Original Research
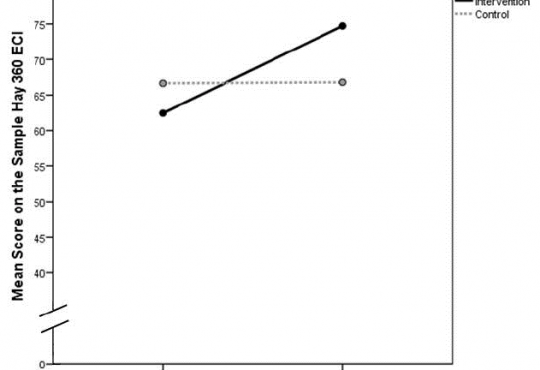
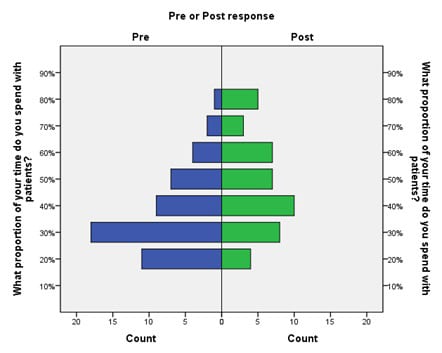
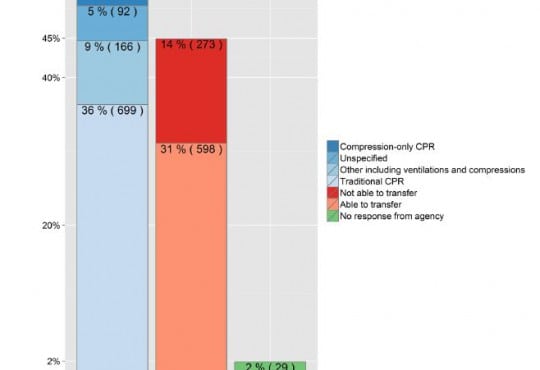
Emergency Department Operations
Scribe Impacts on Provider Experience, Operations, and Teaching in an Academic Emergency Medicine Practice
Westjem Read More
Emergency Department Operations
Identifying Patient Door-to-Room Goals to Minimize Left-Without-Being-Seen Rates
Westjem Read More
Treatment Protocol Assessment
Triple Rule Out versus CT Angiogram Plus Stress Test for Evaluation of Chest Pain in the Emergency Department
Westjem Read More
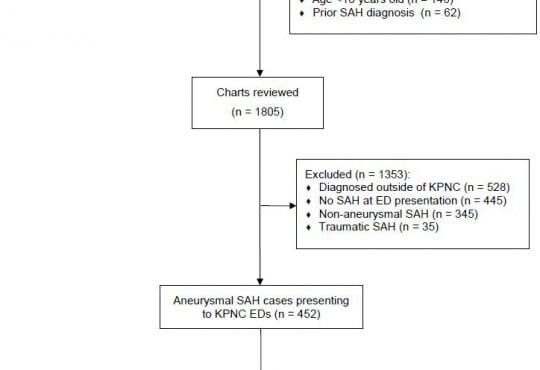
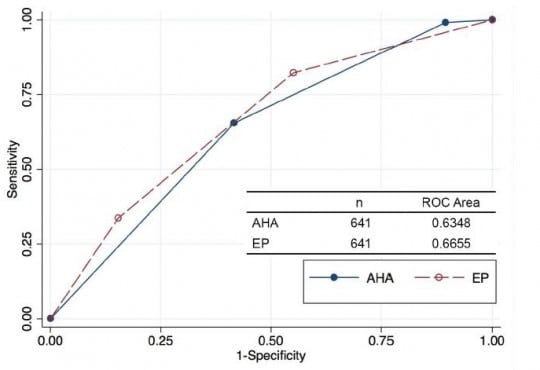
Treatment Protocol Assessment
Comparing an Unstructured Risk Stratification to Published Guidelines in Acute Coronary Syndromes
Westjem Read More
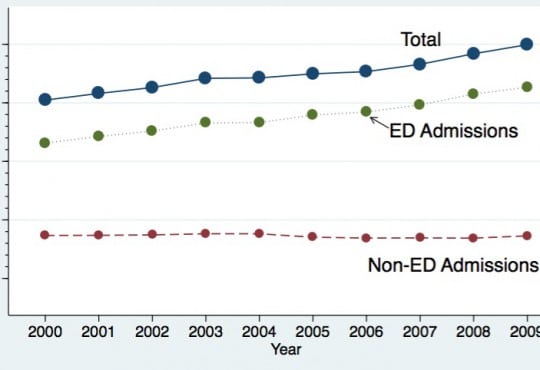
Emergency Department Access
Rural Ambulatory Access for Semi-Urgent Care and the Relationship of Distance to an Emergency Department
Westjem Read More
Treatment Protocol Assessment