| Author | Affiliation |
|---|---|
| Isaac Yoshii, MD | University of California, Irvine School of Medicine, Irvine, CA |
| Rockan Sayegh, MA | University of California, Irvine School of Medicine, Irvine, CA |
| Shahram Lotfipour, MD, MPH | University of California, Irvine School of Medicine, Irvine, CA |
| Federico E. Vaca, MD, MPH | Yale University School of Medicine, Department of Emergency Medicine, New Haven, CT |
ABSTRACT
Injury is the leading cause of death and disability among the U.S. population aged 1 to 44 years. In 2006 more than 179,000 fatalities were attributed to injury. Despite increasing awareness of the global epidemic of injury and violence, a considerable gap remains between advances in injury-prevention research and prevention knowledge that is taught to medical students. This article discusses the growing need for U.S medical schools to train future physicians in the fundamentals of injury prevention and control. Teaching medical students to implement injury prevention in their future practice should help reduce injury morbidity and mortality. Deliberate efforts should be made to integrate injury-prevention education into existing curriculum. Key resources are available to do this. Emergency physicians can be essential advocates in establishing injury prevention training because of their clinical expertise in treating injury. Increasing the number of physicians with injury- and violence- prevention knowledge and skills is ultimately an important strategy to reduce the national and global burden of injury.
INTRODUCTION
Paramedic: “University Med, this is Rescue 1.”
Radio Nurse: “Rescue 1, this is University Med. Your contact time is 23:45.”
Paramedic: “University Med. our patient contact time was 23:35. We have a critical male trauma. He is a 19-year-old male, 90 kg, driver of single vehicle rollover crash, with altered level of consciousness, heavy ethanol odor, high rate of speed with severe vehicle damage and large amount of intrusion. There was no treatment prior to our arrival; airway open, breathing labored; circulation rapid; skin cool, pale and moist; no seatbelt but airbag deployed; left pupil blown, right responds but sluggish; 15 liters non-rebreather; spinal stabilization – back board and c-collar. At patient contact time, Glasgow Coma Score was 2-3-4. At 23:40 pulse of 130, reps are 18 shallow, blood pressure 90/60, sinus tach. University Med, you are our closest trauma center, ETA is 5 minutes.”
Radio Nurse: “10-4, Rescue 1. I will activate our trauma team.”
Paramedic: “10-4, University Med. We are going 902-H to your facility”
In emergency departments (ED) across the nation, it is far too common to receive the paramedic base station call that heralds the needless loss of limb or life due to preventable injury.
Despite increasing recognition of the global epidemic of injury, medical schools have not collectively included injury prevention as an important component of their curriculum. Association of American Medical Colleges (AAMC) data from its 2004 Curriculum Management and Information Tool show that just a over one-quarter of allopathic medical schools in the U.S. require coursework in topics associated with injury.1 Former Surgeon General Richard Carmona wrote in an opinion article that ours is a “treatment-focused society, when the real social and economic benefits arise from being prevention-focused.”2 We believe it is the goal of many national and international organizations [Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), Association of American Medical Colleges (AAMC)]) that the number of physicians with expertise in injury prevention will increase and ultimately improve the injury-prevention infrastructure.
In the treatment-focused ED, emergency physicians (EP) do their best to control the consequences of devastating injuries. However, a study conducted by Stewart et al.3 showed that nearly 90% of trauma deaths occur in patients who sustain injuries that are physiologically and anatomically non-survivable. Clearly, new trauma treatment protocols do not have the potential to reduce mortality as prevention strategies can. Reduction of injury-related mortality can be quickly realized with the systematic implementation of broad prevention efforts aimed at intentional and unintentional injuries.4 However, the paucity of physician training in basic injury prevention and control makes injury-related mortality reduction unlikely. This article highlights the need and ability of medical schools in the U.S. to train physicians in the fundamentals of injury prevention and control.
DISCUSSION
Global Impact of Injury
Worldwide, injury accounts for five million deaths annually, 9% of the world total. Many million more suffer non-fatal injuries.5 In the U.S. injury is the leading cause of death and disability from age 1 to 44 years, killing more than 179,000 people annually.6 In 2007 nearly 30 million suffered non-fatal injuries in the U.S.7 The CDC estimates this number is rising and annually costs approximately 10% of U.S. medical expenditures.8,9
Teaching Medical Students Injury Prevention
The accreditation standards for medical education established by the Liaison Committee on Medical Education mandate inclusion of prevention and preventive medicine, as well as behavioral and socioeconomic subjects.10 A recent AAMC report outlined the need for future physicians to be adequately trained in injury prevention and control.1 To improve medical student education regarding injury, the AAMC collaborated with the CDC to form the Injury Prevention and Control Education for Medical Students Panel, which was further supported by the CDC’s National Center for Injury Prevention and Control. Through coordinated efforts, they addressed what medical students should learn about injury prevention and treatment and what kind of educational experiences allow students to achieve these learning objectives.1
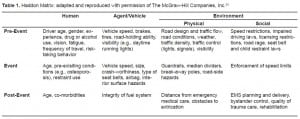
Using general skills from the AAMC Medical School Objectives Project report, the panel identified three categories specific to injury prevention and treatment: 1) Understanding the epidemiology of injury; 2) developing the ability to deliver appropriate clinical care for injuries; and 3) understanding injuries in the context of health systems. A useful tool to contextually depict the first objective is the Haddon Matrix (Table 1). Originally developed by Dr. William Haddon Jr. in 1970, this matrix examines factors involved in an injurious event and categorizes it into an epidemiological triad of agent-host-environment and the event sequence.11,12 Using the Haddon Matrix to establish the factors involved in the presenting case in this article, we can establish a framework for the development of injury-control interventions. Delivering appropriate clinical care for injuries (second objective) involves multiple criteria, including the ability to provide anticipatory guidance based on behavioral risk factors, to recognize injuries related to mass casualty events, and to remain nonjudgmental and avoid stereotyping. Finally, understanding injuries in the context of health systems (third objective) involves understanding the medical-legal aspects of injury and the various systems of acute care. It also encompasses understanding the importance of the quality of patient-level surveillance data and the role of environmental and policy interventions to reduce injury risk, morbidity and mortality.
Educational Strategies and Resources for Medical Student Teaching
Injury-related learning objectives should be integrated in pre-clinical and clinical years. A combination of didactics and experiential learning exercises should also be used.1 Two notable training tools are Teach Violence and Injury Prevention (TEACH-VIP) by the World Health Organization, and Core Competencies: Essentials for Injury and Violence Prevention by the Society for the Advancement of Violence and Injury Research (SAVIR) and the State and Territorial Injury Prevention Directors Association (STIPDA).13,14
TEACH-VIP is designed for classroom instruction and includes PowerPoint slide presentations and supporting lecture notes that address a broad range of topics. The curriculum consists of 21 core lessons and 39 advanced one-hour lessons. Core lesson topics include injury prevention principles, measurement of injuries, injury surveillance, community methodology survey methods, ethical issues in the injury field, types of injuries, and policy development/advocacy. Advanced lessons help to deepen understanding of all aspects of the field of emergency medicine. Almost 80% of surveyed medical and public health students who received injury prevention education via TEACH-VIP felt it was effective.15
In 2000 SAVIR and STIPDA formed the National Training Initiative for Injury and Violence Prevention and began a process to define essential knowledge and skills required by injury-prevention professionals. This guideline lists nine core competencies, some of which are the ability to describe and explain injury as a major social and health problem, and design and implement injury prevention activities (Table 2). These core competencies guide future training and curriculum development. Incorporating this in the curriculum would facilitate teaching students the skills that best serve injury and violence prevention in the clinical setting.

The AAMC report discussed earlier provides a few examples of medical schools that have succeeded in creating educational opportunities in injury prevention. Brown Medical School collaborated with the Injury Prevention Center at Rhode Island Hospital to provide fourth-year medical students rotating through the emergency medicine (EM) elective focused instruction on injury prevention. Instructors deliver an introductory lecture about the history and science of injury prevention, injury as a disease process, the analysis of injury events, and methods of prevention. Students later attend a case conference where they present injured patients they cared for in the ED. They must discuss host risk factors, mechanisms of injury, energy transfer, injury-prevention strategies, and patient education. Finally, students are observed with patients to assess their ability to conduct injury-prevention counseling. The medical students at Brown also receive concentrated exposure during required community health clerkships. One to three students per clerkship are assigned to the Injury Prevention Center and participate in community outreach, including disseminating information, advocating for prevention, and coalition building to promote lasting community change.
Applicability of Injury Prevention to Medical Students
Within the curriculum of the third-year clerkships, medical students are exposed continuously to the end result of injuries. During the fourth year, this effect is seen especially during the EM and trauma surgery rotations. The proper use of such clinical encounters to educate patients must be taught to future physicians, and this is best done during medical school. Students may emphasize injury prevention during their preclinical education while taking a history and performing physical examination. Clinical vignettes could include anticipatory guidance questions and focused injury inquiry. This includes screening for intimate partner violence, alcohol and drug problems, and asking older adults and their families about fitness to drive vs. driving cessation.16 Such training will allow future physicians to play an important role in the safety of patients both in the office and the hospital.
Role of Emergency Medicine
Over the last four decades, injury prevention and control and EM have had parallel evolution. EM provides a unique perspective on injury prevention and control, and EPs are well-suited to help reduce the national burden of injury. Injury prevention and control is now recognized as integral to EM residency training, although it still needs more emphasis in the core curriculum. In 2006, EDs across the U.S. received 119 million visits. Of those, 42.4 million (36%) were the consequence of injury.17 ED prevention efforts can be effective in preventing injury and reducing risky behavior.18–23 EPs should therefore lead efforts to implement injury prevention control in medical school curricula.
CONCLUSION
Future and current physicians have a vital role in prevention of injury. They must be involved in developing strategies, practices and behaviors that promote safety and health in patients as well at the community. We need to incorporate these principles into the medical school curriculum, so that all medical students have a basic understanding of injury prevention and control, which parallels their knowledge of other major health conditions. Physicians, especially EPs, should lead the charge.
Footnotes
Supervising Section Editor: Gene Hern Jr., MD
Submission history: Submitted April 29, 2009; Revision Received August 2, 2009; Accepted August 22, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Federico Vaca MD, MPH, Professor of Emergency Medicine, Department of Emergency Medicine, Yale University School of Medicine, 464 Congress Avenue, Suite 260, New Haven, CT 06519
Email: Federico.vaca@yale.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. AAMC Training future physicians about injury. Washington DC: Association of American Medical Colleges; Dec, 2005.
2. Carmona R. Support candidates who favor preventive health-care approach. Arizona Daily Star; Aug 22, 2007.
3. Stewart RM, Myers JG, Dent DL, et al. Seven hundred and fifty-three consecutive deaths in a level 1 trauma center: the argument for injury prevention. J Trauma. 2003;54:66–71. [PubMed]
4. Gentilello LM. Alcohol Interventions in Trauma Centers: The Opportunity and the Challenge. J Trauma. 2005;59:S18–S20. [PubMed]
5. World Health Organization 10 facts on injuries and violence. Mar 12, 2008. Available at:http://www.who.int/features/factfiles/injuries/en/. Accessed August 24, 2009.
6. Heron MP, Hoyert DL, Murphy SL, et al. Deaths: Final data for 2006. Natl Vital Stat Rep.2009;57(14):1–134. [PubMed]
7. CDC Injury Mortality Report. Web-based Injury Statistics Query and reporting System. National Center for Injury Prevention and Control, Center for Disease Control and Prevention. Available at:http://www.cdc.gov/ncipc/wisqars. Accessed August 10, 2009.
8. CDC Medical expenditures attributable to injuries–United States, 2000. MMWR Morb Mortal Wkly Rep. 2004;53(1):1–4.
9. CDC Years of potential life lost before age 65. Web-based Injury Statistics Query and Reporting System. National Center for Injury Prevention and Control, Center for Disease Control and Prevention. Available at: http://www.cdc.gov/ncipc/wisqars. Accessed October 1, 2007.
10. LCME Accreditation standards. Liaison Committee on Medical Education. Available athttp://www.lcme.org/standard.htm. Accessed July 15, 2008.
11. Runyan CW. Using the Haddon matrix: introducing the third dimension. Inj Prev. 1998;4(4):302–7. [PMC free article] [PubMed]
12. Runyan CW. Introduction: back to the future-revisiting Haddon’s conceptualization of injury epidemiology and prevention. Epidemiol Rev. 2003;25:60–4. [PubMed]
13. TEACH-VIP Developed by World Health Organization (WHO). Available at:http://www.who.int/violence_injury_prevention/capacitybuilding/teach_vip/en/index.htmlAccessed December 15, 2007.
14. Core Competencies for Injury and Violence Prevention Developed by the National Training Initiative for Injury and Violence Prevention (NTI) – a joint project of the State and Territorial Injury Prevention Directors Association (STIPDA) and the Society for the Advancement of Violence and Injury Research (SAVIR) Available at: http://www.injuryed.org/competencies.htm. Accessed December 15, 2007.
15. Meddings DR, Knox LM, Maddaleno M, et al. World Health Organization’s TEACH-VIP contributing to capacity building for youth violence prevention. Am J Prev Med. 2005;29(5 Suppl 2):259–65. [PubMed]
16. Phelan MB, Fallmirski ME, Simpson DE, Czinner ML, Hargarten SW. Competency-based strategies for injury control and prevention curriculums in undergraduate medical education. Inj Prev.2007;13:6–9. [PMC free article] [PubMed]
17. Pitts SR, Niska RW, Xu J, Burt CW. Hyattsville, MD: National Center for Health Statistics; 2008. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary National health statistics reports; no 7.
18. Claudius IA, Nager AL. The utility of safety counseling in a pediatric emergency department.Pediatrics. 2005;115:423–27.
19. Crawford MJ, Patton R, Touquet R. Screening and referral for brief intervention of alcohol-misusing patients in an emergency department: a pragmatic randomized controlled trail. Lancet.2004;364:1334–39. [PubMed]
20. Posner JC, Hawkins LA, Garcia-Espana F, et al. A randomized controlled trial of a home safety intervention based in an emergency department setting. Pediatrics. 2004;113:1603–08. [PubMed]
21. Bishai D, Qureshi A, Cantu N, et al. Contracting with children and helmet distribution in the emergency department to improve bicycle helmet use. Acad Emerg Med. 2003;10:1371–78.[PubMed]
22. Kruesi MJ, Grossman J, Pennington JM, et al. Suicide and violence prevention: parent education in the emergency department. J Am Acad Child Adolesc Psychiatry. 1999;38(3):250–5. [PubMed]
23. Mackenzie EJ, Fowler CJ. Epidemiology of Injury. In: Moore E, Feliciano D, Mattox K, editors.Trauma. 5th ed. New York, NY: McGraw-Hill Companies, Inc; 2003.


