| Author | Affiliation |
|---|---|
| Scott H. Stewart, MD | Medical University of South Carolina, Center for Drug and Alcohol Programs, Charleston, SC |
| Ashley Doscher, MD | Medical University of South Carolina, Department of Emergency Medicine, Charleston, SC |
| Sarah Miles | Medical University of South Carolina, Center for Drug and Alcohol Programs, Charleston, SC |
| Keith T. Borg, MD, PhD | Medical University of South Carolina, Department of Emergency Medicine, Charleston, SC |
ABSTRACT
Introduction:
Brief alcohol intervention may improve outcomes for injury patients with hazardous drinking but is less effective with increased severity of alcohol involvement. This study evaluated a brief method for detecting problem drinking in minor trauma patients and differentiating hazardous drinkers from those with more severe alcohol problems.
Methods:
Subjects included 60 minor trauma patients in an academic urban emergency department (ED) who had consumed any amount of alcohol in the prior month. Screening and risk stratification involved the use of a heavy-drinking-day screening item and the Rapid Alcohol Problems Screen (RAPS). We compared the heavy-drinking-day item to past-month alcohol use, as obtained by validated self-reporting methods, and measured the percentage of carbohydrate-deficient transferrin (%CDT) to assess the accuracy of self-reporting. The Alcohol Dependence Scale (ADS) was administered to gauge the severity of alcohol involvement and compared to the RAPS.
Results:
Eighty percent of the subjects endorsed at least one heavy drinking day in the past year, and all patients who exceeded recommended weekly drinking limits endorsed at least one heavy drinking day. Among those with at least one heavy drinking day, 58% had a positive RAPS result. Persons with no heavy drinking days (n=12) had a median ADS of 0.5 (range 0 to 3). RAPS-negative persons with heavy drinking days (n=20) had a median ADS of 2 (range 0 to 8). RAPS-positive persons with heavy drinking days (n=28) had a median ADS of 8 (range 1 to 43).
Conclusion:
A heavy-drinking-day item is useful for detecting hazardous drinking patterns, and the RAPS is useful for differentiating more problematic drinkers who may benefit from referral from those more likely to respond to a brief intervention. This represents a time-sensitive approach for risk-stratifying non-abstinent injury patients prior to ED discharge.
INTRODUCTION
Heavy alcohol consumption is the major preventable cause of injury resulting in an emergency department (ED) visit; however, many alcohol-related injuries occur in people who drink in a hazardous manner without meeting criteria for alcohol dependence.1,2 Because such hazardous drinkers are excellent candidates for a brief intervention (BI) aimed at decreasing future alcohol-related problems, screening and BI has been recommended for ED patients.2,3 This brief counseling process typically involves feedback about alcohol use, an emphasis on responsibility to change drinking, advice on drinking goals, suggestions on how to achieve drinking goals, empathy on the part of the provider, and support of the patient’s self-efficacy.4 While BI is effective for hazardous drinking, persons with more severe alcohol involvement are less likely to respond to BI alone, and may benefit from referral to an addiction treatment facility or self-help group.5 Implementing efficient methods for detecting hazardous drinking and assessing the severity of alcohol problems would thus improve the quality of care for patients with alcohol-related ED visits. This is particularly true for patients with minor trauma who do not require hospitalization. Their relatively short ED stay represents an opportune time to detect and start treatment for problem drinking.6
The Rapid Alcohol Problems Screen (RAPS) is a four-item instrument that has been validated in EDs for the detection of alcohol use disorders (i.e., alcohol abuse and dependence by American Psychiatric Association criteria).7 An extended version, which includes two alcohol use quantity-frequency (QF) items, is referred to as the RAPS-QF.8 The QF items note the presence of heavy drinking days during the past year, and the presence of at least monthly drinking during the past year. This instrument has good sensitivity and specificity for hazardous drinking and for alcohol use disorders, with a positive response to both QF items indicating hazardous use, and any positive RAPS items suggesting an alcohol use disorder. The National Institutes of Health (NIH), in recognition of the value of brief screening in medical settings, has recommended the use of a heavy-drinking-day item alone for initial screening in healthcare settings, with additional assessment for those with one or more heavy drinking days in the past year.9 The same heavy-drinking-day item, using a three-month rather than 12-month time horizon, has been studied in ED settings, and has good sensitivity and specificity for detecting hazardous drinking or alcohol use disorders in combination, but not for differentiating between these conditions.10 We undertook this study to further evaluate the use of the NIH-recommended heavy-drinking-day screening item, followed by the RAPS in minor trauma patients. Our main hypothesis was that patients with positive heavy drinking days but a negative RAPS would have a low severity of alcohol problems, while those with heavy drinking days and a positive RAPS would have a greater severity of alcohol problems. If so, this would further support the combined use of these brief screens as a tool for detecting hazardous drinkers most likely to respond to BI, while also determining who may benefit from referral for additional alcohol assessment as a component of their discharge planning.
METHODS
Recruitment
Subjects included a convenience sample of minor trauma patients age ≥ 18 presenting to an academic urban ED for treatment. Most subjects were recruited during the work week between 8 AM and 6 PM when part-time research staff were available. Minor trauma was defined as an acute injury not resulting in hospitalization. Potential subjects were asked by healthcare personnel if they had consumed any alcohol in the past month and, if so, were they interested in hearing about a research survey for which they would receive $25 for participating, if eligible. Patients who had consumed any alcohol in the past month, who were not currently intoxicated (i.e., blood alcohol content <0.08 mg/dL as estimated by breathalyzer, alco-Sensor FST, Intoximeters, St. Louis, Missouri), who could converse in English, and who expressed interest in participating were approached by research staff for additional study description and to obtain informed consent. In those providing consent, all data were collected prior to ED discharge. The protocol was approved by the university human subjects committee.
Description of the screening instrument
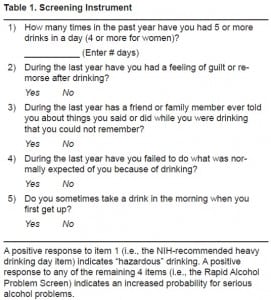
The screening instrument consisted of five items (Table 1). Subjects were provided with the definition of a standard drink before completing the screen. The initial item was the NIH- recommended screen for hazardous drinking, and is similar to the heavy-drinking-day item in the RAPS-QF.8,9 Regardless of their response to the heavy-drinking-day item, all subjects then completed the four RAPS items.7We considered a positive response to the heavy-drinking-day item (i.e., ≥ 1) indicative of hazardous drinking, and any positive response on the RAPS indicative of more severe alcohol problems.
Reference standard for estimating current hazardous drinking
Past 30-day alcohol use was assessed using Alcohol Timeline Followback methodology. This calendar-based method uses memory cues to obtain a daily drinking log from patient recall.11Hazardous drinking is defined by the World Health Organization as drinking that increases risks for adverse health events.12 While there is no specific cutoff for defining hazardous drinking, it is often operationalized as drinking in excess of health-related guidelines. Based on United States dietary guidelines, women who averaged more than one drink per day during any seven-day period in the past month, or consumed more than three drinks on any drinking day, were considered hazardous drinkers.13 For men, the cutoff was averaging more than two drinks per day during any seven-day period or consuming more than four drinks during any drinking day. A “drink” was defined as 14 grams of ethanol, and was calculated from the amount and type of beverage consumed. For example, this is the amount of ethanol in 12 fluid ounces of beer containing 5% ethanol, or 8 fluid ounces of malt liquor containing 8% ethanol.
Reference standard for estimating severity of alcohol involvement
The severity of alcohol problems was estimated with the Alcohol Dependence Scale (ADS).14 This 25-item survey includes questions for estimating elements of an alcohol-dependence diagnosis, including tolerance and withdrawal, impaired control, and compulsivity of drinking behavior. The possible scoring range is 0 to 47, with higher scores correlating with increasing severity of alcohol problems.14,15
Estimating the accuracy of alcohol self-report
Percent carbohydrate-deficient transferrin (%CDT) was used to assess the accuracy of self-reported alcohol consumption, and particularly heavy consumption. Averaging roughly 50 to 60 grams of ethanol or more per day (about four drinks or more as defined for this study) can result in an alteration in the glycoprotein transferrin, which normally has three to six terminal sialic acids on two carbohydrate side chains. Percent CDT consists of the less sialylated isoforms divided by total transferrin, and a level ≥ 2.6% is approximately 65% sensitive and more than 90% specific for heavy drinking within the past 2-3 weeks.16 We measured %CDT in plasma using the Bio-Rad %CDT assay at the Clinical Neurobiology Laboratory of the Medical University of South Carolina.17
Analysis
All analyses were completed with SAS statistical software v. 9.1 (SAS Institute Inc., Cary, NC).
Estimating utility of the screening instrument
We compared the heavy-drinking-day screening results to the alcohol timeline followback, and the RAPS to the ADS. Specifically, we assessed agreement between the heavy-drinking-day item and a hazardous drinking categorization from the timeline followback using Fisher’s exact test. The sensitivity and specificity of this item for hazardous drinking were also estimated. We compared ADS scores between groups with a negative heavy-drinking day and negative RAPS, a positive heavy-drinking day but negative RAPS, and a positive heavy-drinking day and positive RAPS using the Kruskal-Wallis test.
Estimating the validity of alcohol self-report
Using the Wilcoxon rank sum test, we compared the total number of drinks on the 30-day timeline followback, and total number of past-year heavy-drinking days from the screening item, between those with and without a positive %CDT. We also calculated Spearman correlation coefficients between these drinking measures and %CDT.
RESULTS
Research staff approached 166 potential subjects over a four-month period to recruit the 60 (36%) study participants. The major reasons for non-participation included no reported drinking in the past month (n=46), not interested in participating without providing a specific reason (n=39), and blood alcohol concentration above 0.08 mg/dL (n=8). The characteristics of the 60 participants are listed in Table 2. The majority of the patients were less than 35 years of age, with males and females equally represented. Most endorsed at least one heavy-drinking day in the past year, and roughly half of the sample had a positive RAPS result.
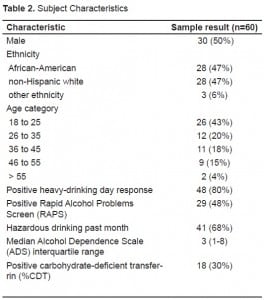
Percent CDT findings supported the accuracy of self-reported alcohol consumption. We correlated % CDT with the total number of drinks in the past month (r=0.38, p=0.003) and total number of heavy-drinking days in the past year (r=0.48, p<0.001). In addition, those with a positive %CDT (n=18, 30%) consumed a median of 164 drinks in the past month, while those with a negative %CDT (n=42) consumed a median of 13 drinks in the past month (Wilcoxon rank sum test p<0.001). Individuals with a positive %CDT reported a median of 209 heavy-drinking days in the past year, while those with a negative %CDT reported a median of six heavy days (Wilcoxon rank sum test p<0.001).
The heavy-drinking-day item was predictive of hazardous drinking (Fisher’s exact test p<0.001), with a sensitivity of 100% and specificity of 85%. The imperfect specificity reflected past-year heavy-drinking days on the screening item in patients without past month hazardous drinking on the timeline followback. The median ADS score in patients with a negative heavy-drinking day item (n=12) was 0.5 (interquartile range 0 to 2); in patients with a positive heavy-drinking day item but negative RAPS (n=20), median ADS was 2 (interquartile range 1 to 3); in patients with a positive heavy-drinking day item and positive RAPS (n=28), median ADS was 8 (interquartile range 5 to 15). These scores were significantly different (p<0.001). Pairwise comparisons were also significantly different (for comparing the heavy-drinking item negative group to the heavy-drinking positive/RAPS negative group p=0.027; p<0.001 for the other pairwise comparisons).
DISCUSSION
This study evaluated the use of the NIH-recommended heavy-drinking-day item and the RAPS for detecting minor injury patients with potentially problematic alcohol use, and subsequently estimated their severity of alcohol problems. Results support the use of the heavy-drinking-day item for detecting hazardous drinking, and the utility of the RAPS in identifying patients who merit additional assessment for alcohol problems.
The utility of the heavy-drinking-day screen has been supported in prior ED-based research, and the RAPS has been clinically validated as a screen for alcohol dependence in ED patients.7,10 In addition, the RAPS-QF includes two items on heavy-drinking days and frequency of drinking, rendering it appropriate for both hazardous drinking and alcohol dependence screening.8 Our results support the use of the RAPS-QF, or RAPS with the heavy-drinking-day item alone, in those endorsing any alcohol use for identifying hazardous drinkers and estimating the severity of their alcohol problems. Since any heavy-drinking day identifies drinking in excess of health-related guidelines,13 patients with a positive heavy-drinking-day item should receive a brief intervention. This may be sufficient treatment given a negative RAPS, although additional study is needed to confirm this hypothesis. Prior research in large probability samples found that a positive RAPS was 87% specific for alcohol dependence in ED patients.7 Results of this study are consistent with this finding, indicating a relatively low level of alcohol problems in RAPS negative patients, and a relatively higher level of problems in those with a positive RAPS. For these patients, referral for additional diagnostic assessment and possible treatment may be indicated, although additional study is also needed in this regard.
LIMITATIONS
Strengths of this study include assessment of a gender-balanced group at high risk for alcohol problems, who require accurate risk stratification during a relatively brief exposure to the healthcare system. The main limitation is the assumption that RAPS negative persons are appropriate for BI alone, while RAPS positive persons require additional assessment and possibly treatment. While this is a reasonable approach to implement in the ED, stronger evidence would require a controlled trial. An additional limitation was our reliance on self-reported consumption, the accuracy of which can be threatened by intentional underreporting or other sources of bias.18However, the validity of self-reported consumption was objectively supported by %CDT results. Finally, the recruitment process may have biased our results. The subjects were not chosen at random or explicitly selected to provide a representative sample, and it is possible that results would differ for the general population of minor trauma patients. Also, some hazardous or even dependent drinkers may have been excluded if they had not consumed any alcohol during the month preceding their ED visit.
CONCLUSION
Brief alcohol interventions are effective in individuals who drink too much at times but are not alcohol dependent, and constitute an important component of care for ED patients. The current study suggests that the use of the NIH-recommended heavy-drinking-day screen, followed by the RAPS in those with heavy-drinking days, is a time-sensitive means for detecting hazardously drinking patients who merit BI, and also risk stratifying these patients to gauge who should be referred for evaluation by an addiction specialist.
Footnotes
Supervising Section Editor: Eric D. Isaacs, MD
Submission history: Submitted December 2, 2008; Revision Received October 6, 2009; Accepted October 7, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Scott H. Stewart, MD, Medical University of South Carolina, PO Box 250861, 67 President Street, Charleston, SC 29425
Email: stewarsh@musc.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Cherpitel CJ, Ye Y. Alcohol-attributable fraction for injury in the U.S. general population: data from the 2005 National Alcohol Survey. J Stud Alcohol Drugs. 2008;69(4):535–8. [PubMed]
2. Gentilello LM, Ebel BE, Wickizer TM, et al. Alcohol interventions for trauma patients treated in emergency departments and hospitals: a cost benefit analysis. Annals of Surgery. 2005;241(4):541–50. [PMC free article] [PubMed]
3. D’Onofrio G, Degutis LC. Preventive care in the emergency department: screening and brief intervention for alcohol problems in the emergency department: a systematic review. Acad Emerg Med. 2002;9(6):627–38. [PubMed]
4. Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction.1993;88(3):315–35. [PubMed]
5. Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations.[see comment] Addiction. 2002;97(3):279–92. [PubMed]
6. Walton MA, Goldstein AL, Chermack ST, et al. Brief alcohol intervention in the emergency department: moderators of effectiveness. J Stud Alcohol Drugs. 2008;69(4):550–60. [PubMed]
7. Cherpitel CJ. A brief screening instrument for problem drinking in the emergency room: the RAPS4. Rapid Alcohol Problems Screen. J Stud Alcohol. 2000;61(3):447–9. [PubMed]
8. Cherpitel CJ, Ye Y, Bond J, et al. Cross-national performance of the RAPS4/RAPS4-QF for tolerance and heavy drinking: data from 13 countries. J Stud Alcohol. 2005;66(3):428–32.[PubMed]
9. National Institute on Alcohol Abuse and Alcoholism Helping patients who drink too much: A clinician’s guide Bethesda, MD: US Department of Health and Human Services 2007. Report No.: NIH Publication No. 07-3769.
10. Williams R, Vinson DC. Validation of a single screening question for problem drinking. Journal of Family Practice. 2001;50(4):307–12. [PubMed]
11. Sobell L, Sobell M. Timeline follow-back: A technique for assessing self-reported ethanol comsumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychological and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72.
12. Babor TF, de la Fuente JR, Saunders J, et al. The Alcohol Use Disorders Identification Test Guidelines for use in primary health care. Geneva, Switzerland: World Health Organization; 1992.
13. Dietary Guidelines for Americans 6th ed. Washington, DC: US Government Printing Office; 2005. 2005.
14. Skinner H, Horn J. Alcohol Dependence Scale User’s Guide. Toronto, ON Canada: Centre For Addiction and Mental Health; 1984.
15. Saxon AJ, Kivlahan DR, Doyle S, et al. Further validation of the alcohol dependence scale as an index of severity. J Stud Alcohol Drugs. 2007;68(1):149–56. [PubMed]
16. Anton RF. Carbohydrate-deficient transferrin for detection and monitoring of sustained heavy drinking. What have we learned? Where do we go from here? Alcohol. 2001;25(3):185–8. [PubMed]
17. Anton RF, Dominick C, Bigelow M, Westby C, Group CDR. Comparison of Bio-Rad %CDT TIA and CDTect as laboratory markers of heavy alcohol use and their relationships with gamma-glutamyltransferase. Clin Chem. 2001;47(10):1769–75. [PubMed]
18. Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction. 2003;98(Suppl 2):1–12. [PubMed]


