| Author | Affiliation |
|---|---|
| Faheem W. Guirgis, MD | University of Florida, Department of Emergency Medicine, Jacksonville, Florida |
| Kelly Gray-Eurom, MD, MMM | University of Florida, Department of Emergency Medicine, Jacksonville, Florida |
| Teri L. Mayfield, MD | University of Florida, Department of Emergency Medicine, Jacksonville, Florida |
| David M. Imbt, MD | University of Florida, Department of Emergency Medicine, Jacksonville, Florida |
| Colleen J. Kalynych, MD | University of Florida, Department of Emergency Medicine, Jacksonville, Florida |
| Dale F. Kraemer, PhD | University of Florida College of Medicine, Jacksonville; Center for Health Equity and Quality Research |
| Steven A. Godwin, MD | University of Florida, Department of Emergency Medicine, Jacksonville, Florida |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
In 2007 there were 64,000 visits to the emergency department (ED) for possible myocardial infarction (MI) related to cocaine use. Prior studies have demonstrated that low- to intermediate-risk patients with cocaine-associated chest pain can be safely discharged after 9–12 hours of observation. The goal of this study was to determine the safety of an 8-hour protocol for ruling out MI in patients who presented with cocaine-associated chest pain.
Methods
We conducted a retrospective review of patients treated with an 8-hour cocaine chest pain protocol between May 1, 2011 and November 30, 2012 who were sent to the clinical decision unit (CDU) for observation. The protocol included serial cardiac biomarker testing with Troponin-T, CK-MB (including delta CK-MB), and total CK at 0, 2, 4, and 8 hours after presentation with cardiac monitoring for the observation period. Patients were followed up for adverse cardiac events or death within 30 days of discharge.
Results
There were 111 admissions to the CDU for cocaine chest pain during the study period. One patient had a delta CK-MB of 1.6 ng/ml, but had negative Troponin-T at all time points. No patient had a positive Troponin-T or CK-MB at 0, 2, 4 or 8 hours, and there were no MIs or deaths within 30 days of discharge. Most patients were discharged home (103) and there were 8 inpatient admissions from the CDU. Of the admitted patients, 2 had additional stress tests that were negative, 1 had additional cardiac biomarkers that were negative, and all 8 patients were discharged home. The estimated risk of missing MI using our protocol is, with 99% confidence, less than 5.1% and with 95% confidence, less than 3.6% (99% CI, 0–5.1%; 95% CI, 0–3.6%).
Conclusion
Application of an abbreviated cardiac enzyme protocol resulted in the safe and rapid discharge of patients presenting to the ED with cocaine-associated chest pain.
INTRODUCTION
In 2007 there were 2.1 million cocaine users leading to 64,000 emergency department (ED) visits to evaluate for possible myocardial infarction (MI).1 Approximately 57% of these patients were admitted to the hospital at an annual cost of $83 million.1 Cocaine use has significant cardiovascular complications, including myocardial infarction, arrhythmias, aortic dissection, hypertensive crises, cardiomyopathy, and endocarditis.
Cocaine is well absorbed through all body mucous membranes and can be administered through several routes. The onset of action varies from 3 seconds to 5 minutes depending on the route of administration. Also dependent on the route of administration are peak effects and duration of action, which vary from 1 to 20 minutes and 5 to 90 minutes, respectively.1
A 24-fold increased risk of MI has been reported within 1 hour of cocaine use and two-thirds of MI events occur within 3 hours of cocaine ingestion.2,3 However, Amin et al4 reported an 18-hour median length of time between cocaine use and MI onset among 22 patients presenting after cocaine ingestion. Other studies reported a range extending from 1 minute up to 4 days.3 The extended time frame may be secondary to metabolites that cause delayed or recurrent vasoconstriction.5
Generally accepted MI rates range from 0.7% to 6% of patients with cocaine-associated chest pain. These low rates of MI have prompted some hospitals to use observation units to reduce the number of admissions.6,7 In a prospective trial of 302 low- to intermediate-risk patients who underwent observation there were no cardiac deaths noted. Only 2% of patients sustained a non-fatal MI, and only 1% of patients sent home had a cardiac complication.8 Another retrospective review found that out of 187 patients observed in a chest pain unit, 87% were discharged and only 1% had a cardiac complication.9 A separate long-term prospective study found that out of 219 patients there was a zero rate of myocardial infarction at 1 year.10
Prior studies have demonstrated that low- to intermediate-risk patients with cocaine-associated chest pain can be safely discharged after 9–12 hours of observation.8 Additional literature suggests that in patients with undifferentiated chest pain, a rapid rule-out protocol using 2-hour delta CK-MB measurements is safe and effective.11,12 Therefore, our institution developed an abbreviated 8-hour cocaine-associated chest pain protocol for monitoring patients in the clinical decision unit (CDU). The goal of this study was to determine if patients treated with the 8-hour protocol were safely discharged from the CDU.
METHODS
This was an institutional review board approved (University of Florida College of Medicine, Jacksonville) retrospective review of patients treated in a CDU for cocaine-associated chest pain under the 8-hour protocol between May 1, 2011 and November 30, 2012.. To qualify for treatment in the CDU, patients had to be considered low to intermediate risk and meet the following inclusion criteria: 1) history of cocaine use within 72 hours; 2) normal EKG or EKG showing no acute changes and no left bundle branch block; 3) first set of cardiac markers (CK, CK-MB, and Troponin-T) negative; and 4) Thrombolysis in myocardial infarction risk score (TIMI) 0–3. We excluded patients if any of the following were true: 1) prior history of coronary artery disease (CAD), stents, or coronary artery bypass graft (CABG); 2) prior history of valvular disease, cardiomyopathy, or rhythm disturbance; 3) systolic blood pressure >160 or diastolic blood pressure >100 at time of transfer; 4) prior history of diabetes mellitus; 5) other causes of life-threatening chest pain; 6) active chest pain at time of transfer; 7) less than 18 years of age.
For patients who met inclusion criteria, the 8-hour protocol encompassed serial cardiac biomarker testing with Troponin T, CK-MB, and total CK at 0, 2, 4 and 8 hours after presentation to the ED. The rapid rule out protocol used delta CK-MB at 0, 2, and 4 hours to evaluate for a rise in CK-MB of 1.6 ng/mL for each 2-hour interval.11,12 A CK-MB >5 ng/ml with >5% fraction of the total CK was considered positive. Troponin-T was considered elevated if >0.04 ng/ml. If the patient’s cardiac biomarkers became positive at any point, the patient was consulted to the cardiology service and admitted for further workup. If cardiac enzymes remained negative, there was no change in the EKG, and the patient was free of chest pain or arrhythmia, the patient was discharged following the 8-hour observation period without additional testing.
We identified potential patients for inclusion in this study by reviewing the CDU chest pain log for patients treated between May 1, 2011 and November 30, 2012. Data collected on identified patients included initial vital signs, EKG findings, chest radiographs, cardiac biomarkers (Troponin-T, CK-MB, total CK), drug testing (if available), time of cocaine ingestion, disposition, and repeat visits for chest pain, adverse cardiac events or death within 30 days of CDU admission.
To determine death within 30 days, we searched hospital records for patient visits greater than 30 days after discharge from the CDU. For those who had not visited the hospital greater than 30 days post initial visit, we used the Social Security Death Index and Florida Vital Statistics databases to determine if patients expired and if death was within 30 days of treatment with the protocol. If the patient did expire, the cause of death was recorded. We reviewed charts for primary and secondary outcomes; primary outcomes were positive cardiac biomarkers, adverse cardiac events, or death within 30 days of discharge. Secondary outcomes were discharge versus admission and specialist consultations. If admitted, cardiac enzymes, stress testing, procedures, and discharge summaries were reviewed and recorded.
We entered the data collected into REDCap (Research Electronic Data Capture), hosted at the University of Florida and transferred to STATA12 (StataCorp LP, College Station, Texas). Frequency statistics were used to describe the study population and any chest-pain related care or death within 30 days of presenting to the ED. We calculated mean and standard deviations for numeric statistics. Exact 95% confidence intervals were provided by STATA 12’s cii command.
RESULTS
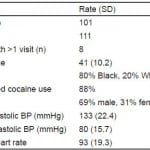
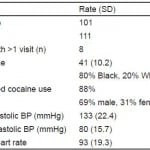
There were 101 unique patients comprising 111 admissions to the CDU for cocaine-associated chest pain during the study period. Eight patients had more than 1 visit; 1 patient had 4 visits and 7 patients had 2 visits each. Patient demographics are in Table 1.
Table 1. Demographics of 101 patients treated in clinical decision unit for cocaine chest pain.
BP, blood pressure
One patient had a delta CK-MB of 1.6ng/ml, but had negative Troponin-T at all time points. There were no patients with positive Troponin-T or CK-MB, notable EKG changes, or pertinent abnormal chest radiographs over the observation period (Table 2). Additionally, there were no myocardial infarctions and no deaths during the 30-day follow-up period. Most patients (103) were discharged home from the CDU, while 8 were admitted to the hospital. Of the 8 admitted patients, 2 had stress tests that were negative and 1 had additional cardiac biomarkers, which were also negative. All 8 patients were subsequently discharged home, and none were diagnosed with new cardiac disease or acute coronary syndrome upon discharge.
Table 2. Outcomes for 101 patients treated in clinical decision unit for cocaine chest pain.
None of the patients included in this study were found to have any of the primary outcomes (MI or death within 30 days); therefore, we were unable to determine the true sensitivity of our 8-hour protocol for ruling out MI in patients with cocaine-associated chest pain. However, the estimated risk of missing a patient with positive cardiac biomarkers, adverse cardiac event, or death within 30 days, using our protocol is almost surely less than 5.1% and most likely less than 3.6% (exact 95% CI, 0–3.6%; exact 99% CI, 0–5.1%) based on a zero event rate.
DISCUSSION
Cocaine-associated chest pain is a frequently encountered complaint in the ED, especially in urban inner city hospitals. In this study, the use of an ED observation unit for the monitoring and treatment of patients with cocaine-associated chest pain showed that an 8-hour protocol using delta CK-MB and frequent Troponin-T assays appears to be safe in patients who have used cocaine within 72 hours of presentation.
In general, the incidence of MI in cocaine users presenting with chest pain is low, and cocaine use does not predispose patients to coronary artery disease after adjusting for other risk factors.13,14 Because of this, low- to intermediate-risk patients with cocaine-associated chest pain can usually be observed in the ED without admission to the hospital. The use of ED observation units has allowed for the extended treatment of patients with cocaine-associated chest pain outside of the acute care area; however, bed space in observation units can be limited. Given the low risk of adverse cardiac events in this population it is reasonable to attempt to safely shorten the duration of observation for these patients.
Current evidence supports observation periods of 9 to 12 hours for low- to intermediate-risk cocaine-associated chest pain.8 Ruling out cardiac events more rapidly should involve the use of additional imaging, provocative testing, or more frequent serum biomarkers for detecting myocardial damage. Hendel and colleagues reported on the use of single-photon emission computed tomography myocardial perfusion imaging (MPI) in 151 patients with cocaine chest pain and found that it effectively ruled out cardiac events and lowered admission rates.15 Paraschin and colleagues applied cardiac CT angiography (CTA) in 24 cocaine users presenting with chest pain. They found that cardiac CTA was normal in 96% of patients, and positive in only 1 patient (4%) who had non-significant coronary stenosis.16 The use of imaging studies and/or provocative testing can expedite patient disposition; however, the risks of contrast allergies, contrast-induced nephropathy, and radiation exposure are all important considerations.
Our approach used a “rapid rule-out” protocol to safely and expeditiously rule out adverse cardiac events in patients presenting with cocaine-associated chest pain.11,12 This approach allowed for rapid disposition and discharge without radiation exposure from additional imaging or the resources required for provocative testing. In our cohort, only 2 patients required additional stress testing and 103 patients were discharged safely from the CDU after the 8-hour protocol. No patient experienced an adverse cardiac event, a positive provocative test, or positive additional cardiac biomarkers. Further, there were no deaths found in this cohort within 30 days of discharge. We believe we have demonstrated that the described 8-hour cocaine-associated chest pain protocol is safe and effective in this population.
LIMITATIONS
First, this retrospective study identified patients by reviewing the CDU chest pain logs. Although we performed a judicious search, the possibility of missing a small number of patients cannot be excluded. Second, the lack of positive cardiac biomarkers, adverse cardiac events, or deaths in our cohort limits our ability to make a true estimate about the sensitivity of the 8-hour protocol. However, we believe that our data give a realistic representation of patients who frequent urban EDs with complaints of cocaine-associated chest pain. Our data are reflective of the literature, in that the low- to intermediate-risk group of patients presenting with cocaine-associated chest pain has an inherently low rate of MI. Given our low estimated risk of no more than 5.1%, we feel it is safe to use our protocol in this population for the rule out of MI.
CONCLUSION
Our study demonstrated that an 8-hour abbreviated protocol safely ruled out MI in patients presenting to the ED with cocaine-associated chest pain. This protocol has the advantages of shortening ED length of stay, limiting radiation exposure, and reducing provocative testing.
Footnotes
Address for Correspondence: Faheem W. Guirgis, MD, 655 W 8th St, Jacksonville, FL 32209. Email: faheem.guirgis@jax.ufl.edu 3 / 2014; 15:180 – 183
Submission history: Revision received August 9, 2013; Submitted November 5, 2013; Accepted November 22, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Maraj S, Figueredo VM, Lynn Morris D. Cocaine and the heart. Clin Cardiol. 2010; 33:264-269.
2. Hollander JE, Hoffman RS. Cocaine-induced myocardial infarction: An analysis and review of the literature. J Emerg Med. 1992; 10:169-177.
3. Mittleman MA, Mintzer D, Maclure M, et al. Triggering of myocardial infarction by cocaine. Circulation. 1999; 99:2737-2741.
4. Amin M, Gabelman G, Karpel J, et al. Acute myocardial infarction and chest pain syndromes after cocaine use. Am J Cardiol. 1990;66:1434-1437.
5. Brogan WC, Lange RA, Kim AS, et al. Alleviation of cocaine-induced coronary vasoconstriction by nitroglycerin. J Am Coll Cardiol. 1991; 18:581-586.
6. Feldman JA, Fish SS, Beshansky JR, et al. Acute cardiac ischemia in patients with cocaine-associated complaints: Results of a multicenter trial. Ann Emerg Med. 2000;36:469-476.
7. Weber JE, Chudnofsky CR, Boczar M, et al. Cocaine-associated chest pain: How common is myocardial infarction?. Acad Emerg Med. 2000; 7:873-877.
8. Weber JE, Shofer FS, Larkin GL, et al. Validation of a brief observation period for patients with cocaine-associated chest pain. N Engl J Med. 2003; 348:510-517.
9. Kushman SO, Storrow AB, Liu T, et al. Cocaine-associated chest pain in a chest pain center. Am J Cardiol. 2000;85:394-396, A 10.
10. Cunningham R, Walton MA, Weber JE, et al. One-year medical outcomes and emergency department recidivism after emergency department observation for cocaine-associated chest pain. Ann Emerg Med. 2009; 53:310-320.
11. Fesmire FM, Percy RF, Bardoner JB, et al. Serial creatinine kinase (CK) MB testing during the emergency department evaluation of chest pain: Utility of a 2-hour deltaCK-MB of +1.6ng/ml. Am Heart J. 1998; 136:237-244.
12. Fesmire FM. Delta CK-MB outperforms delta troponin I at 2 hours during the ED rule out of acute myocardial infarction. Am J Emerg Med. 2000;18:1-8.
13. Chang AM, Walsh KM, Shofer FS, et al. Relationship between cocaine use and coronary artery disease in patients with symptoms consistent with an acute coronary syndrome. Acad Emerg Med. 2011;18:1-9.
14. McCord J, Jneid H, Hollander JE, et al. Management of cocaine-associated chest pain and myocardial infarction: A scientific statement from the american heart association acute cardiac care committee of the council on clinical cardiology. Circulation. 2008; 117:1897-1907.
15. Hendel RC, Ruthazer R, Chaparro S, et al. Cocaine-using patients with a normal or nondiagnostic electrocardiogram: Single-photon emission computed tomography myocardial perfusion imaging and outcome. Clin Cardiol. 2012; 35:354-358.
16. Paraschin K, Guerra De Andrade A, Rodrigues Parga J. Assessment of myocardial infarction by CT angiography and cardiovascular MRI in patients with cocaine-associated chest pain: A pilot study. Br J Radiol. 2012; 85:e274-278.