| Author | Affiliation |
|---|---|
| Robert H. Birkhahn | New York Methodist Hospital, Department of Emergency Medicine, Brooklyn, NY |
| Andra Blomkalns | University of Cincinnati, Cincinnati, OH |
| Howard Klausner | Henry Ford Hospital, Detroit, MI |
| Richard Nowak | Affiliation |
| Ali S. Raja | Brigham and Women’s Hospital, Boston, MA |
| Richard Summers | University of Mississippi Medical Center, Tupelo, MS |
| Jim E. Weber | University of Michigan, Hurley Medical Center, Flint, MI |
| William M. Briggs | New York Methodist Hospital, Department of Emergency Medicine, Brooklyn, NY |
| Alp Arkun | New York Methodist Hospital, Department of Emergency Medicine, Brooklyn, NY |
| Deborah Diercks | University of California, Davis Medical Center, Davis, CA |
ABSTRACT
Introduction:
Financial conflicts of interest have come under increasing scrutiny in medicine, but their impact has not been quantified. Our objective was to use the results of a national survey of academic emergency medicine (EM) faculty to determine if an association between money and personal opinion exists.
Methods:
We conducted a web-based survey of EM faculty. Opinion questions were analyzed with regard to whether the respondent had either 1) received research grant money or 2) received money from industry as a speaker, consultant, or advisor. Responses were unweighted, and tests of differences in proportions were made using Chi-squared tests, with p<0.05 set for significance.
Results:
We received responses from 430 members; 98 (23%) received research grants from industry, while 145 (34%) reported fee-for-service money. Respondents with research money were more likely to be comfortable accepting gifts (40% vs. 29%) and acting as paid consultants (50% vs. 37%). They had a more favorable attitude with regard to societal interactions with industry and felt that industry-sponsored lectures could be fair and unbiased (52% vs. 29%). Faculty with fee-for-service money mirrored those with research money. They were also more likely to believe that industry-sponsored research produces fair and unbiased results (61% vs. 45%) and less likely to believe that honoraria biased speakers (49% vs. 69%).
Conclusion:
Accepting money for either service or research identified a distinct population defined by their opinions. Faculty engaged in industry-sponsored research benefitted socially (collaborations), academically (publications), and financially from the relationship.
INTRODUCTION
With healthcare spending now 15% of the United States (US) economy, it is no surprise that pharmaceutical companies are spending in excess of seven billion dollars annually to market their products to physicians.1,2 The topic of physician-industry relations has been debated in depth over the years in countless articles and, although still a controversial issue, academic medical societies have published guidelines with regard to the activities of their members.
This trend has been amplified by recent media coverage of unprincipled activities involving some of the most prestigious medical societies in the US. The American Heart Association and the American College of Cardiology, for example, recently were criticized for their revisions of guidelines outlining increased use of statins. It was discovered that seven of the nine members who drafted the guidelines had personal financial arrangements with drug manufacturers.3 These financial relationships result in an appearance of impropriety that undermines the public’s trust in medicine as an institution.4,5
Although the effects of industry-physician relations on professional behavior and prescribing patterns have been addressed by both opinion surveys and commentary, the impact of money has not been objectively studied.6–11
The reporting of financial conflicts of interest has become commonplace in all areas of academic medicine, although the exact meaning of those conflicts remains to be understood. This study utilizes the results from a recent survey of the Society of Academic Emergency Medicine (SAEM) membership to determine if an association between money and personal opinion exists.
METHODS
Study Design
We designed a survey instrument using a web-based format and implemented it during a three-week period in 2007. The instrument was based on a New England Journal of Medicine article outlining physician-industry relations based on specialty and was adapted for use by the SAEM.12 After adaptation the survey was reviewed in a small focus group setting comprised of faculty from a single institution. The instrument was then reviewed further by 10 representatives from different academic institutions for validity and aptness (Industry Relations Committee, SAEM, 2007). After appropriate changes were made to the questionnaire, we submitted it to the Board of Directors of SAEM for final approval. The study protocol met criteria for exemption from review by the Institutional Review Board at the first author’s institution.
Setting/Selection of Participants
The data source for this study was the national membership of SAEM, 3,183 individuals. Via e-mail we contacted those who had previously provided their information to the society. If they expressed interest in participating, the e-mail routed them to the appropriate web-based questionnaire. We sent follow-up e-mails requesting participation for three weeks after the initial mailing.
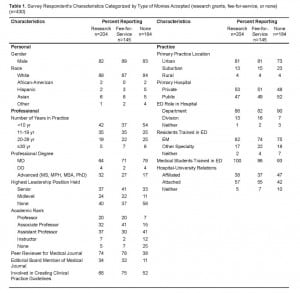
Data Collection and Processing
The questionnaire collected demographic information on the participants, including personal and professional characteristics. Personal characteristics included gender and race. Professional characteristics included number of years in practice and role as a peer reviewer, editor, or clinical guidelines contributor. Additional professional characteristics included degrees held, current leadership positions within their program, and academic rank. Highest leadership position was reported as senior (chair, vice-chair or equivalent, program director or research director), or midlevel (all others). The final demographic recorded dealt with practice characteristics and included the location (urban, suburban, or rural), type of hospital (private or public), emergency medicine (EM) departmental status, and academic affiliation. Finally, respondents included if residents (EM, other, neither) and medical students trained in their departments.
The next part of the survey asked 17 yes/no questions dealing with specific faculty-industry relationships. The data was directly linked to fields in a Microsoft Excel spreadsheet compiled by the SAEM administrative offices. The website did not close the HTML page after the respondent clicked “submit.” For this reason, some duplicate questionnaires were identified. We used a structured data-cleaning algorithm to count the number of unique and repeat answers.13
Outcome Measures/Primary Data Analysis
Research Grants
Participants were asked what, if any, percentage of research funding they received from public, private, industrial, or intramural sources in the preceding year. Those who reported a percentage for any of these sources were classified as having received research funding; otherwise they were classified as not having received funding.
Fee-for-service
The second category included respondents who accepted monies for intellectual-based services. Participants were asked whether they had received payments from industry within the preceding year for consulting work or for serving as a speaker or on an advisory board. An affirmative response in any of the three categories was sufficient to classify respondents as having accepted fee-for-service money from industry.
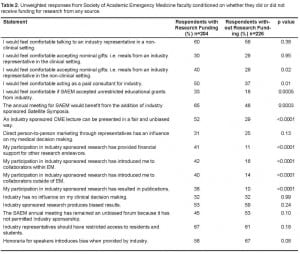
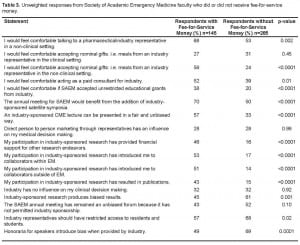
On a number of opinion questions (see Tables 2 and and3)3) a Likert scale was used. For conciseness, responses to each of these questions were then split into two categories, either strongly agree or agree vs. all other responses. We then compared the percentages in the affirmative category between the groups of people receiving research funding or not and the groups of people receiving fee-for-service money or not. Then we calculated chi-squared tests of differences in the proportions, and reported a p-value on the difference. There were no corrections made for multiple testing.
RESULTS
A total of 655 surveys were completed after a three-week period in 2007. Of these, 225 responses were discarded due to duplication, leaving viable responses from 430 members who represented 14% of the 3,183 active members of SAEM. There was no difference between duplicate and unique responses in our sample. Respondent demographics are in Table 1. In our sample, 51% of respondents reported receiving research funding from any source; 23% reported receiving research grants from industry, 31% from private sources, 35% from public funds, and 25% from intramural sources within the last year. One-third of respondents (34%) reported money coming from industry for fee-for-service work in the preceding year.
The results of our chi-squared test for respondents receiving research grants are summarized in Table 2. Respondents who received research money from any source were more likely to be comfortable accepting gifts (OR 1.6, 1.05–2.3) and acting as paid consultants (OR 1.7, 1.1–2.5). They were also more likely to agree that SAEM should accept educational grant money from industry (OR 2.3, 1.5–3.6), that the annual meeting would benefit from satellite symposia (OR 2.0, 1.4–3.0), and that industry-sponsored continuing medical education (CME) could be fair and unbiased (OR 2.4, 1.6–3.6). These findings held true even when only respondents holding research grants from industry were analyzed against all others. The responses from faculty with research grants from industry were the same as those with research grants from all other sources. The one exception was that respondents with research money from industry agreed that industry-sponsored research was biased only 38% of the time, as opposed to 66% of the time for respondents receiving research grants from all other sources.
Respondents who accepted fee-for-service money from industry for activities other than research had similar opinions to those who received research money (Table 3). Additionally, these respondents were more likely to agree that industry-sponsored research produces fair and unbiased results (OR 0.51, 0.34–0.77). Conversely, they were less likely to believe that industry-provided honoraria introduce bias for speakers (OR 0.43, 0.28–0.65) and that industry representatives should have restricted access to residents and students (OR 0.62, 0.41–0.94).
Faculty who received funding for either research or fee-for-service activities were more likely to agree that their participation in industry-sponsored research has allowed them to receive financial support for other research endeavors, introduced them to collaborators within and outside EM, and has resulted in publications (OR 2.5, 2.3–2.8).
DISCUSSION
We demonstrate that industry interactions with a medical society (SAEM) are viewed more favorably by members receiving funds for research, as well as industry-sponsored fee-for-service activities. It is important to note that the source of research money was unimportant; with the exception of whether or not the respondents believed industry-sponsored research to be biased. The same observation cannot be made for fee-for-service activities since our survey did not specifically include any fee-for-service activities not sponsored by industry.
Although causality cannot be determined from our sample, the association we find between money and opinions can be interpreted in a variety of different ways. One way to view these findings is that money buys influence, and the exchange of money for service imparts a more favorable view of the client (industry) on the provider. The problem with this view is that differences in opinion do not extend beyond the societal level to individual physician-industry interactions in our sample. The opposing viewpoint may ascribe the differences seen in our survey to lack of money rather than the presence of it. Perhaps faculty without compensation or funding are not so by choice, and are motivated more by resentment in their view of industry interaction. A more moderate way to explain our findings is that experience with the requirements and expectations of a financial relationship to industry results in a familiarity and acceptance of the process. Faculty who accept payment or funding from any source might be expected to be comfortable with the ramifications of such an interaction at the societal level. Regardless of why it exists, it is clear that accepting payment or funding defines a distinct subset of faculty members with regard to their opinions.
Our study centered on the relationship that exists when payment is provided for intellectual service or research, as opposed to the gift-recipient relationship. Social theory holds that the act of gift giving creates a social bond with an obligation to reciprocate on the part of the recipient. A recent study by Halperin et al.6 found that radiation oncologists who accepted gifts of high value from industry representatives were more likely to be sympathetic toward this practice. The obligatory relationship of the gift relationship with regard to physician-industry interactions has been explored even for trivial gifts, but little has been said about whether an independent contractor relationship produces similar obligations.
It seems clear from our survey that faculty-industry interactions involve more than just money. In our sample, roughly 40% of faculty receiving research funding agreed that industry-sponsored trials resulted in publications, financial support for other research activities, or professional collaboration. This number is even higher for faculty participating in fee-for-service activities with industry, with more than half receiving a benefit beyond just money. These are tangible benefits that make industry interactions an important component of academic advancement, and should not be dismissed as imparting insignificant influences on academic faculty. A recent survey published in theJournal of the American Medical Association showed that more than half of department chairs with ties to industry believed that a positive relationship exists and the support received from industry plays “an important role in the education and research missions of academic centers.”14
Although it is reassuring that those who conduct industry-sponsored trials are no more likely than their faculty counterparts to believe that industry sponsored is biased, it is concerning that those who participate in fee-for-service activities (speakers, consultants, or advisors) are less likely to believe that their participation may bias their perception (45% vs. 61%). It is also not surprising that those who receive fee-for-service money from industry are more likely to feel that industry-sponsored CME can be presented in a fair and unbiased manner. This may be due to unrecognized bias or increased knowledge of the process.
The recent media spotlight on medical societies, as well as individual physicians’ relationships with the pharmaceutical and biotechnology industry, has forced some to take a closer look at current practice guidelines and question the nature of these interactions.2,3,8–11 With the traditional physician guise of nonmaleficence, fidelity, justice, and self-improvement at stake, professional associations have moved to update their guidelines regarding the acceptance of money from industry. However, in a paternalistic system where physicians often believe that their peers are susceptible to the influences of industry and they themselves are invulnerable, discussing financial relationships and opinions remains a delicate topic with causality difficult to establish.2,14
An article published in the Canadian Medical Association Journal outlined particular interactions between physicians and the pharmaceutical industry, including CME conferences.9 They concluded that industry-sponsored CME events could be biased and influence physicians even after conforming to guidelines designed to prevent such occurrences. It is of interest to note that this study came out after SAEM, the American College of Physicians, and the American Medical Association implemented updated physician-industry relations guidelines, including appropriate industry support for CME conferences.15–17
LIMITATIONS
The sampling strategy used was less than ideal and created a potential for sampling bias. The survey was administered to all active SAEM members, so that they could provide input to the Board of Directors for future interactions between SAEM and industry. As such, we were more likely to receive responses from members who had formed opinions. The demographics of our responding faculty are in line with previously reported physician survey samples and suggest that we received responses from an academically diverse selection of members.
The poor sample response rate of 14%, linked with a broad, non-random sampling strategy, resulted in a survey response that was deemed inadequate for representing the opinions of SAEM as a whole. This is why the current manuscript emphasizes the relationship between opinion and the self-reported receipt of monies, as opposed to the opinions in and of themselves. In this case, having a sample split evenly between those who did and did not receive funding is ideal for the analysis. This still remains subject to self-selection bias, as the response rate further emphasizes that the respondents were not random.
It is not possible from our survey design to determine if respondents’ opinions were a result of either their research grants or fee-for-service activities, or if respondents merely participated in those activities because their pre-formed opinions allowed them to do so. It is beyond the scope of this survey to determine which came first, opinion or money. The important point from our work is that the mere fact that a faculty member has received money for any reason defines a distinct subset with regard to their personal opinions. We only assessed opinions regarding bias and the intrinsic value of various relationships. The survey instrument was not derived to show the existence of actual bias in clinical or academic decision-making, only the perception of bias.
CONCLUSION
In our sample, receiving money for either service or research identified a distinct group of faculty defined by their opinions. Our results also point out that faculty engaged in industry- sponsored research were likely to benefit socially (via collaborations), academically (via publications), and financially from the relationship. The pharmaceutical and biotechnology industry is a business, and as such it imparts these benefits to physicians with expectations of fiscal returns. Academic faculty must carefully consider the impact of these benefits when weighing the pros and cons of physician-industry interactions and realize the impact that they may have on opinions.
Footnotes
Supervising Section Editor: Eric D. Isaacs, MD
Submission history: Submitted May 11, 2009; Revision Received October 5, 2009; Accepted October 31, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Robert H. Birkhahn, MD, Department of Emergency Medicine, New York Methodist Hospital, Brooklyn, NY 11791
Email: rhbirkhahn@pol.net
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Drum K. Political Animal. Washington Monthly. 2004 Jul 14;
2. Chimonas S, Brennan TA, Rothman DJ. Physicians and drug representatives: exploring the dynamics of the relationship. J Gen Intern Med. 2007;22(2):184–90. [PMC free article] [PubMed]
3. Kassirer JP. Professional societies and industry support: what is the quid pro quo? Perspect Biol Med. 2007;50(1):7–17. [PubMed]
4. Blake RL, Jr, Early EK. Patients’ attitudes about gifts to physicians from pharmaceutical companies. J Am Board Fam Pract. 1995;8(6):457–64. [PubMed]
5. Randall T. Kennedy hearings say no more free lunch–or much else–from drug firms JAMA 1991.26544402. [PubMed]
6. Halperin EC, Hutchison P, Barrier RC., Jr A population-based study of the prevalence and influence of gifts to radiation oncologists from pharmaceutical companies and medical equipment manufacturers. Int J Radiat Oncol Biol Phys. 2004;59(5):1477–83. [PubMed]
7. Chren MM, Landefeld CS. Physicians’ behavior and their interactions with drug companies. A controlled study of physicians who requested additions to a hospital drug formulary. JAMA.1994;271(9):684–9. [PubMed]
8. Wazana A. Physicians and the pharmaceutical industry: is a gift ever just a gift? JAMA.2000;283(3):373–80. [PubMed]
9. Lexchin J. Interactions between physicians and the pharmaceutical industry: what does the literature say? Cmaj. 1993;149(10):1401–7. [PMC free article] [PubMed]
10. Chren MM, Landefeld CS, Murray TH. Doctors, drug companies, and gifts. JAMA.1989;262(24):3448–51. [PubMed]
11. Katz D, Caplan AL, Merz JF. All gifts large and small: toward an understanding of the ethics of pharmaceutical industry gift-giving. Am J Bioeth. 2003;3(3):39–46. [PubMed]
12. Campbell EG, Gruen RL, Mountford J, Miller LG, Cleary PD, Blumenthal D. A national survey of physician-industry relationships. N Engl J Med. 2007;356(17):1742–50. [PubMed]
13. Becker RACJ, Wilks AR. The New S language: A Programming Environment for Data Analysis and Graphics. Pacific Grove: Wadsworth & Brooks/Cole; 1988.
14. Campbell EG, Weissman JS, Ehringhaus S, et al. Institutional academic industry relationships.JAMA. 2007;298(15):1779–86. [PubMed]
15. Physicians and the pharmaceutical industry American College of Physicians. Ann Intern Med.1990;112(8):624–6. [PubMed]
16. Gifts to physicians from industry. JAMA. 1991;265(4):501. [PubMed]
17. Sanders AB, Keim SM, Sklar D, et al. Emergency physicians and the biomedical industry. Ann Emerg Med. 1992;21(5):556–8. [PubMed]


