| Author | Affiliation |
|---|---|
| Zachary Shinar, MD | Keck School of Medicine of the University of Southern California Medical Center |
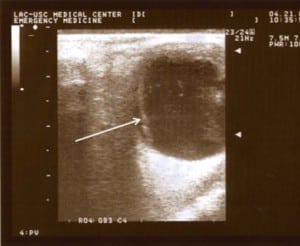
A 62-year-old Asian male with a past medical history significant for diabetes mellitus, hypertension, and prior surgical correction of a retinal detachment of the right eye presented to the emergency department (ED) for further evaluation of an abnormal examination by his optometrist. The patient denied any acute visual changes. On examination, corrected visual acuities measured 20/40 in the left eye and 20/100 in the right eye. Sclera, cornea, anterior chamber, and visual field examinations were unremarkable for both eyes, and retinal examination of the left eye was normal by undilated direct opthalmoscopy. ED ultrasound of both eyes revealed significant findings. In the right eye, a curved hyperdensity along the lateral aspect of the retina consistent with a prior surgically corrected retinal detachment was observed. In the left eye (Figure), a medial retinal detachment was noted. These images were generated by applying the 10 MHz linear ultrasound probe with water soluble gel directly on the closed eyelid. Picture quality and interpretation can be greatly improved by placing the probe slightly lateral on the eye, directing the beam medially in line with the optic nerve. Asking the patient to move his closed eye medial and lateral also allows the differentiation of a taught retinal detachment from a more freely moving vitreous hemorrhage.
This image demonstrates another emerging use for ultrasound in the ED: the evaluation for and diagnosis of a retinal detachment. As noted above, some patients with a retinal detachment may present with minimal visual complaints and subtle physical exam findings. Furthermore, direct ophthalmoscopy itself has limitations, especially when the pathology is distant from the macula. Diagnosing retinal detachment while the macula is still attached is particularly important, as permanent vision loss increases dramatically once this occurs. The improving resolution and increasing availability of ultrasound may assist emergency physicians in diagnosing this potentially devastating cause of vision loss.
Literature concerning ED ultrasound diagnosis of ocular pathology consists predominately of case reports1 with one prospective observational study2 showing ED physicians agreeing with a criterion standard on 98% of the cases. More studies concerning the accuracy of ED ultrasound diagnosis of retinal detachment are needed.
Footnotes
Submission history: Submitted June 21, 2007; Accepted November 26, 2007.
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for correspondence: Zachary Shinar, MD, Department of Emergency Medicine, LAC+USC Medical Center, Unit #1, Room 1011, 1200 N. State St., Los Angeles, CA 90033
Email: zshinar@hotmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Kahn An, Kahn Am, Corinaldi C. Retinal detachment diagnosed by bedside ultrasound in the emergency department. West J Emerg Med. 2005;6:47–51.
2. Blaivas M, Theodoro DL, Sierzenski PR. A study of bedside ocular ultrasonography in the emergency department. Acad Emerg Med. 2002;9:462b–463b.