| Author | Affiliation |
|---|---|
| Christopher R Carpenter, MD, MSc | Washington University School of Medicine, Division of Emergency Medicine, St Louis, Missouri |
| Richard T Griffey, MD, MPH | Washington University School of Medicine, Division of Emergency Medicine, St Louis, Missouri |
| Susan Stark, PhD, OTR/L | Washington University School of Medicine, Division of Occupational Therapy, St Louis, Missouri |
| Craig M Coopersmith, MD | Emory University School of Medicine, Division of Critical Care, Atlanta, Georgia |
| Brian F Gage, MD, MSc | Washington University School of Medicine, Division of General Medical Sciences, St Louis, Missouri |
ABSTRACT
Introduction:
The objective of this study was to evaluate emergency medicine physician and nurse acceptance of nonnurse, nonphysician screening for geriatric syndromes.
Methods:
This was a single-center emergency department (ED) survey of physicians and nurses after an 8-month project. Geriatric technicians were paid medical student research assistants evaluating consenting ED patients older than 65 years for cognitive dysfunction, fall risk, or functional decline. The primary objective of this anonymous survey was to evaluate ED nurse and physician perceptions about the geriatric screener feasibility and barriers to implementation. In addition, as a secondary objective, respondents reported ongoing geriatric screening efforts independent of the research screeners.
Results:
The survey was completed by 72% of physicians and 33% of nurses. Most nurses and physicians identified geriatric technicians as beneficial to patients without impeding ED throughput. Fewer than 25% of physicians routinely screen for any geriatric syndromes. Nurses evaluated for fall risk significantly more often than physicians, but no other significant differences were noted in ongoing screening efforts.
Conclusion:
Dedicated geriatric technicians are perceived by nurses and physicians as beneficial to patients with the potential to improve patient safety and clinical outcomes. Most nurses and physicians are not currently screening for any geriatric syndromes.
INTRODUCTION
In 1900, just 5% of the population was older than 65 years; today it is 17% and projected to reach 25% by 2051.1 Emergency departments (ED) will be caring for increasing volumes of geriatric patients for decades.2 Older adults often face social isolation and economic stressors just as their health is challenged with increasing frailty and comorbid illness.3 Geriatric patient pathology presents particular challenges as signs and symptoms are frequently atypical and layered with multiple confounding socioeconomic and chronic disease influences. These barriers result in prolonged ED length of stay and increased resource utilization.4,5 Recently, improving older adult care has been the focus for the development of emergency medicine (EM) quality indicators and revised graduate medical education curricula.6–8 Responding to this demographic imperative with structural and procedural innovations will be a challenge to EM, which will require heightened efforts at evidence-based surveillance and intervention.9
The historic charge of EM has been to expeditiously recognize life-threatening conditions in order to rapidly intervene and appropriately “disposition” patients.10 Within these objectives, emergency physicians have long recognized the unique challenges geriatric adults represent.11–13 Despite this awareness, busy physicians operating in crowded EDs too often fail to recognize occult dementia, delirium, or high-risk fallers.14–18 For example, up to 40% of adults older than 65 years in the ED will demonstrate an abnormal mental status, including 10% with delirium, but nurses and clinicians will fail to recognize up to 80% of these patients.14,16,17,19–21 Similarly, 27% of older adults will have suffered a standing-level fall each year; however, when these patients present to the ED, they rarely receive guideline-directed care to prevent subsequent injurious falls.18,22 Whether these missed opportunities result from insufficient training, lack of well-accepted quality indicators, personnel indifference, or crowding is not clear. What is clear is that missed opportunities to intervene can adversely impact mortality and ED recidivism.16,23–25 In addition, patients expect EM to participate in preventive medicine when possible, and the Society for Academic Emergency Medicine Preventive Medicine Task Force has identified several geriatric-specific efforts to undertake.26,27
In the past, older adult emergency care models have been used to identify occult cognitive dysfunction and poor short-term prognosis.28,29 These surveillance programs relied upon nurse or physician participation to evaluate patients beyond their presenting complaint. Since then, brief screening tools have been derived and partially validated in the ED for cognitive dysfunction, falls, and prognostic decline.20,21,30–32 Geriatric syndromes have been defined as “multifactorial health conditions that occur when the accumulated effects of impairments in multiple systems render [an older] person vulnerable to situational changes.”33 The mechanistic concept of geriatric syndromes is elusive to study, since it does not often result from deterioration of 1 organ system, but instead results from a constellation of age-related changes.3,34 Although physicians and nurses are best equipped to administer and appropriately interpret geriatric syndrome screening tools, staffing and patient volumes often preclude lengthy one-on-one encounters. The perception that ED screening tools are complicated and time-consuming can further impede their use by busy nurses and physicians.
Inserting cheaper, readily available personnel with responsibilities limited to older adult screening using simple, validated tools may be 1 widely applicable solution to effective surveillance for modifiable age-related disease processes. The objective of the current study was to evaluate EM nurse and physician acceptance of a “geriatric technician” for screening older patients. A secondary objective was to assess ongoing physician and nurse screening for geriatric syndromes.
METHODS
Study Design
We performed a cross-sectional survey of attending physicians and nurses at a single level I trauma center ED. At the time of the survey, the 4 geriatric technicians had been screening consenting adults older than 65 years for 40 hours per week for 8 months (July 2008–February 2009) for cognitive dysfunction, fall risk, and short-term functional decline. The geriatric technicians were premedical or medical students with an interest in older adult healthcare who were paid an hourly wage through research funds. The criterion standard for cognitive dysfunction was the Mini-Mental Status Examination,35 while functional decline was determined by baseline and 3-month Older American Resources and Services activities of daily living.36,37 Initial fall-risk stratification was based upon a recent systematic review, while fall incidence was determined by 3-month telephone follow-up.30This survey and the geriatric technician screening objectives were approved by the institutional review board.
Study Setting and Population
Our ED evaluates 84,000 adult patients annually of which 18% are older than 65 years. In February 2009, our ED consisted of 103 full-time nurses and 29 faculty physicians, all of whom were EM board certified or board eligible. Nurses and faculty received no in-service training before the initiation of geriatric technician screening, but they did receive an e-mail notification that individuals would be approaching them to evaluate their older adult patients for potential inclusion in ongoing research projects. The ED staff was otherwise unaware of the geriatric technician objectives or findings. Geriatric technician screening worked around clinical care, endeavoring never to impede patient care or ED flow.
Survey Content and Administration
Attending physicians were provided an 8-item survey (Appendix 1; online only) pertaining to the ED management of geriatric patients at a faculty meeting. No resident physicians were surveyed. During day, evening, and overnight shifts, nurses completed the same survey except for question 8, which was changed to reflect nursing experience. Both nurse and physician responses were anonymously placed into a closed collection box with no identifiers.
Measures
The primary outcome was the proportion of respondents who found the geriatric technician role acceptable and feasible. The secondary outcome was the proportion of respondents reporting independent screening for selected geriatric syndromes.
Data Analysis
All data were entered into a Microsoft Excel database (Excel 2007; Microsoft Corporation, Redmond, Washington). The data were analyzed to determine proportions amenable to geriatric technician screening and the proportion with ongoing self-reported geriatric screening efforts. Likert responses were collapsed into 2 categories: favorable/neutral and unfavorable by combining the first 3 response choices into 1 category labeled “favorable” versus the latter 2 choices labeled “unfavorable.” Percentages with 95% confidence intervals were then computed with SPSS (version 16.0; SPSS Inc, Chicago, Illinois). Nurse and physician responses were compared with χ2 tests with significance defined as a 2-sided P < 0.05.
RESULTS
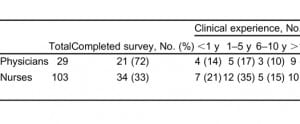
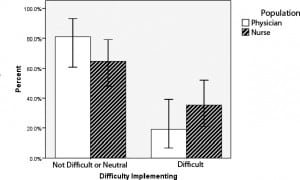
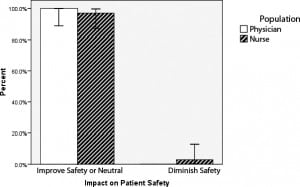
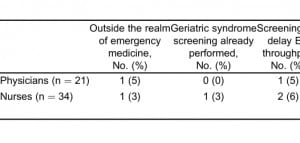
The survey was completed by 21 physicians and 34 nurses for an overall response rate of 42%, including 72% of physicians and 33% of nurses (Table 1). Most physicians (71%; 95% confidence interval [CI], 52%–91%) and nurses (85%; 95% CI, 73%–97%) identified geriatric technician screening as an overall benefit to older ED patients. In analyzing perceived delays in ED throughput, physician (0%; 95% CI, 0%–4%) and nurse (18%; 95% CI, 5%–30%) responses differed nonsignificantly on whether geriatric technician screening prolonged the ED length of stay. Most respondents believed that geriatric technician screening would have a positive effect on patient care (Table 2) and patient safety (Table 3), but one third were neutral regarding the level of difficulty in implementing this clinical strategy (Table 4).
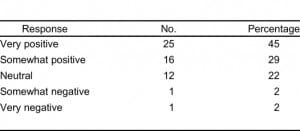
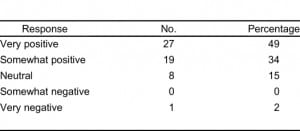
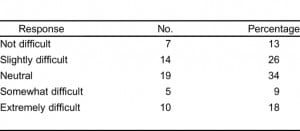
Few physicians or nurses identified barriers to geriatric technician screening for geriatric syndromes in the ED (Figures 1–3, which include 95% CI). While most physicians and nurses believed that a geriatric technician would enhance patient safety and improve patient care, 35% of nurses and 19% of physicians believe that such a role would be difficult to implement in most EDs. In free-text responses, the respondents who believed that this model would be more difficult to implement elsewhere listed personnel shortages and budget shortfalls as their rationale for these implementation problems. Fewer than 5% of physicians or nurses felt that geriatric technician screening would adversely impact older adult patient safety or overall clinical care (Table 5). With the exception of nursing screening for fall risk, neither nurses nor physicians reported significant ongoing geriatric syndrome screening efforts using validated instruments (Table 6). Nurses reported significantly more falls screening than physicians, but no other significant differences were noted between physicians and nurses.
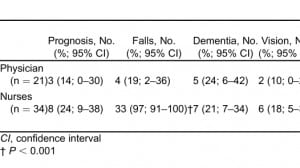
DISCUSSION
This study demonstrates that most nurses and physicians do not believe that screening older adults for prevalent geriatric syndromes is outside the realm of EM. However, our results suggest that fewer than 25% of EM physicians and 30% of nurses are currently screening for prevalent geriatric syndromes. After exposure to a dedicated individual without ancillary responsibilities to screen older adults for prevalent geriatric syndromes, most EM physicians and nurses recognize a potential overall benefit to patient safety and clinical outcomes. On the other hand, a substantial proportion of the respondents were equivocal about the degree of difficulty entailed in establishing a geriatric technician screening protocol.
The current screening model limited evaluation to 3 geriatric syndromes: cognitive dysfunction, falls, and functional decline. Older adults offer many other opportunities for screening including pneumococcal and influenza vaccinations,26,38–42 depression,43–46 sensory deficits,34,47,48 home safety,49,50 polypharmacy,51,52 frailty,53 elder neglect or abuse,54 or malnutrition.55,56 In an era of daily ED crowding with prolonged length of stays, time is less of an obstacle than personnel resources.
Although not evaluated, the geriatric technician model may improve patient satisfaction through enhanced attention to time-consuming issues and effective time management during lengthy ED evaluations.57 No interventions were evaluated in the current screening model, which was an acceptability assessment. However, the geriatric technician offers valuable risk-stratification information upon which clinicians can modify decision making and initiate protocols to activate nursing, social work, and case-manager resources. For example, 4 EM geriatric prognostic instruments incorporate self-reported memory problems or objectively detected cognitive dysfunction in assessing for the risk of short-term functional decline, ED recidivism, or death.37,58–60Expedited and reliable recognition of cognitive dysfunction via focused geriatric technician case finding might facilitate incorporation of these prognostic instruments into clinical decision making. Currently, EM physicians and nurses fail to diagnose most patients with dementia or delirium.14,16,17,19,61 Furthermore, when the diagnosis of cognitive dysfunction is not established in the ED, inpatient and outpatient providers often fail to make the diagnosis as well.61,62
Another role that the geriatric technician could serve is as a 2-way communication conduit between the ED and older adult resources within the institution or community. In addition, the geriatric technician could perform a next-day phone follow-up to ascertain symptom improvement, medication compliance, follow-up scheduling, and ED satisfaction. Insufficient follow-up feedback to clinicians is a major barrier to improving patient safety.63 Access to systems failures via this follow-up feedback loop could enhance clinicians’ awareness and empower them to avoid similar issues in the future.
Common ED presentations resulting from geriatric syndromes include incontinence, pressure ulcers, falls, altered mental status, and functional decline. How might geriatric technician screening be incorporated into routine ED operations for older adults? One model would be to have geriatric technicians screen all older adults for cognitive dysfunction and fall risk by using validated instruments. For example, the geriatric technicians could have a non–critically ill patient complete the Short Blessed Test64,65 and a few fall-related questions22 (Appendix 2; online only) to identify subsets of patients at higher risk for occult dementia, delirium, or short-term injurious falls. The geriatric technician could then communicate findings to ED providers and family while helping to facilitate appropriate referrals to outpatient resources for definitive diagnostic testing and appropriate interventions. Since falls have recently been labeled as “never events” for which Medicare will not reimburse, reliable fall-risk stratification could provide patient-oriented benefit while simultaneously proving cost-effective.66 Therefore, efficient and timely recognition of high-risk subsets may ultimately avoid some of these “never events” and ultimately prove cost-effective for hospitals while simultaneously improving ED care of older adults. Dementia is one of the strongest predictors of falls in older adults, but independent of fall risk, identifying potential cognitive impairment would empower clinicians to reinforce discharge planning with caregivers and facilitate late-stage life planning while patients still possess relatively intact decision-making capabilities.67,68
LIMITATIONS
This study has several limitations. First, this was a convenience sampling of nurses and physicians from a single institution. Results may differ at other sites, based upon existing older adult screening protocols or staffing levels. Additionally, nurse survey response rates were low and the sampling may not adequately reflect the perspectives of the entire ED nursing staff. Future geriatric technician screening efforts will most likely benefit from more active involvement of nursing research and leadership teams. Second, the geriatric technician role was not fully explained to healthcare providers in the trial period. A comprehensive introduction of the geriatric technician to nurse and physician staff would probably enhance awareness, recruitment, and incorporation into existing protocols. Third, the survey used was not validated and the reported results may not reflect actual practice. For example, cognitive dysfunction is often underrecognized by EM physicians, suggesting that dementia and/or delirium screening efforts are not routinely conducted.14,15 In addition, question 2 offered several general reasons why geriatric technician screening might be impractical, with the option to free text additional barriers not foreseen by the investigators, but additional obstacles undoubtedly exist. Furthermore, validated screening instruments for dementia,69 falls,22frailty,53 and functional decline 31,70 have yet to be developed for EM such that the self-reported use of validated instruments in our cohort most likely reflects a deficiency in geriatric medical knowledge.11,13 Fourth, responses were collected as a 5-item Likert scale and then collapsed into 2 post-hoc categories to simplify the data interpretation. Most respondents favored geriatric technician screening for the impact upon patient care and safety, while a substantial proportion were equivocal about the level of difficulty in implementing this case-finding protocol. Collapsing 5 category responses into 2 categories may therefore be an oversimplification of the results. Finally, screening results were not actually used in patient management decisions; therefore, the potential impact of positive or negative test results on clinical decision making or patient outcomes cannot be determined. We wanted to evaluate the acceptability of the geriatric technician for screening and felt that blinding clinicians to their ongoing activities would provide the most accurate measure of the geriatric technicians’ unique contribution to ED information attainment. Nonetheless, without an interventional arm, we cannot evaluate whether such screening changes clinician behavior or patient-oriented outcomes.
CONCLUSION
Most EM nurses and physicians believe that an individual dedicated to screening older adults for prevalent geriatric syndromes would benefit overall clinical care without negatively impacting patient flow. Many nurses and physicians report screening for dementia, falls, functional status, polypharmacy, and functional decline despite lacking validated tools. Future research will need to demonstrate clinically important impact on outcomes or safety without significantly diminishing operational flow before widespread geriatric syndrome screening can be broadly recommended.
Footnotes
Supervising Section Editor: Teresita M. Hogan, MD
Submission history: Submitted May 5, 2010; Revision received September 9, 2010; Accepted January 15, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.1.1962
Address for Correspondence: Christopher R. Carpenter, MD, MSc
Washington University School of Medicine, Campus Box 8072, 660 S Euclid Ave, St Louis, MO 63110
E-mail: carpenterc@wusm.wustl.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. Dr Carpenter was supported by the Washington University Goldfarb Patient Safety Award. None of the other co-authors have any conflicts of interest to declare.
REFERENCES
1. [No authors listed]. Who cares for the elderly. The Lancet. 2008;;371:959.
2. Roberts DC, McKay MP, Shaffer A. Increasing rates of emergency department visits for elderly patients in the United States, 1993 to 2003. Ann Emerg Med. 2008;;51:769–774. [PubMed]
3. Inouye SK, Studenski S, Tinetti ME, et al. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;;55:780–791. [PMC free article][PubMed]
4. Baum SA, Rubenstein LZ. Old people in the emergency room: age-related differences in emergency department use and care. J Am Geriatr Soc. 1987;;35:398–404. [PubMed]
5. Singal BM, Hedges JR, Rousseau EW, et al. Geriatric patient emergency visits, part I: comparison of visits by geriatric and younger patients. Ann Emerg Med. 1992;;21:802–807. [PubMed]
6. Terrell KM, Hustey FM, Hwang U, et al. Quality indicators for geriatric emergency care. Acad Emerg Med. 2009;;16:441–449. [PubMed]
7. Hogan TM, Losman ED, Carpenter CR, et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med. 2010;;17:316–324.[PMC free article] [PubMed]
8. Carpenter CR, Heard K, Wilber ST, et al. Research priorities for high-quality geriatric emergency care: medication management, screening and prevention, and functional assessment. Acad Emerg Med. 2011;;18:644–654. [PMC free article] [PubMed]
9. Hwang U, Morrison RS. The geriatric emergency department. J Am Geriatr Soc. 2007;;55:1873–1876. [PubMed]
10. Sanders AB, Witzke DB, Jones JS, et al. Principles of care and application of the geriatric emergency care model. In: Sanders AB, editor. Emergency Care of the Elder Person. St Louis, MO: Beverly-Cracom Publications;; 1996. pp. 59–93.
11. McNamara RM, Rousseau E, Sanders AB. Geriatric emergency medicine: a survey of practicing emergency physicians. Ann Emerg Med. 1992;;21:796–801. [PubMed]
12. Schumacher JG, Deimling GT, Meldon SW, et al. Older adults in the Emergency Department: predicting physicians’ burden levels. J Emerg Med. 2006;;30:455–460. [PubMed]
13. Carpenter CR, Lewis LM, Caterino JM, et al. Emergency physician geriatric education: an update of the 1992 geriatric task force survey: has anything changed? Ann Emerg Med. 2008;;52:S156.
14. Hustey FM, Meldon SW. The prevalence and documentation of impaired mental status in elderly emergency department patients. Ann Emerg Med. 2002;;39:248–253. [PubMed]
15. Hustey FM, Meldon SW, Smith MD, et al. The effect of mental status screening on the care of elderly emergency department patients. Ann Emerg Med. 2003;;41:678–684. [PubMed]
16. Lewis LM, Miller DK, Morley JE, et al. Unrecognized delirium in ED geriatric patients. Am J Emerg Med. 1995;;13:142–145. [PubMed]
17. Elie M, Rousseau F, Cole M, et al. Prevalence and detection of delirium in elderly emergency department patients. CMAJ. 2000;;163:977–981. [PMC free article] [PubMed]
18. Donaldson MG, Khan KM, Davis JC, et al. Emergency department fall-related presentations do not trigger fall risk assessment: a gap in care of high-risk outpatient fallers. Arch Gerontol Geriatr.2005;;41:311–317. [PubMed]
19. Naughton BJ, Moran MB, Kadah H, et al. Delirium and other cognitive impairment in older adults in an emergency department. Ann Emerg Med. 1995;;25:751–755. [PubMed]
20. Wilber ST, Lofgren SD, Mager TG, et al. An evaluation of two screening tools for cognitive impairment in older emergency department patients. Acad Emerg Med. 2005;;12:612–616.[PubMed]
21. Wilber ST, Carpenter CR, Hustey FM. The Six-Item Screener to detect cognitive impairment in older emergency department patients. Acad Emerg Med. 2008;;15:613–616. [PubMed]
22. Carpenter CR. Evidence-based emergency medicine/rational clinical examination abstract. Will my patient fall? Ann Emerg Med. 2009;;53:398–400. [PubMed]
23. Ballabio C, Bergamaschini L, Mauri S, et al. A comprehensive evaluation of elderly people discharged from an Emergency Department. Intern Emerg Med. 2008;;3:245–249. [PubMed]
24. Laniece I, Couturier P, Drame M, et al. Incidence and main factors associated with early unplanned hospital readmission among French medical inpatients aged 75 and over admitted through emergency units. Age Ageing. 2008;;37:416–422. [PubMed]
25. McCusker J, Cole M, Abrahamowicz M, et al. Delirium predicts 12-month mortality. Arch Intern Med. 2002;;162:457–463. [PubMed]
26. Rodriguez RM, Kreider WJ, Baraff LJ. Need and desire for preventive care measures in emergency department patients. Ann Emerg Med. 1995;;26:615–620. [PubMed]
27. Babcock-Irvin C, Wyer PC, Gerson LW. Preventive care in the emergency department, Part II: Clinical preventive services—an emergency medicine evidence-based review. Acad Emerg Med.2000;;7:1042–1054. [PubMed]
28. Gerson LW, Counsell SR, Fontanarosa PB, et al. Case finding for cognitive impairment in elderly emergency department patients. Ann Emerg Med. 1994;;23:813–817. [PubMed]
29. Mion LC, Palmer RM, Meldon SW, et al. Case finding and referral model for emergency department elders: a randomized clinical trial. Ann Emerg Med. 2003;;41:57–68. [PubMed]
30. Ganz DA, Bao Y, Shekelle PG, et al. Will my patient fall? JAMA. 2007;;297:77–86. [PubMed]
31. Dendukuri N, McCusker J, Belzile E. The identification of seniors at risk screening tool: further evidence of concurrent and predictive validity. J Am Geriatr Soc. 2004;;52:290–296. [PubMed]
32. Hustey FM, Mion LC, Connor JT, et al. A brief risk stratification tool to predict functional decline in older adults discharged from emergency departments. J Am Geriatr Soc. 2007;;55:1269–1274.[PubMed]
33. Tinetti ME, Inouye SK, Gill TM, et al. Shared risk factors for falls, incontinence, and functional dependence: unifying the approach to geriatric syndromes. JAMA. 1995;;273:1348–1353. [PubMed]
34. Cigolle CT, Langa KM, Kabeto MU, et al. Geriatric conditions and disability: the health and retirement study. Ann Intern Med. 2007;;147:156–164. [PubMed]
35. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;;12:189–198. [PubMed]
36. Fillenbaum G. The OARS Methodology—A Manual. 2nd ed. Durham, NC: Center for Study of Aging, Duke University;; 1978.
37. McCusker J, Bellavance F, Cardin S, et al. Detection of older people at increased risk of adverse health outcomes after an emergency visit: the ISAR screening tool. J Am Geriatr Soc.1999;;47:1229–1237. [PubMed]
38. Manthey DE, Stopyra J, Askew K. Referral of emergency department patients for pneumococcal vaccination. Acad Emerg Med. 2004;;11:271–275. [PubMed]
39. Polis MA, Davey VJ, Collins ED, et al. The emergency department as part of a successful strategy for increasing adult immunization. Ann Emerg Med. 1988;;17:1016–1018. [PubMed]
40. Polis MA, Smith JP, Sainer D, et al. Prospects for an emergency department-based adult immunization program. Arch Intern Med. 1987;;147:1999–2001. [PubMed]
41. Slobodkin D, Kitlas JL, Zielske PG. A test of the feasibility of pneumococcal vaccination in the emergency department. Acad Emerg Med. 1999;;6:724–727. [PubMed]
42. Wrenn K, Zeldin M, Influenza Miller O. and pneumococcal vaccination in the emergency department: is it feasible? J Gen Intern Med. 1994;;9:425–429. [PubMed]
43. Fabacher DA, Raccio-Robak N, McErlean MA, et al. Validation of a brief screening tool to detect depression in elderly ED patients. Am J Emerg Med. 2002;;20:99–102. [PubMed]
44. Hustey FM. The use of a brief depression screen in older emergency department patients. Acad Emerg Med. 2005;;12:905–908. [PubMed]
45. Meldon SW, Emerman CL, Schubert DS. Recognition of depression in geriatric ED patients by emergency physicians. Ann Emerg Med. 1997;;30:442–447. [PubMed]
46. Meldon SW, Emerman CL, Schubert DS, et al. Depression in geriatric ED patients: prevalence and recognition. Ann Emerg Med. 1997;;30:141–145. [PubMed]
47. Wallhagen MI, Pettengill E, Whiteside M. Sensory impairment in older adults, part 1: hearing loss.Am J Nurs. 2006;;106:40–48. [PubMed]
48. Whiteside M, Wallhagen MI, Pettengill E. Sensory impairment in older adults, part 2: vision loss.Am J Nurs. 2006;;106:52–61. [PubMed]
49. Carter SE, Campbell EM, Sanson-Fisher RW, et al. Environmental hazards in the homes of older people. Age Ageing. 1997;;26:195–202. [PubMed]
50. Lord SR, Menz HB, Sherrington C. Home environment risk factors for falls in older people and the efficacy of home modifications. Age Ageing. 2006;;35:ii55–ii59. [PubMed]
51. Caterino MM, Emond JA, Camargo CA Jr. Inappropriate medication administration to the acutely ill elderly: a nationwide emergency department study, 1992–2000. J Am Geriatr Soc.2004;;52:1847–1855. [PubMed]
52. Hohl CM, Dankoff J, Colacone A, et al. Polypharmacy, adverse drug-related events, and potential adverse drug interactions in elderly patients presenting to an emergency department. Ann Emerg Med. 2001;;38:666–671. [PubMed]
53. Hastings SN, Purser JL, Johnson KS, et al. Frailty predicts some but not all adverse outcomes in older adults discharged from the emergency department. J Am Geriatr Soc. 2008;;56:1651–1657.[PMC free article] [PubMed]
54. Anetzberger GJ. Elder abuse identification and referral: the importance of screening tools and referral protocols. J Elder Abuse Neglect. 2001;;13:3–22.
55. Lang PO, Heitz D, Hedelin G, et al. Early markers of prolonged hospital stays in older people: a prospective, multicenter study of 908 inpatients in French acute hospitals. J Am Geriatr Soc.2006;;54:1031–1039. [PubMed]
56. Drame M, Jovenin N, Novella JL, et al. Predicting early mortality among elderly patients hospitalised in medical wards via emergency department: the SAFES cohort study. J Nutr Health Aging. 2008;;12:599–604. [PubMed]
57. Nerney MP, Chin MH, Jin L, et al. Factors associated with older patients’ satisfaction with care in an inner-city emergency department. Ann Emerg Med. 2001;;32:140–145. [PubMed]
58. Meldon SW, Mion LC, Palmer RM, et al. A brief risk-stratification tool to predict repeat emergency department visits and hospitalizations in older patients discharged from the emergency department. Acad Emerg Med. 2003;;10:224–232. [PubMed]
59. Runciman P, Currie CT, Nicol M, et al. Discharge of elderly people from an accident and emergency department: evaluation of health visitor follow-up. J Adv Nurs. 1996;;24:711–718.[PubMed]
60. Boyd M, Koziol-McLain J, Yates K, et al. Emergency department case-finding for high-risk older adults: the Brief Risk Identification for Geriatric Health Tool (BRIGHT) Acad Emerg Med.2008;;15:598–606. [PubMed]
61. Heidt JW, Carpenter CR. Occult cognitive impairment in admitted older emergency department patients is not identified by admitting services. Ann Emerg Med. 2009;;54:S81.
62. Callahan CM, Hendrie HC, Tierney MC. Documentation and evaluation of cognitive impairment in elderly primary care patients. Ann Intern Med. 1995;;122:422–429. [PubMed]
63. Cosby KS, Croskerry P. The nature of EM. In: Croskerry P, Cosby KS, Schenkel SM, editors.Patient Safety in Emergency Medicine. Philadelphia, PA: Lippincott Williams & Wilkins; 2009. pp. 5–7. et al, eds.
64. Katzman R, Brown T, Fuld P. Validation of a short orientation-memory-concentration test of cognitive impairment. Am J Psychiatry. 1983;;140:734–739. [PubMed]
65. Carpenter CR, Bassett ER, Fischer GM, et al. Four sensitive screening tools to detect cognitive dysfunction in geriatric emergency department patients: brief Alzheimer’s Screen, Short Blessed Test, Ottawa3DY, and the caregiver administered AD8. Acad Emerg Med. 2011;18:374–384.[PMC free article] [PubMed]
66. Pronovost PJ, Goeschel CA, Wachter RM. The wisdom and justice of not paying for “preventable complications” JAMA. 2008;;299:2197–2199. [PubMed]
67. Engel KG, Heisler M, Smith DM, et al. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand? Ann Emerg Med. 2009;;53:454–461. [PubMed]
68. Carpenter BD, Xiong C, Porensky EK, et al. Reaction to a dementia diagnosis in individuals with Alzheimer’s disease and mild cognitive impairment. J Am Geriatr Soc. 2008;;56:405–512. [PubMed]
69. Carpenter CR. Does this patient have dementia? Ann Emerg Med. 2008;;52:554–556. [PubMed]
70. Lee DC, Pancu DM, Rudolph GS, et al. Age-associated time delays in the treatment of acute myocardial infarction with primary percutaneous transluminal coronary angioplasty. Am J Emerg Med. 2005;;23:20–23. [PubMed]


