| Author | Affiliation |
|---|---|
| Michael Manka, Jr., MD | Erie County Medical Center, Department of Emergency Medicine, Buffalo, NY |
| Ronald Moscati, MD | Erie County Medical Center, Department of Emergency Medicine, Buffalo, NY |
| Krishnan Raghavendran, MD | Erie County Medical Center, Department of Emergency Medicine, Buffalo, NY |
| Aruna Priya, MD | Erie County Medical Center, Department of Emergency Medicine, Buffalo, NY |
ABSTRACT
Introduction:
The focused assessment with sonography for trauma (FAST) exam is a routine diagnostic adjunct in the initial assessment of blunt trauma victims but lacks the ability to reliably predict which patients require laparotomy. Physiologic data play a major role in decision making regarding the need for emergent laparotomy versus further diagnostic testing or observation. The need for laparotomy often influences the decision to transfer the patient to a trauma center. We set out to derive a simple scoring system using both ultrasound findings and immediately available physiologic data that would predict which patients require laparotomy.
Methods:
We conducted a prospective observational study of victims of blunt trauma who presented to a Level 1 Trauma Center. We collected FAST findings, physiologic data, and lab values. A previously-developed ultrasound scoring system was applied to the FAST findings. Patients were followed to determine if they underwent laparotomy. We used logistic regression analysis to determine which variables correlated with laparotomy and developed a new scoring system.
Results:
We enrolled a convenience sample of 1,393 patients. A simple scoring system (range 0–6) was developed that included both FAST findings and vital signs (heart rate and blood pressure). Patients with a score of 0 or 1 had a less than 1% chance of requiring laparotomy.
Conclusion:
The combination of FAST findings with vital signs in our scoring system predicted which victims of blunt trauma did not undergo laparotomy. Applying this to trauma patients who present to non-trauma centers could help prevent unnecessary patient transfers. This derivation set must be validated prior to use in patient care.
INTRODUCTION
The rapid identification of potentially life threatening intra-abdominal injury is critical for patients who sustain blunt abdominal trauma. Early definitive surgical care is crucial for improved survival. Emergency physicians (EPs) practicing in non-trauma center hospitals must often quickly decide whether to transfer a trauma patient to a trauma center or to fully evaluate and manage the patient at their hospital. The suspicion of a significant intra-abdominal injury requiring laparotomy greatly influences the decision to transfer.
Focused assessment with sonography for trauma (FAST) has become a routine part of the initial evaluation of victims of blunt abdominal trauma.1,2 While it has limited ability to detect specific organ injury, its ability to rapidly and non-invasively assess for intra-abdominal hemorrhage makes it a useful diagnostic tool. It has gained widespread use in trauma centers throughout North America and Europe, and as increasing numbers of practicing EPs are trained in ultrasound, its use has expanded beyond urban trauma centers to community and rural hospitals.3
Multiple studies have attempted to derive a decision rule or scoring scale to predict the need for emergent laparotomy based on FAST findings and clinical presentation.4–11 While this may be useful for patients who are evaluated in a trauma center, for patients in rural or community hospitals the question is not whether to take the patient to the operating room (OR), but rather whether or not to immediately transfer the patient to a trauma center. A tool that could reliably predict which patients had a very low likelihood of requiring an emergent laparotomy would be helpful.
Most previously developed decision rules use FAST findings with or without hypotension to predict the need for laparotomy.7–9,11 We were interested in combining a larger number of physiologic findings and laboratory values with a previously developed FAST scoring scale to predict more accurately which patients would not require a laparotomy. Our study objective was to identify the combination of ultrasound findings, physiologic criteria, and laboratory values that reliably excluded patients from requiring an urgent laparotomy.
METHODS
This study was a prospective observational study of victims of blunt trauma who presented to our American College of Surgeons Level I Trauma Center with an annual emergency department (ED) census of 52,000. The study was approved by our local institutional review committee. A waiver of informed consent was granted since patient care was not altered.
Eligible study subjects included victims of blunt trauma who presented directly or were transferred to our trauma center for evaluation and required trauma team activation. The study population was a convenience sample, as enrollment occurred from 7am to 11pm when ED data collectors were present. Prisoners and patients with known ascites or with penetrating trauma were excluded. We made no effort to enroll patients who presented outside these hours, nor to determine if the nighttime population differed from those in our study.
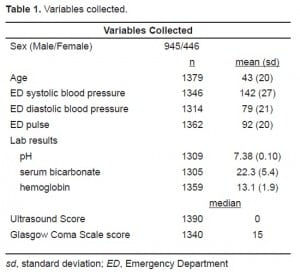
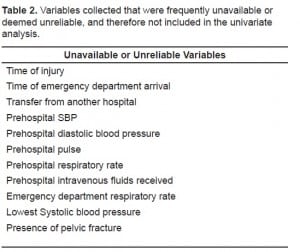
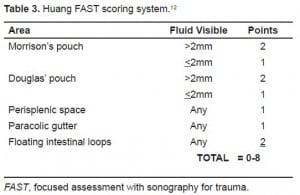
Patients had routine trauma evaluations performed by both EPs and the trauma team (comprised of surgical residents and a trauma surgery attending). Either post-graduate year 3 emergency medicine (EM) residents or EM attendings trained in bedside ultrasound performed FAST exams. Locations of free intraperitoneal fluid on FAST exams were reported to the data collector by the treating physician. Physiologic data were also collected. (Tables 1 and and 2) Patients had further evaluation and treatment at the discretion of the ED and trauma services. Study investigators scored FAST exam findings later, using a previously developed scoring system (Table 3).12
Subjects’ medical records were subsequently reviewed to determine which patients had a therapeutic laparotomy within the first three days of hospital admission. Therapeutic laparotomy was defined by any of the following findings: grade 4 or 5 hepatic injury or splenic injury, greater than one liter of intraperitoneal blood, hollow viscus injury requiring repair, great vessel injury, left diaphragmatic rupture, pancreatic injury, or bladder rupture. Patients who had surgery other than laparotomy, such as craniotomy, thoracic, or orthopedic procedures were not considered positives.
The data were initially examined for reliability. Prehospital and ED respiratory rates were not included in the final data analysis due to a clear lack of variability that led us to believe they were not accurately measured. We excluded time of injury and prehospital intravenous fluid received in the analysis due to frequent missing data. For the remaining physiologic data and ultrasound scores (USs), we used logistic regression to determine which variables correlated with laparotomy. Using SAS (SAS 8.1, SAS Institute, Cary, NC), univariate models were fit with “laparotomy done” as the outcome to identify variables significantly (p-value < 0.05) associated with therapeutic laparotomy.
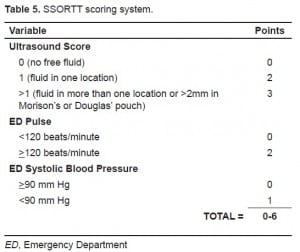
Once the associated variables were identified, multiple logistic models with stepwise selection procedures were tested using progressive cutoff points (heart rate every 5 beats/minute and blood pressure every 10 mm Hg). We chose the cutoff values based on these models, as well as physiologic parameters that represent class III hemorrhagic shock [pulse ≥ 120 beats/minute and systolic blood pressure (SBP) < 90 mm Hg].2 From these models we developed a simplified score that used the combined variables associated with which subjects would not have urgent laparotomy. We called this the sonographic score for operating room triage in trauma (SSORTT) score.
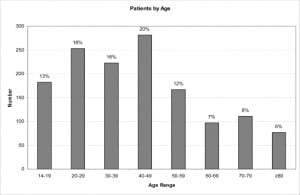
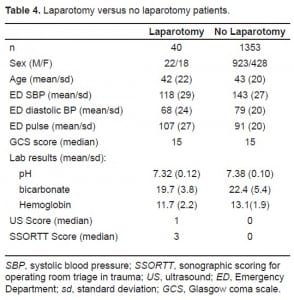
RESULTS
We enrolled 1,393 patients, of whom 40 (2.9%) had urgent laparotomy. Subjects were 68% male. Age range was 14 to 94 years, with a median of 40 and an inter-quartile range of 25 to 55 (Figure 1). Of the 40 patients who had laparotomy, all were reported to have a therapeutic surgical intervention. Mean results for the reliably collected variables are demonstrated in Table 4. Time of injury, prehospital vital signs and fluid resuscitation volumes were not consistently available or accurately recorded (for example, pre-hospital respiratory rates showed little variability and were most often recorded as 20 breaths/minute). We analyzed the remaining variables for association with the need for laparotomy. Ultrasound score, initial ED SBP, and ED pulse were the only three variables associated with laparotomy.
A model using the variables ultrasound score, initial ED SBP, and ED pulse as continuous variables gave an area under receiver-operator characteristic curve (AUC) of 0.852. These variables were then modeled using stepwise cutoffs to develop a mathematical scoring system. We condensed the US, which initially had a range of 0–8, into three categories (US score = 0, 1 or >1). This equated to either no free fluid (US score = 0), fluid in one location (US score = 1), or fluid in more than one location or more than 2mm of fluid in either Morison’s or Douglas’s pouch (US score >1). We condensed ED pulse and SBP into two categories (pulse<120 or ≥120 and SBP<90 or ≥90). The model with laparotomy necessary as the outcome and the variables categorized in this manner gave an AUC of 0.823. To develop a simple, useable scoring system we then weighted the variables based on their strength of correlation in the regression model and perceived clinical importance.
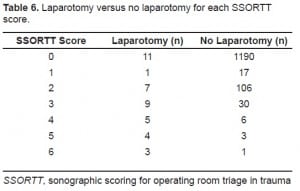
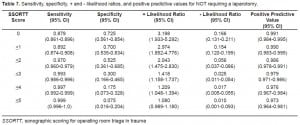
Table 5 illustrates our scoring system. Based on this system, a patient could achieve a score from 0 to 6. The breakdown of patients (laparotomy versus no laparotomy) for each SSORTT score is demonstrated in Table 6. Table 7 presents the sensitivity, specificity, positive and negative likelihood ratios, and positive predictive values for not requiring a laparotomy at different SSORTT score cutoffs. Patients with a score of less than or equal to 1 had a positive likelihood ratio of 2.974 (95% CI 1.852–4.776) and a positive predictive value of 0.990 (95% CI 0.983–0.995) for not requiring a laparotomy.
DISCUSSION
The use of ultrasound in the initial evaluation of blunt trauma victims is routine within trauma centers in North America and Europe, and the American College of Surgeons now includes FAST as an adjunct to the primary survey in the Advanced Trauma Life Support course.2 We set out to develop a simple scoring system that could help the treating physician decide how to proceed with patient management.
We developed a simple scoring system that, if validated prospectively, would predict which victims of blunt trauma have a very low probability of requiring laparotomy. Our score combines FAST exam findings with immediately available vital signs of pulse and SBP. The ability to rapidly and non-invasively determine that a trauma patient does not need urgent laparotomy may help the treating physician decide whether to transfer the patient to a trauma center.
A number of studies have used various types of FAST scoring systems to try to determine the need for a therapeutic laparotomy. A hemoperitoneum score developed by McKenney et al., combined the depth of the largest fluid collection with the number of sites of free intraperitoneal fluid. Based on their scoring system, 87% of patients with an US score ≥ 3 and all patients with hypotension (defined as SBP ≤90 mm Hg) and an US score ≥ 3 required a therapeutic laparotomy. Thirty-eight percent of their patients with scores of <3 and hypotension still required laparotomy compared with only 4% of patients who were normotensive with a score <3.9 However, their study was limited in that they only included patients with sonograms positive for free fluid, so predictions regarding patients who had negative sonograms could not be made. Huang, et al.12 developed “A Simple Scoring System” for the evaluation of hemoperitoneum with ultrasonography based on free intra-abdominal fluid seen at specific sites. In their study, 96% of patients with an US score ≥ 3 required therapeutic laparotomy. While both of these studies showed that FAST findings can be used to help predict the overall probability that a given patient will require laparotomy, neither scoring system has been widely incorporated into practice. This is due in large part to the difficulty of applying broad percentages to individual patients, to the poor negative predictive values, and partly due to the complexity of their scoring systems. With the widespread availability of CT and the fact that traumatic intra-abdominal injuries are increasingly managed non-operatively, even patients with positive FAST exams rarely go directly to the OR, unless they are hemodynamically unstable.
In a recent study by Moylan et al., it has been demonstrated that there is a strong association between a positive ED FAST exam and therapeutic laparotomy in normotensive blunt trauma patients.13 In their study, 37% of normotensive patients (defined as SBP > 100mm Hg) with a positive FAST exam required a therapeutic laparotomy versus 0.5% with a negative FAST exam. Their study excluded patients who were hypotensive during the initial ED evaluation. Our study builds upon this association by including hypotensive patients and by attempting to develop a useable scoring system to accurately predict which patients will likely not require laparotomy.
Recognizing that it is difficult to make clinical decisions based on a single test (FAST exam), we analyzed multiple clinical, laboratory, and US findings to determine how best to predict which patients would ultimately require therapeutic laparotomy. Interestingly, none of the laboratory values had a significant correlation with the need for laparotomy. This is most likely due to other traumatic injuries frequently causing significant lab abnormalities, such as hypoxemia, acidosis, coagulopathy, and anemia. Overall, in our study, a positive FAST exam was the single best predictor of laparotomy, but adding SBP and pulse strengthened the correlation.
The scoring system that we developed is simple and uses variables that are immediately and dependably available, as well as highly correlated with the need for surgery. It also allows the physician to easily calculate a score while at the patient’s bedside with minimal information and without the aid of complex formulas. This score, if validated prospectively, can then be applied to reliably predict which patients would likely not require a laparotomy.
Blunt trauma patients evaluated at community and rural hospital EDs are often transferred to trauma centers early in the course of their evaluation. This is often done to hasten emergent laparotomy if it becomes necessary, as well as place decisions with those more experienced in trauma. However, this also consumes resources to transfer and manage patients at trauma centers who are increasingly treated non-operatively. It can also displace patients away from home and family support.
Although often times disregarded, there is both a significant cost (financial and personnel) as well as risk associated with an ambulance or helicopter transfer. As the demand on the emergency medical services (EMS) increases, unnecessary utilization of EMS places patients who truly need those services at risk. Also, patients who are transferred emergently via ambulance place both the crew and patient at increased risk of motor vehicle collision.14,15
Frequently lab and imaging are repeated at the receiving trauma center. In addition to financial costs, there is the risk of additional radiation exposure to the patient. Experts generally agree that CT scans are associated with an increase in the lifetime risk of cancer and that trauma patients generally have a significant radiation exposure as the result of diagnostic imaging.16–18 Avoiding unnecessary transfers may limit the amount of repeat diagnostic imaging at the receiving facility, thereby decreasing radiation risk.
While victims of significant blunt trauma should be thoroughly evaluated by physicians experienced in trauma management, there are significant potential benefits of limiting unnecessary transfers to a Level I Trauma Center. SSORTT could better inform the decision to transfer for patients with a low likelihood of needing laparotomy.
LIMITATIONS
Some of our desired data were either unavailable or not reliably collected, especially by prehospital providers. For example, the amount of IV fluids received was often not documented and had the potential for lowering heart rate and increasing blood pressure. We also questioned the accuracy of some of our data, particularly the respiratory rates, which lacked the expected physiologic variability.
Relating to our data analysis, we used univariate models to identify variables associated with therapeutic laparotomy. Variables that may help discriminate between laparotomy versus no laparotomy in a multivariate model may not have been identified.
Our data set was derived only from patients who were transported to a single Level I Trauma Center. The decision to operate on a patient is at the discretion of the trauma surgeon. It is possible our trauma surgeons are more or less likely to operate than surgeons at other centers, although our overall laparotomy rate of 2.9% is similar to rates noted in other studies.13,19 Also, our patients are more likely to be severely injured than those seen in a non-trauma setting. Additionally, two of the variables (blood pressure and heart rate) are important factors that are considered as part of the decision-making paradigm by the trauma surgeon. As with any derived clinical decision rule, our score needs prospective validation in different settings and in non-trauma centers.
Finally, while all of our trauma FAST exams were performed by EPs trained to perform emergency ultrasound, we did not determine inter-rater reliability. Since ultrasound findings are highly operator dependent, this is another potential source of error.
CONCLUSION
FAST exams are part of the initial evaluation of victims of blunt trauma. Combining FAST findings with heart rate and SBP determines a simple score associated with a low likelihood of having therapeutic laparotomy. If prospectively validated, this score might prevent unnecessary or emergent transfers of blunt trauma patients to trauma centers. In an era of shrinking healthcare resources, this score could be of benefit.
Footnotes
Supervising Section Editor: J. Christian Fox, MD, RDMS
Submission history: Submitted March 9, 2009; Revision Received October 26, 2009; Accepted October 26, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Michael A. Manka, Jr., MD, Department of Emergency Medicine, Erie County Medical Center, 462 Grider St., Buffalo, NY 14215
Email : mmanka@ecmc.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. Supported by the Center for Transportation Injury Research (CenTIR) Grannt #C99-006F. National Highway Transportation and Safety Agency.
REFERENCES
1. ACEP Clinical Policies Committee and the Clinical Policies Subcommittee on Acute Blunt Abdominal Trauma Clinical policy: Critical issues in the evaluation of adult patients presenting to the emergency department with acute blunt abdominal trauma. Ann Emerg Med. 2004;43(2):278–90.[PubMed]
2. American College of Surgeons Advanced Trauma Life Support for Doctors: Student Manual. 8th ed. American College of Surgeons; Chicago, IL: 2008.
3. Boulanger BR, Kearney PA, Brenneman FD, et al. Utilization of FAST (Focused Assessment with Sonography for Trauma) in 1999: results of a survey of North American trauma centers. Am Surg.2000;66(11):1049–55. [PubMed]
4. Bode PJ, Edwards MJ, Kruit MC, et al. Sonography in a clinical algorithm for early evaluation of 1671 patients with blunt abdominal trauma. AJR Am J Roentgenol. 1999;172(4):905–11. [PubMed]
5. Bode PJ, Niezen RA, van Vugt AB, et al. Abdominal ultrasound as a reliable indicator for conclusive laparotomy in blunt abdominal trauma. J Trauma. 1993;34(1):27–31. [PubMed]
6. Boulanger BR, McLellan BA, Brenneman FD, et al. Prospective evidence of the superiority of a sonography-based algorithm in the assessment of blunt abdominal injury. J Trauma.1999;47(4):632–7. [PubMed]
7. Farahmand N, Sirlin CB, Brown MA, et al. Hypotensive patients with blunt abdominal trauma: performance of screening US. Radiology. 2005;235(2):436–43. [PubMed]
8. Lee BC, Ormsby EL, McGahan JP, et al. The utility of sonography for the triage of blunt abdominal trauma patients to exploratory laparotomy. AJR Am J Roentgenol. 2007;188(2):415–21. [PubMed]
9. McKenney KL, McKenney MG, Cohn SM, et al. Hemoperitoneum score helps determine need for therapeutic laparotomy J Trauma 2001. 504650–4.4discussion 654–6. [PubMed]
10. Rose JS, Richards JR, Battistella F, et al. The fast is positive, now what? Derivation of a clinical decision rule to determine the need for therapeutic laparotomy in adults with blunt torso trauma and a positive trauma ultrasound. J Emerg Med. 2005;29(1):15–21. [PubMed]
11. Wherrett LJ, Boulanger BR, McLellan BA, et al. Hypotension after blunt abdominal trauma: the role of emergent abdominal sonography in surgical triage. J Trauma. 1996;41(5):815–20. [PubMed]
12. Huang MS, Liu M, Wu JK, et al. Ultrasonography for the evaluation of hemoperitoneum during resuscitation: a simple scoring system. J Trauma. 1994;36(2):173–7. [PubMed]
13. Moylan M, Newgard C, Ma O, et al. Association between a positive ED FAST examination and therapeutic laparotomy in normotensive blunt trauma patients. J of Emer Med. 2007;33(3):265–71.
14. Becker LR, Zaloshnja E, Levick N, et al. Relative risk of injury and death in ambulances and other emergency vehicles. Accid Anal Prev. 2003;35(6):941–8. [PubMed]
15. Custalow CB, Gravitz CS. Emergency medical vehicle collisions and potential for preventive intervention. Prehosp Emerg Care. 2004;8(2):175–84. [PubMed]
16. Brenner DJ, Hall EJ. Computed tomography–an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–84. [PubMed]
17. Ott M, McAlister J, VanderKolk WE, et al. Radiation exposure in trauma patients J Trauma 2006.613607–9.9discussion 609–10. [PubMed]
18. Tien HC, Tremblay LN, Rizoli SB, et al. Radiation exposure from diagnostic imaging in severely injured trauma patients. J Trauma. 2007;62(1):151–6. [PubMed]
19. Hadjizacharia P, Plurad D, Green D, et al. Outcomes of Blunt Assault at a Level 1 Trauma Center. J Trauma. 2009;66(4):1202–6. [PubMed]


