| Author | Affiliation |
|---|---|
| Brent W. Morgan, MD | Emory University, Department of Emergency Medicine and the Georgia Poison Center, Atlanta, GA |
| Carl G. Skinner, MD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, WA |
| Richard J. Kleiman, MD | Emory University, Department of Emergency Medicine and the Georgia Poison Center, Atlanta, GA |
| Robert J. Geller, MD | Emory University, Department of Pediatrics and the Georgia Poison Center, Atlanta, GA |
| Arthur S. Chang, MD | Emory University, Department of Emergency Medicine and the Georgia Poison Center, Atlanta, GA |
ABSTRACT
Objective:
Poisoning events, including exposures to hazardous materials, can involve multiple victims. Regional poison centers often are contacted in such events involving multiple victims.
Methods:
We searched our poison center database over a nine-year time period for all calls involving a poisoning event in which more than two people were exposed to the same substance. We then matched each product to the generic category used by the National Poison Data System. We analyzed this data to find the most frequent substances reported as primary substances in the multiple exposures.
Results:
We identified 6,695 calls between 2000 and 2008 that had more than two people exposed to the same substance. In these calls, 25,926 people were exposed (3.6% of the 715,701 human exposure calls for this period). These calls involved 64 of the 67 NPDS substance group codes. Some substances were much more commonly involved than others. The top three categories causing the most exposures were Fumes/Gases/Vapors, Food Products/Food Poisoning and Pesticides. Of the patients exposed, 69.4 % were not followed due to minimal effects possible or judged as nontoxic, 0.3% had major effects, 8.6% had no effects, and 9.3% had minimal to moderate effects. Eight people expired.
Conclusion:
Fumes, gases, and vapors make up the majority of multi-exposure calls. The overall mortality from multi-exposures, based on our data, is low. Analysis of these calls can help poison centers better understand these events and direct training.
INTRODUCTION
The United States has 60 poison centers serving its citizens.1 Poison centers provide medical advice to the lay public and healthcare personnel, most frequently following exposure to a drug or chemical or following a bite from an animal. In addition, poison centers gather information about the substance involved in the poisoning event as well as patient information. Some poisoning events can involve multiple patients.
Poisoning events that involve more than one person are categorized as multi-exposure incidents in our regional poison center data system (Call Tracking System, Jacksonville FL). The 2008 Annual Report of the American Association of Poison Control Centers reported that 9.7% of human exposures involved multiple patients.2 However, details about these exposures, such as substances and outcome, are not included in the annual report. The Duke Poison Control Center published a study about multi-exposure incidents in 1982.3 This study evaluated calls from one year (1977), only included patients less than 10 years old, and had 40 incidents, which limits what conclusion can be drawn. We undertook this study to help us understand the nature and epidemiology of multi-exposure incidents as reported to our regional poison center.
METHODS
The Georgia Poison Center keeps track of call data in an electronic database that is uploaded in near real-time to the National Poison Data System (NPDS). Data fields collected from each call include caller name, date, exposure substance, dose, circumstances, therapies received and outcome among others. We queried this dataset from Jan 1, 2000 to Dec 31, 2009 (n=715,701) for all events that were classified as multi-exposure. We excluded calls in which a substance could not be identified, and calls in which the exposure victims were non-human (such as pets or farm animals).
We defined a multi-exposure poisoning event as two or more victims exposed to the same substance at the same location over the same time period. For example, chemical fumes in building that affected three victims would qualify as a multi-exposure event. We analyzed these events using descriptive and categorical statistics to gain better understanding of these events. NPDS Medical Outcome categories were used to describe medical outcomes of the exposures.4 Minor effect: The patient developed some signs or symptoms as a result of the exposure, but they were minimally bothersome and generally resolved with no residual disability or disfigurement. Moderate effect: The patient exhibited signs or symptoms as a result of the exposure that were more pronounced, more prolonged or more systemic in nature than minor symptoms. Usually, some form of treatment is indicated. Symptoms were not life threatening, and the patient had no residual disability or disfigurement. Major effect: The patient exhibited signs or symptoms as a result of the exposure that were life threatening or resulted in significant residual or disfigurement. This study received approval from the local institutional review committee.
RESULTS
Over the nine-year period, our regional Poison Center received 715,701 exposure calls, of which 6,695 (0.9%) were classified as multi-exposure. The multiple exposure calls involved 25,962 patients, or a mean of 3.8 patients per multi-exposure event; 58% were female. Table 1 reports the age of the multi-exposure patients. Only 16,345 (63%) of the patients had definite ages documented; of these, 58% were less than 18 years of age. Seventy-nine percent of exposures occurred at residencies, 6% at workplaces, 5% public areas, 5% schools, 2% vehicles, 1% medical facilities, and in 2% unknown.
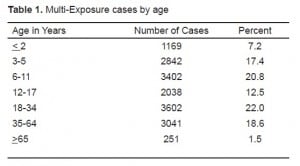
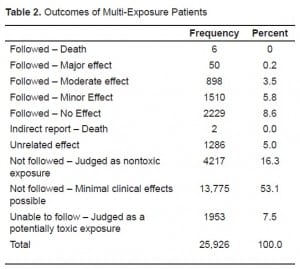
Table 2 shows the outcome of the multi-exposure patients. Of the patients exposed, 69.4 % were not followed because the poison center staff judged their exposure as at most minimal severity (either “minimal effects possible” or “nontoxic”), 8.6% had no effects, 9.3% had minimal to moderate effects, and 0.3% had major effects. There were eight fatalities, in which six involved a poisonous gas: three were from carbon monoxide, two from ammonia and one fatality from hydrogen sulfide. The deaths not related to gases were caused by hydrofluoric acid and an alleged malicious poisoning with ethylene glycol. The hydrogen sulfide and hydrofluoric acid deaths were occupationally related. The two ammonia fatalities occurred from a single event in which an accidental release occurred while the individuals were transporting anhydrous ammonia allegedly for illicit methamphetamine production.
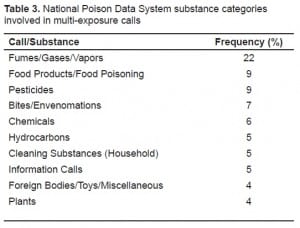
The poisoning events involved 64 of the 67 NPDS substance group codes. Table 3 lists the top 10 most common substances involved. The NPDS substance category gas/fumes/vapor was the number one substance involved in multi-exposure calls, involved in 22% of all calls.
DISCUSSION
The majority of multi-exposure calls to our poison center resulted in minimal or no health effects, and the overall mortality was low. The data suggests that the majority of these exposures can be safely managed without visiting a healthcare facility. Awareness or education about the safe handling of the substances in the gas/fumes/vapor category could make a significant contribution to injury prevention, since more victims potentially are involved in these cases.5,6
We found that the most common substance involved were gases, fumes or vapors. Gases have a variable volume and shape. Since they expand to fill available space, they potentially expose large numbers of people. This well-known property of gases/fumes/vapors is one of the reasons they are chosen as terrorist weapons.7 Analysis of the events that led to the release of the gas/fumes/vapor calls can help poison centers better understand these events and direct educational efforts for prevention. In addition, since these exposures were the most common sources of multi-person exposures, educational efforts should be directed to train healthcare providers in the medical care of patients exposed to these substances.
Our regional poison center has a close working relationship with our state government and performs several services (rabies triage and public health line) not typically associated with a poison center. These additional services may explain our relatively high percentage of calls involving food poisoning and bites/envenomations. An example of a multi-exposure event from the rabies triage line would be a family that found a bat in their residence. Poison centers performing these services can provide valuable information to the public and healthcare professionals, and could prevent an unnecessary healthcare provider visit. Preventive educational materials can also be developed in an attempt to decrease the incidents of these exposures.
LIMITATIONS
Our study only includes data from one poison center. Our specialized rabies triage and public health line may have influenced our data, making these results different from the experience of other populations.
CONCLUSION
Patients from multi-exposure poisoning events were more likely to be female and under 18 years of age. The most common substance category in multi-exposure poisoning events was Fumes/Gases/Vapors. Mortality and morbidity from these events was low.
Footnotes
Supervising Section Editor: Abigail Hankin, MD, MPH
Submission history: Submitted February 25, 2010; Revision Received April 1, 2010; Accepted April 15, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Brent Morgan, MD, Emory University, 50 Hurt Plaza Suite 600, Atlanta, Georgia 30303
Email: bmorg02@emory.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Data from American Association of Poison Control Centers Downloaded from www.aapcc.org on February 23, 2010.
2. Bronstein AC, Spyker DA, Cantilena LR, et al. 2008 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 26th Annual Report. Clin Tox.2009;47(10):911–1084.
3. Greenberg RS, Osterhout SK. Reported Multiple Victim Poisonings of Children. Clin Tox.1982;19(10):1073–80.
4. Bronstein AC, Spyker DA, Cantilena LR, et al. 2007 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 25th Annual Report. Clin Tox.2008;46(10):927–1057.
5. Heron RJ. Worker education in the primary prevention of occupational dermatoses. Occup Med.1997;47(7):407–10.
6. Nixon J, Spinks A, Turner C, et al. Community based programs to prevent poisoning in children 0–15 years. Inj Prev. 2004;10(1):43–6. [PMC free article] [PubMed]
7. Okumura T, Takasu N, Ishimatsu S, et al. Report on 640 victims of the Tokyo subway sarin attack.Ann Emerg Med. 1996;28:129–35. [PubMed]


