| Author | Affiliation |
|---|---|
| John W. Hafner, Jr., MD, MPH | University of Illinois, Department of Surgery, Peoria, IL |
| Joanna C. Gardner, MD | University of Illinois, College of Medicine, Peoria, IL |
| William S. Boston | Southern Illinois University, Department of Surgery, Springfield, IL |
| Jean C. Aldag | University of Illinois, College of Medicine, Peoria, IL |
ABSTRACT
Introduction:
Although other specialties have examined the role of the chief resident (CR), the role and training of the emergency medicine (EM) CR has largely been undefined.
Methods:
A survey was mailed to all EM CRs and their respective program directors (PD) in 124 EM residency programs. The survey consisted of questions defining demographics, duties of the typical CR, and opinions regarding the level of support and training received. Multiple choice, Likert scale (1 strong agreement, 5 strong disagreement) and short-answer responses were used. We analyzed associations between CR and PD responses using Chi-square, Student’s T and Mann-Whitney U tests.
Results:
Seventy-six percent of CRs and 65% of PDs responded and were similar except for age (31 vs. 42 years; p<0.001). CR respondents were most often male, in year 3 of training and held the position for 12 months. CRs and PDs agreed that the assigned level of responsibility is appropriate (2.63 vs. 2.73, p=0.15); but CRs underestimate their influence in the residency program (1.94 vs. 2.34, p=0.002) and the emergency department (2.61 vs. 3.03, p=0.002). The majority of CRs (70%) and PDs (77%) report participating in an extramural training program, and those CRs who participated in training felt more prepared for their job duties (2.26 vs. 2.73; p=0.03).
Conclusion:
EM CRs feel they have appropriate job responsibility but believe they are less influential in program and department administration than PD respondents. Extramural training programs for incoming CRs are widely used and felt to be helpful.
INTRODUCTION
The position of chief resident (CR) has been long regarded as important in physician residency training, with references as early as the late 1800s.1,2 The CR position is often seen as a bridge between the faculty and resident physicians, and individuals selected for chief are seen as resident leaders based upon their accomplishments, teaching skills, and overall personalities. The CR often balances multiple responsibilities, ranging from administrative duties, such as scheduling junior residents, to patient care, research and teaching medical students and fellow residents.1–4 Published reports from several sources suggest that although the administrative duties of the CR comprise a relatively large percentage of the CR’s time, the least amount of satisfaction is derived from these duties.5,6 Furthermore, recent trends may indicate that administrative duties are taking up a larger percentage of a CR’s time.6
The role of CR and its relation to academic medicine has been recognized in prior research. The position is often regarded as a stepping stone into an academic career in medicine and surgery. Despite the fact that it is an integral part of most training programs throughout the medical and surgical specialties, surprisingly little research is available regarding the CR position, especially within emergency medicine (EM) literature.7 EM CRs are appointed positions and do not simply reflect the last year of a resident physician’s training, as they do in some surgical specialties.7Perhaps because EM is a relatively young specialty, little has been published on the CR’s role. While EM has unique practice characteristics and relies heavily on off-service rotations for completing training of its trainees, we assume that the roles and responsibilities of the EM CR may resemble those of other training specialties. With this in mind, we sought to define the current demographics as well as the training and responsibilities held by EM CRs throughout residency programs in the United States. We also explored the concordance of the CR’s and PD’s viewpoint of the training, expectations and influence of the position.
METHODS
Study Design and Population
A structured anonymous written survey was mailed to each of the 124 Residency Review Committee-approved EM programs for 2002. To compare and contrast opinions between populations, we distributed a parallel survey of CRs (up to four per program) and their PDs. The catalog of EM residencies provided by the Society for Academic Emergency Medicine (SAEM) was the source of the correspondence addresses. This study was reviewed and approved by our local Institutional Review Board prior to initiation.
Survey Content and Administration
Because no prior survey of EM CRs has been performed, the authors developed the survey instrument. The survey consisted of a 28-question CR instrument and a 27-question PD instrument, focusing on the demographics, training and responsibilities of the current CRs. Residency program faculty and former CRs reviewed the instruments for face validity, and we then we revised for clarity. The survey utilized multiple-choice, Likert scales (1, most positive; 5, most negative) and open-ended questions. No survey questions were strictly open-ended, as they reflected additional information provided by respondents for an “other” response in a multiple- choice format question. We reviewed these answers, and if by investigator consensus we discerned a distinct pattern, an additional answer category was reported. Subjects also occasionally provided unsolicited comments to questions. We attempted to incorporate these into our results whenever logically possible. A follow-up mailing was sent six weeks after the first to those programs that had not initially responded. We sent several reminder e-mails to the CRs who used the Emergency Medicine Residents’ Association (EMRA) CR e-mail list serve, and to the PDs using the published SAEM e-mail listing. Each survey was filled out anonymously and returned in a postage-paid envelope to the investigators. We encoded the surveys with a randomly generated study identification number that corresponded to each specific EM program, allowing reminder letters to be mailed without compromising anonymity.
Demographic queries included age, gender and educational background. EM residency program demographics included the length of the program, program type (PGY 1-2-3, 1-2-3-4 or 2-3-4), number of annual CRs, the annual number of accepted resident physicians and the length of the CR term. We also queried about the process for choosing and training CRs, as well as which PDs had served as CRs and found the position beneficial.
Data Analysis
We analyzed responses using SPSS v11.0 (SPSS Inc., Chicago IL), and used descriptive statistics to summarize demographic data. Associations between CR’s and PD’s responses were sought using the Chi-Square test, student T-test and Mann-Whitney U test for nominal, ordinal and interval variables, respectively. We defined statistical significance as p<0.05. We also conducted a content analysis of open-ended questions.
RESULTS
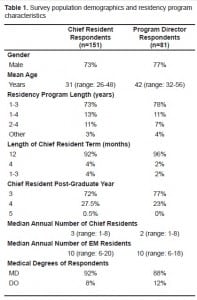
One hundred fifty-one CRs (representing 76% of total U.S. EM programs) and 81 PDs (representing 65% of total U.S. EM programs), returned completed surveys. Sixty-four programs (51.6% of total U.S. EM programs) had responses from both the PD and a CR. When we compared individual demographic factors and program characteristics of the CR and PD respondents, no significant demographic differences existed aside from age (Table 1). Most CRs are between the ages of 26 and 35 (mean age 31), while most PDs are between 36 and 50 (mean age 42). The majority of PDs (77%) and CR respondents (73%) were men. The majority of EM CRs complete their duties during the last year of their EM residency, with a few programs requiring additional training time. EM residency programs appoint one or more CRs for a term of 12 months, and rotating positions are rare (2% of CR respondents, 4% of PD respondents). Eighty-six percent of CR and PD respondents had MD degrees (Table 1). Fifty-six percent of CRs and 59% of PDs reported that they filled the CR position based on a combination of faculty, program director and resident input (Table 2).
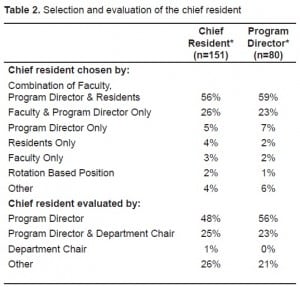
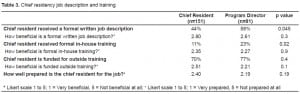
Significant differences were reported in the training experiences for CRs between CRs and their PDs. Forty-four percent of CRs reported that they received a formal written job description, while 58% of PDs reported distributing one (p=0.045). Of CRs, only 11% reported participating in a formal intra-institutional training program, while 23% of the PDs reported offering one (p=0.02). The majority of CRs (70%) and PDs (77%) reported participation in a formal extra-institutional training program prior to assuming the CR role. The most common extra-institutional training program was the EMRA Chief Resident Forum, a one-day didactic and interactive forum held annually during the American College of Emergency Physician (ACEP) Scientific Assembly. The majority of intra-institutional training reported was a formal job orientation, most often conducted by residency faculty and the PD. Both groups felt that a job description and training was beneficial, and that overall CRs were prepared for the position (Table 3). When responses were stratified by orientation and training, CRs who received a written job description reported feeling more prepared for their position than those who did not (mean Likert scale 2.23 vs. 2.53, p=0.047). Those CRs that had received extra-institutional training reported feeling better prepared for the position compared to those who had not participated in such a program (mean Likert scale 2.26 vs. 2.73, p=0.03). PDs also reported that residents participating in extra-institutional training were more prepared for CR duties (mean Likert scale 2.08 vs. 2.56, p=0.01).
PDs and CRs agreed that the level of responsibility given to the CR was appropriate (2.63 vs. 2.73, p=0.15). However, PDs found the position more influential than the CRs in effecting change in the residency program (mean Likert scale 1.94 vs. 2.34, p=0.002) and the ED (mean Likert scale 2.61 vs. 3.03, p=0.002). Both groups agreed that fellow residents and faculty are supportive of the CR, but that university and hospital administrators are not helpful.
Gender did not affect responses in the majority of the survey questions. However, a few important distinctions exist. Female CRs felt significantly less prepared to perform the duties than their male counterparts (mean Likert score 2.77 vs. 2.28, p=0.001). Female CRs also found PDs to be less helpful than their male counterparts (mean Likert score 1.7 vs. 1.4, p=0.03). Female PDs also reported the faculty was less supportive of the CRs, as compared to male PDs (mean Likert score 2.38 vs. 1.85, p=0.02).
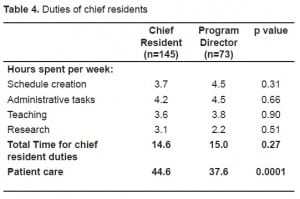
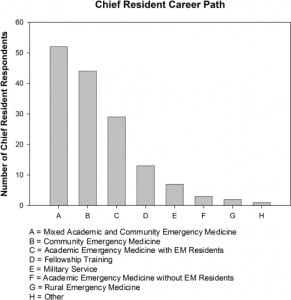
Most CRs receive a benefit for holding the position, with fewer shifts and increased salary/stipend as the most commonly offered. PDs and CRs had similar estimations of time spent on each duty of the CR (13–15 hours per week on average); however, PDs underestimated CRs’ time spent on patient care (44.1 vs. 37.5 hours/week, p=0.001) (Table 4). The majority of CRs would recommend the job to fellow residents, believe that the position is helpful to their career and would choose to be CR again. Those PDs who had at one time held a CR position felt stronger than current CRs that they would choose the job again (mean Likert score 1.35 vs. 1.87; p=0.007). Most CRs responded that they planned on pursuing careers in an academic, mixed academic and community hospital, or a community medicine setting (Figure 1).
DISCUSSION
After compiling data from the participating CRs and PDs, we are able to describe the general demographics of EM CRs and their position requirements. Most chiefs are male, with an allopathic medical degree, and generally hold the position for 12 months during the last year of their training. They are required to perform multiple academic and administrative duties, and usually receive some form of benefit for the 13–15 hours per week this requires. In general, the CR position is filled by a combination of faculty, PD and resident input; however, the PD is usually the sole evaluator of the CR. This is consistent with previous reports from the published literature of other medical specialties.3,6–8
By surveying both the CRs and PDs, a comparison between their opinions is offered on a variety of issues. While we found consistencies between the two groups, we discovered that several differences also exist. Although CRs and PDs perceive different amounts of job description and formal training given, both agree that chiefs receiving formal extra-institutional training are better prepared to perform the assigned duties compared to those who do not. This finding is mirrored in previous CR literature from other medical specialties as well, and other authors have proposed formal training programs in other specialties.9,10 Kim et al.11 noted in a survey of former pediatric CRs that only 37% had received some form of an orientation with 54% in the form of a workshop or seminar, while others had verbal training from outgoing CRs, chairpersons or PDs. In a survey of family practice CRs, 70% received no formal training and 19% participated in an extra-institutional training program.12 The most common venue for EM CR extra-institutional training reported was the EMRA Chief Resident Forum, offered annually at the ACEP Scientific Assembly.13 The daylong workshop offers training in conflict resolution, leadership training, bedside teaching, and tips from former CRs. The workshop uses formal didactic lectures, small groups and panel discussions. While a causative relationship cannot be determined by this type of research methodology, these responses suggest that should further development of extra-institutional formal training programs occur, the time and funding to send residents to these programs is important. If validated, the development of extra-institutional formal training programs may help to unify the CR position among EM residency programs, as well as other medical specialties.
CRs and PDs have varied opinions regarding the level of influence held by the CR. In general, CRs perceive themselves as less influential than PDs do in effecting change throughout the residency program and the ED, although both agree that the CR has power to make changes in program policies. While reasons for this difference are unclear from this survey, this may represent a need for better communication and feedback between PDs and CRs. Despite the differences in perceived influence, both CRs and PDs felt that the university and hospital administration are not as supportive as they could be. While the importance of this deficit is not known, there may also be an opportunity for improved communication between PDs, department chairs and administrators.
Little research exists regarding the CR position as a whole,1,2,4–9,11 and even less for EM;7however, many of our survey points reinforce previous findings. The majority of respondents indicated that the EM CR position is incorporated into the standard EM residency and no additional training time is allocated. Although limited medical specialty studies exist, this pattern is similar to reports from family practice 12 and pediatrics.14 EM CRs spent over 15 hours per week on chief duties and also had to perform similar academic and clinical duties as their peers. Previous surveys have noted similar trends in CR workloads and the desire for more time devoted to teaching and research and less time allotted for scheduling and administrative duties.11,12 PDs who had previously been a CR, as well as current CRs, found the position satisfactory enough to do it again if given the opportunity. Although follow-up data is unavailable, many of the respondent CRs were planning on pursuing a career in an either academic or mixed academic and community medicine setting, suggesting that a CR position prepares individuals for an academic emergency medicine career, an opinion supported in the literature of other specialties.14
Gender differences in other specialty CRs appear to exist as well in EM. Female EM CRs report less preparedness and PD support. Interestingly, female PDs recognize this and feel less faculty support of CRs as well. Consistent with other limited published findings among psychiatry CRs, this suggests further obstacles for women in EM, especially in academic careers.15 Further research is warranted in exploring gender differences in EM training programs and academic emergency medicine.
LIMITATIONS
This study has some limitations worth noting. We achieved a limited response rate (CR responses represented 76% of U.S. EM residency programs and PD responses represented 65% of U.S. EM residency programs); therefore, our reported results may not reflect those of the non-respondents. No data could be collected on survey non-responders to identify any differences with survey responders. In addition, not all surveys were completed in their entirety. This survey is also subject to recall bias, especially when attempting to quantify time spent performing specific duties or the amount of support felt from administration and faculty. Using an EM CR list serve to identify potential participants could have introduced selection bias, as these individuals may have been different from those not represented on the list serve. Because no previously validated survey of CRs had been compiled, the survey was developed by the study’s authors. Although the study was tested for face validity and clarity by resident faculty and former CRs, it was not formally assessed for performance of the questionnaire. Survey results were analyzed using aggregate CR and PD populations, and data were not linked to specific programs or individuals. While these results give a general overview of the EM CR position, they may not be applicable to individual locations. The results of this survey reflect a cross-sectional descriptive overview of the CR position in EM. The associations noted in this study do not reflect a causative relationship, as multiple additional variables and confounders may be responsible. Further research with different methods would be required to determine causation of these findings. Finally, gender differences noted may be influenced by prior social and academic events experienced outside of the role of CR or PD.
CONCLUSION
CRs in EM most often represent male allopathic physicians appointed in the last year of residency training by a combination of the PD, faculty and residents, for a term of 12 months. Resident physicians who undergo formal training, particularly from an extra-institutional source, feel more prepared for the role of CR. Most would recommend the position and would choose to be CR again. Further research into why female CRs and PDs sense less support in their field of academic EM is indicated.
Footnotes
Supervising Section Editor: Laleh Gharahbaghian, MD
Submission history: Submitted September 4, 2009; Revision Received February 8, 2010; Accepted February 15, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: John W. Hafner, MD MPH, Department of Emergency Medicine, OSF Saint Francis Medical Center, 530 NE Glen Oak Dr, Peoria, IL, 61637
Email: jhafner@pol.net
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Grant I, Dorus W, McGlashan T, et al. The chief resident in psychiatry. Arch Gen Psychiatry.1974;30(4):503–7. [PubMed]
2. Nelson CS, Brown IE, Rao TK. A study of the responsibilities of chief residents in anesthesiology with a suggested job description. Anesthesiology Review. 1994;21(6):199–202. [PubMed]
3. Norris T, Susman J, Gilbert C. Do program directors and their chief residents view the role of chief resident similarly? Fam Med. 1996;28:343–5. [PubMed]
4. Doughty RA, Williams PD, Seashore CN. Chief residency training. Developing leadership skills for future medical leaders. AJDC. 1991;145:639–42. [PubMed]
5. Wortman RL, Costrini NV, Adams ND. The chief medical residency: a description and recommendations. J of Med Educ. 1982;57(4):288–93. [PubMed]
6. Young MA, Stiens SA, Hsu P. Chief residency in PM&R, a balance of education and administration.American Journal of Physical Medicine and Rehabilitation. 1996;75(4):257–62. [PubMed]
7. Playe SJ, Squillante MD, Durkin L, et al. Chief residency in emergency medicine. Acad Emerg Med.1998;5(5):448.
8. Ticknor CB, Matthews KL. A model for selecting a psychiatry chief resident. J Med Educ.1988;63:333–5. [PubMed]
9. Wilder JF, Plutchik R, Conte HR. The role of the chief resident: expectations and reality. Am J Psychiatry. 1976;133(3):328–31. [PubMed]
10. Colenda CC. The psychiatry chief resident as information manager. J Med Educ. 1986;61:666–76.[PubMed]
11. Kim SC, Giardino AP, Casey R, et al. Experiences and reflections of former pediatric chief residents. Arch Pediatr Adolesc Med. 1994;148:518–21. [PubMed]
12. Susman J, Gilbert C. Family medicine residency directors’ perception of the position of chief resident. Acad Med. 1992;67:212–3. [PubMed]
13. Emergency Medicine Resident’s Association. Scientific Assembly 2006-EMRA Activities Website. Available at: http://www.emra.org/Index.cfm?FuseAction=Page&PageID=1002196; Accessed February 20, 2007.
14. Alpert JJ, Levenson SM, Osman CJ, et al. Does being a chief resident predict leadership in pediatric careers? Pediatrics. 2000;105(4 Pt 2):984–8. [PubMed]
15. Kessler MD, Hellekson-Emery C, Wilder JF. The psychiatric chief resident: does gender make a difference? Am J Psychiatry. 1982;139(12):1610–3. [PubMed]


