Archives
Emergency Department Operations
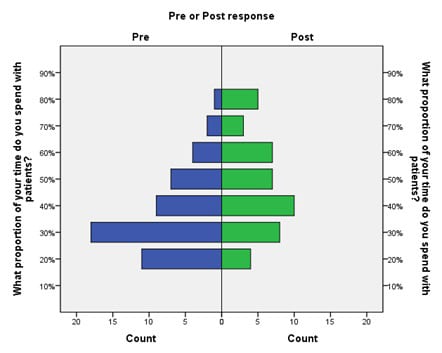
Scribe Impacts on Provider Experience, Operations, and Teaching in an Academic Emergency Medicine Practice
Westjem Read More
Emergency Department Operations
Identifying Patient Door-to-Room Goals to Minimize Left-Without-Being-Seen Rates
Westjem Read More
Treatment Protocol Assessment
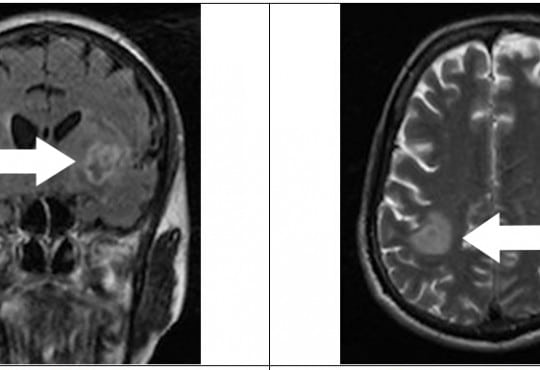
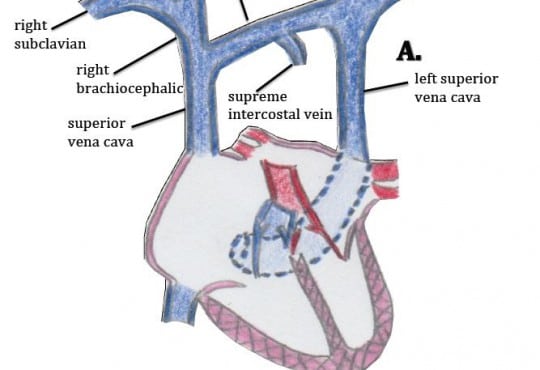
Triple Rule Out versus CT Angiogram Plus Stress Test for Evaluation of Chest Pain in the Emergency Department
Westjem Read More
Treatment Protocol Assessment