| Author | Affiliation |
|---|---|
| Brian Dawson, MD | Brody School of Medicine at East Carolina University, Greenville, NC |
| Kelly Carter, MD | Brody School of Medicine at East Carolina University, Greenville, NC |
| Kori Brewer, PhD | Brody School of Medicine at East Carolina University, Greenville, NC |
| Luan Lawson, MD | Brody School of Medicine at East Carolina University, Greenville, NC |
ABSTRACT
Introduction:
The healthcare chart is becoming ever more complex, serving clinicians, patients, third party payers, regulators, and even medicolegal parties. The purpose of this study was to identify our emergency medicine (EM) resident and attending physicians’ current knowledge and attitudes about billing and documentation practices. We hypothesized that resident and attending physicians would identify billing and documentation as an area in which residents need further education.
Methods:
We gave a 15-question Likert survey to resident and attending physicians regarding charting practices, knowledge of billing and documentation, and opinions regarding need for further education.
Results:
We achieved a 100% response rate, with 47% (16/34) of resident physicians disagreeing or strongly disagreeing that they have adequate training in billing and documentation, while 91% (31/34) of residents and 95% (21/22) of attending physicians identified this skill as important to a resident’s future practice. Eighty-two percent (28/34) of resident physicians and 100% of attending physicians recommended further education for residents
Conclusion:
Residents in this academic EM department identified a need for further education in billing and documentation practices.
INTRODUCTION
“If it isn’t in the chart then it wasn’t done,” is often heard from attending physicians, department heads, administrators, and coders alike. Documentation has been important as a means of communicating to future providers what was done for the patient; over time the chart has evolved to serve additional purposes. Many academic physicians lament this progressive growth in charting as required by the Centers for Medicare and Medicaid Services [CMS, or as it was previously known, the Health Care Financing Administration (HCFA)] and believe that it detrimentally impacts both patient care and resident teaching.1–3 The medical chart is now used to justify reimbursement from third-party payers, and is an important medicolegal document. Each of the chart functions has separate requirements and considerations that the physician must master to be successful in today’s healthcare environment. The Accreditation Council for Graduate Medical Education (ACGME) has recognized the importance of teaching residents these skills by including a requirement in its six core competencies for “systems-based practice” and for “professionalism.”4–6
In 1992, the Medicare fee schedule became “resource based,” and the new Current Procedure Terminology (CPT) codes developed by the American Medical Association were implemented by the HCFA. The Evaluation and Management (E/M) codes under this system are site specific, indicating where [clinic, nursing home, emergency department (ED)] the service was performed. These codes are further divided into as many as five different levels, reflecting the amount of work required by the physician. E/M levels are designed to reflect separate elements of every visit, most importantly the patient’s history, physician’s examination, and medical decision-making. Under this system there are graduated requirements for each level of service and each of the three elements. A problem arises when the physician evaluates a patient for a problem that is eligible to be billed at a certain level but cannot be billed due to inadequate chart documentation. Although the physician may have performed the work they will be reimbursed at the lower level, a practice referred to as “downcoding.”
Current didactics in billing and documentation at this academic ED include a lecture during intern orientation, a focus on documentation in monthly morbidity and mortality conference, chart reviews and a “billing overview” meeting during third-year administration month. We created a survey to document our resident and attending physicians’ attitudes and knowledge regarding billing and documentation practices under our current educational system. Our hypothesis was that our physicians would identify lack of adequate knowledge in this area.
METHODS
All protocols were reviewed and approved by the University Medical Center Institutional Review Board.
Study design
We gave a 15-question survey using a Likert scale to 34 EM residents (study authors were excluded) from a single accredited three-year residency, with 12 first-year, 13 second-year, and 11 third- year residents. The ED has an annual census of about 70,000 and is in a rural tertiary care hospital. The purpose of the resident survey was to evaluate residents’ knowledge of and attitudes towards billing and documentation practices. We gave a similar 22-question survey using a Likert scale to all 22 EM attending physicians from the same EM residency. The attending physician survey asked similar questions regarding knowledge of billing and documentation practices, as well as their opinions about the residents’ knowledge.
Data Analysis
Responses were recorded in a database and response percentages were calculated and reported.
RESULTS
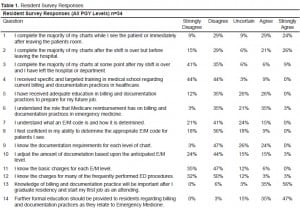
For the purposes of analysis an affirmative response was considered to be agree or strongly agree, while a negative response was disagree or strongly disagree. While significant findings are discussed below, complete survey questions and results by percentage are provided in Tables 1 (for residents) and Table 2 (for attendings).

We obtained completed surveys from both 100% (34/34) of EM residents (excluding two study authors) and 100% (22/22) of EM attending physicians.
Regarding current residency training, only 26% of our residents and 29% of our attendings reported adequate education in billing and documentation in the residency program to prepare the residents for their future jobs. Both residents (91%) and attendings (95%) agreed that current or future jobs will require this knowledge.
Understanding of evaluation and management (E/M) codes was poor among residents, with 15% reporting that they understood what an E/M code is and how it is determined. While 81% of attending physicians reported that they themselves understood the E/M code and how it is determined, only 14% thought that residents understood this aspect of billing.
Regarding future education on billing and documentation, 82% of our residents and 100% of our attendings agreed that further education on this topic should be provided. Furthermore, 100% of our attendings reported that resident documentation needs improvement.
DISCUSSION
In our EM residency a recent change in our documentation system underscored that resident education in billing and documentation requirements may be inadequately addressed. Previously, EM residents and their programs have identified documentation criteria for various E/M codes and the concept and use of RVUs as an area in which they lack adequate knowledge and skill, even after graduation.7 More recently, an abstract presented at the 2006 American College of Emergency Physicians Research Forum reported more frequent downcoding from one billable level of chart to a lower level among EM residents, compared to midlevel providers and attending physicians.8 Not only do EM residents identify this as an area needing improvement, but a recent Schumacher Group survey of ED administrators reported they felt EM physicians were not well prepared for the current pay-for-performance setting.9
This appears not to be an isolated issue for EM, as several other residency groups including internal medicine, surgery, and obstetrics and gynecology have all identified billing and documentation by residents as an area that needs improvement.10
Further training in documentation would be helpful to EM residents on more than one level. In today’s EM job environment, there seems to be a move towards more pay-for-performance jobs. This is likely to continue if reimbursement rates from third parties stay stagnant or decline. Preparing EM residents for this job climate requires proficiency in billing and documentation.
Given the growing trend toward reporting of “core measures,” quality initiatives, and hospital ratings, it is likely administrators will continue to place emphasis on the medical chart to ensure compliance. We should be preparing EM residents to meet these aspects of their future careers.
In 1999 a survey given to all EM residents as part of the annual American Board of Emergency Medicine In-training examination reported that residents across the nation identified billing and documentation practices as an area in which they needed more training.7 Our survey confirms that our current residents continue to identify this as an area in which they believe they lack adequate education. A focused educational offering on billing and documentation offered during residency, rather than at the beginning and end, might help meet this perceived deficit. Future areas of study could include developing and testing the outcome of an educational program, using the metric of RVUs generated before and after the program to document change.
LIMITATIONS
Our study was limited to one EM program with a small sample size. We did not measure actual resident or attending performance or detailed knowledge of billing and coding documentation requirements.
CONCLUSION
EM residents and attending physicians in this academic department continue to identify billing, coding and documentation requirements as an area in which resident physicians need further training.
Footnotes
We would like to thank Kim Carter and the billing department for their assistance.
Supervising Section Editor: Eric D. Isaacs, MD
Submission history: Submitted January 6, 2009; Revision Received October 14, 2009; Accepted October 25, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Brian Dawson, MD, Department of Emergency Medicine, Brody School of Medicine at East Carolina University, Greenville, NC
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Brett AS. New guidelines for coding physicians’ services – a step backward. N Engl J Med.1998;339:1705–8. [PubMed]
2. Kassierer JP, Angell M. Evaluation and management guidelines – fatally flawed. N Engl J Med.1998;339:1697–8. [PubMed]
3. McLean SA. The Impact of Changes in HCFA Documentation Requirements on Academic Emergency Medicine: Results of a Physician Survey. Acad Emerg Med. 2001;8(9):880–885.[PubMed]
4. Stahmer SA, Ellison SR, Jubanyik KK, et al. Integrating the core competencies: proceedings from the 2005 Academic Assembly consortium. Acad Emerg Med. 2007;14(1):80–94. [PubMed]
5. Dyne PL, Strauss RW, Rinnert S. Systems-based practice: the sixth core competency. Acad Emerg Med. 2002;9:1270–7. [PubMed]
6. ACGME Outcome Projects website Available at: www.acgme.org/outcome/ Accessed November 2007.
7. Howell J, Chisholm C, Clark A, Spillane L. Emergency medicine resident documentation: results of the 1999 american board of emergency medicine in-training examination survey. Acad Emerg Med.2000 Oct;7(10):1135–8. [PubMed]
8. Ardolic B, Weizberg M, Cambria B, Dazio F, Hahn B, Farooqui Y, Maniago E. Documentation and Coding Skills: Is There Adequate training in Emergency Medicine Residency? Ann Emerg Med. 2006 Oct;48(4):108(S).
9. Hospital ED Survey Reveals Growing Concerns ACEP News, Emergency Medicine Connect Career and CME Guide, October2007. Page 12, 26. (Results of Schumaker Group Survey 2006 – survey of hospital emergency department administrators.
10. Fakhry SM, Robinson L, Hendershot K, Reines HD. Surgical residents’ knowledge of documentation and coding for professional services: an opportunity for a focused educational offering. Am J Surg. 2007 Aug;194(2):263–7. [PubMed]


