of the women with punch mechanism sustained a fracture, one of whom had an underlying psychiatric diagnosis. There were no women seen for intentional punch injury who had evidence of old or healing fractures on their radiographs. Ninety percent of female recidivists had documented psychiatric disease on their charts.
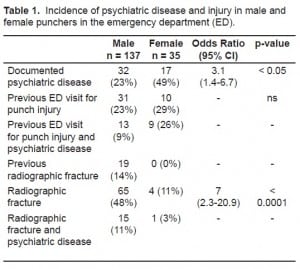
Of the 137 male patients evaluated for punch injuries, 32 (23%) had pre-existing psychiatric disease noted on their charts, and 31 (23%) had been radiographed on other occasions for punch injuries. Eleven of these had evidence of old or healing fractures. An additional eight patients had no old studies in the PACS system, but reported previous punch injury and had radiographic evidence of healing or old fractures on their current radiographs, for a total recidivism rate of 28% and a refracture rate of 14%. One-third of these recidivists had a documented psychiatric disease on their charts. Acutely, 65 (48%) of the male patients sustained fractures, and 15 (23%) of these had underlying psychiatric disease.
Males were more likely to suffer fractures from punch injuries when compared to females (p < 0.0001) with an odds ratio of 7 (confidence interval 2.3–20.9). Female punchers were much more likely than male punchers to have comorbid psychiatric disease (p = 0.004) with an odds ratio of 3.1 (confidence interval 1.4–6.7). There was no difference between the recidivism rate of female and male punchers (p = 1) nor was there any relationship between likelihood of fracture and presence of psychiatric disease in either group (p = 0.69 for men, p = 0.60 for women).
Of the 172 patients imaged for intentional punch injuries, there were 76 fractures in 70 patients (41%). Of all the fractures identified, 46 (61%) were fifth metacarpal fractures; however, the classic boxer’s fracture represented only 20 (26%) of these fractures. The remaining were mid- or proximal fifth metacarpal fractures. There were 16 (21%) fractures involving the other four metacarpals. There were 10 (13.3%) fractures of the fourth metacarpal, 3 (4%) of the third metacarpal, 2 (2.7%) of the second metacarpal and 1 (1.3%) of the first metacarpal. In addition, other injuries noted were nine (11.8%) phalanx fractures, three (4%) carpal fractures, and one (1.3%) radius and ulna fracture. There were also nine dislocations noted: three of the fifth metacarpal, three of the fourth metacarpal, one of the third metacarpal, and two involving phalanges (Figure 1).
Interobserver reliability was 1.0 for agreement on diagnosis of punch mechanism, patient age and gender, presence of psychiatric comorbidity, nature of injury, and presence of recidivism.
DISCUSSION
Hand injuries comprise a large proportion of ED visits, representing significant cost to the medical system and potential patient morbidity.1–2,7–8,11 Most of these injuries are accidental, secondary to falls, crush injuries, or major trauma. However, intentional hand injuries are an important sub-group to consider, since the nature of intentional injuries implies that they are potentially preventable. In our ED, self-inflicted hand injuries accounted for 13% of all hand radiographs performed during the study period. These injuries were almost exclusively to the patients’ dominant hand or wrist (one patient fractured both hands), thereby causing additional functional morbidity in terms of the patients’ ability to work and perform activities of daily living. The range of bony injuries was extensive, with only a quarter being the classically described boxer’s fracture.
Over the one-year study period, we found that women were far less likely to intentionally punch an object or person compared to men. This finding is consistent with other studies looking exclusively at boxer’s fractures from all mechanisms in men and women.3–4 Women were also less likely to suffer an injury as the result of their punch, with only 11% sustaining a fracture, compared to almost half of men. The smaller number of female punchers and the lack of serious injury in most women after punching an object may be because of differences in male and female baseline characteristics. Past data show that men engage in more risk-taking behavior, suffer more injuries, and harm themselves both fatally and non-fatally more often than women.14 Our findings may be an extension of these phenomena. This may also be due to last minute hesitation on the part of female punchers, or secondary to the fact that women typically have less upper body strength than men, and do not generate the force necessary to break bone.
Women in this study had a similar overall rate of recidivism (29%) compared to men (23%). These rates are consistent with other studies looking at hand fractures in general and boxer’s fractures in particular.4,13 Interestingly, in spite of this recidivism and the presence of acute fractures in 11% of women, no women had old fractures documented on their radiographs. Admittedly, the sample size of female punchers was small (n=35), but this also suggests that women, in addition to being less likely to suffer bony injury from punching, may also be less likely to do it again when they do incur fractures. Fifteen percent of men imaged for punch injuries had previous fractures documented, which may simply reflect the increased rate of fractures among men or may indicate a difficulty in processing the consequences of this self-destructive behavior.
Nearly half of the women in this study who did intentionally strike a person or object had underlying psychiatric disease, compared to less than a quarter of the men. This is much higher than the incidence of psychiatric disease in the general population, which is estimated to be about 20% for women and 8% for men over the course of a lifetime.14 Patients with mental illness may be more likely to punch people or objects because of increased frustration or anger related to their illness, poor interpersonal relationships that predisposed to the mental illness, or possibly secondarily to difficulties in verbal communication. Certainly, the disinhibition caused by drug and alcohol abuse may play a role, and many of our patients who had underlying mental illness were also intoxicated. There is a well-described relationship between substance use and abuse and mental illness, and this may play a synergistic role in intentional self-inflicted violent injuries.
Overall, this study demonstrates that punch as a mechanism of injury causes bony hand injuries far in excess of boxer’s fractures. Further, it shows that ED presentation for a punch injury is a marker for underlying psychiatric disease. This may seem self-evident to those who practice in emergency medicine, but has not previously been described or documented in the literature. Although our mental health system in the United States is in crisis, these data suggest that it is prudent to screen punching patients for psychiatric stability in much the way we do for those who self-mutilate or present with polysubstance abuse. Although we did not do a financial analysis, there is the potential for considerable cost of these injuries in terms of morbidity and disability to the patient as well as the financial cost to an already overburdened and overcrowded emergency healthcare system. This has been described in other studies.6–8 Since the rate of recidivism is so high and the co-incidence of punching injuries with psychiatric disease is so common, it seems reasonable to target these patients for urgent psychiatric referral and move toward prevention of these injuries, and not just acute treatment.
LIMITATIONS
This study is limited by nature of its design, which excluded any hand injury that was not radiographed. This could result in potentially missing patients who were transferred to the ED from community hospitals who did not have repeat films on arrival or patients in whom the clinical diagnosis of contusion or fracture was made. Although anecdotally we feel that it is uncommon for a patient to be seen in our ED with a punch-related injury who does not undergo radiographs, it is still possible. Additionally, one could argue that patients who are clinically diagnosed without imaging are likely to possess less physical strength, in order for the clinician to feel there is no fracture, and are therefore more likely to be women. This would result in selection bias. However, we feel the number of missed patients is likely to be small, and although including them would have strengthened our numbers and shown an even bigger impact of these injuries, it would have made it impossible to determine the specific bony injuries incurred, since none of these patients had films.
In addition, we may have underrepresented the incidence of psychiatric disease in the population, as we only included psychiatric diagnoses mentioned in the past medical history for the visit related to the punch injury, and did not look through previous charts. Therefore, our data is necessarily limited by the thoroughness of the charting of the ED residents, attending physicians, and mid-level providers. These injuries are often cared for in urgent care areas, and therefore may be subjected to less documentation scrutiny. That said, we felt it was more prudent to under-diagnose psychiatric disease rather than erroneously magnify the incidence of co-morbid psychiatric disease. Additionally, we felt that there is a possibility that a patient with psychiatric disease might undergo treatment and no longer be classified as mentally ill, and we did not want to classify “cured” psychiatric patients as having mental illness.
Furthermore, our study relied heavily upon patient history. There were likely many hand injuries from an intentional punch mechanism that were not included because the patient either wasn’t sure or wouldn’t report what happened. In our dataset, the majority of patients had punched objects, such as trees, walls, or refrigerators. Very few admitted to punching other people. However, some patients had been in altercations, and could not recall how their hands had been injured. All of these patients were excluded from analysis on the basis of unknown mechanism. Again, including these patients would likely have strengthened our argument regarding the importance of these injuries, but we felt the inability to completely classify them from a mechanistic standpoint mandated they be removed from the study population.
Finally, this study was performed at a single academic institution, and the results may not be incorporated to other institutions.
CONCLUSION
Self-inflicted hand injuries account for 13% of all hand radiographs performed in the ED. The classic boxer’s fracture accounts for only 20% of the fractures sustained through a punch mechanism indicating that a careful search for other injury patterns, including dislocations, is vital in the evaluation of these patients.
One-fifth of the patients presenting for punch injuries are women and although women are less likely to incur fractures from punch injury, about 10% do in fact suffer fractures. Almost half of these patients also carry an underlying psychiatric diagnosis. Men are much more likely to have fractures from self-inflicted injury but have a lower rate of psychiatric illness compared to women. Overall, punch as a mechanism of injury is a marker for underlying psychiatric disease, and it is prudent to screen these patients for this in order to appropriately refer them for care.
Footnotes
Supervising Section Editor: Laleh Gharahbaghian, MD
Submission history: Submitted July 5, 2010; Revision received September 13, 2010; Accepted September 27, 2010
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Rebecca Jeanmonod, MD, 801 Ostrum St., Bethlehem, PA 18015
Email: rebeccajeanmonod@yahoo.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Hove LM. Fractures of the hand. Distribution and relative incidence. Scand J Plast Reconstr Surg Hand Surg. 1993;27:317–9. [PubMed]
2. Frazier WH, Miller M, Fox RS, et al. Hand injuries: incidence and epidemiology in an emergency service. J Amer Col Emerg Phys. 1978;7:265–8.
3. Gudmundsen TE, Borgen L. Fractures of the fifth metacarpal. Acta Radiol. 2009;50:296–300.[PubMed]
4. Greer SE, Williams JM. Boxer’s fracture: an indicator of intentional and recurrent injury. Am J Emerg Med. 1999;17:357–60. [PubMed]
5. Lowdon IM. Fractures of the metacarpal neck of the little finger. Injury. 1986;17:89–92.
6. Bansal R, Graigen MA. Fifth metacarpal neck fractures: is follow-up required? J Hand Surg Eur.2007;32:69–73.
7. Rosberg HE, Carlsson KS, Dahlin LB. Prospective study of patients with injuries to the hand and forearm: costs, function, and general health. Scand J Plast Reconst Surg Hand Surg. 2005;39:360–9.
8. Larsen CF, Mulder S, Johansen AM, et al. The epidemiology of hand injuries in the Netherlands and Denmark. Eur J Epidemiol. 2004;19:323–7. [PubMed]
9. Stanton JS, Dias JJ, Burke FD. Fractures of the tubular bones of the hand. J Hand Surg Eur.2007;32:626–36.
10. Aitken S, Court-Brown CM. The epidemiology of sports-related fractures of the hand. Injury.2008;39:1377–83. [PubMed]
11. Van Onselen EB, Karim RB, Hage JJ, et al. Prevalence and distribution of hand fractures. J Hand Surg Br. 2003;28:491–5. [PubMed]
12. Mercan S, Uzun M, Ertugrul A, et al. Psychopathology and personality features in orthopedic patients with boxer’s fractures. Gen Hosp Psychiatry. 2005;27:13–7. [PubMed]
13. Finsen V, Benum P. The interrelationship of past and present fractures of the forearm and hand.Acta Orthop Scand. 1987;58:372–4. [PubMed]
14. Center for Disease and Control and Prevention Acta Orthop Scand. http://cdc.gov. Accessed January 11, 2010.


