| Author | Affiliation |
|---|---|
| Michael C Wadman, MD | University of Nebraska Medical Center, Department of Emergency Medicine, Omaha, Nebraska |
| William L Lyons, MD | University of Nebraska Medical Center, Section of Geriatrics and Gerontology, Department of Internal Medicine, Omaha, Nebraska |
| Lance H Hoffman, MD | University of Nebraska Medical Center, Department of Emergency Medicine, Omaha, Nebraska |
| Robert L Muelleman, MD | University of Nebraska Medical Center, Department of Emergency Medicine, Omaha, Nebraska |
ABSTRACT
Introduction:
We hypothesized that a geriatric chief complaint–based didactic curriculum would improve resident documentation of elderly patient care in the emergency department (ED).
Methods:
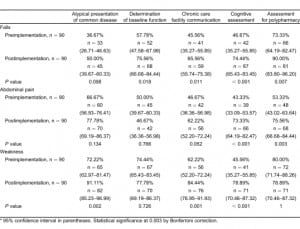
A geriatric chief complaint curriculum addressing the 3 most common chief complaints—abdominal pain, weakness, and falls—was developed and presented. A pre- and postcurriculum implementation chart review assessed resident documentation of the 5 components of geriatric ED care: 1) differential diagnosis/patient evaluation considering atypical presentations, 2) determination of baseline function, 3) chronic care facility/caregiver communication, 4) cognitive assessment, and 5) assessment of polypharmacy. A single reviewer assessed 5 pre- and 5 postimplementation charts for each of 18 residents included in the study. We calculated 95% confidence and determined that statistical significance was determined by a 2-tailed z test for 2 proportions, with statistical significance at 0.003 by Bonferroni correction.
Results:
For falls, resident documentation improved significantly for 1 of 5 measures. For abdominal pain, 2 of 5 components improved. For weakness, 3 of 5 components improved.
Conclusion:
A geriatric chief complaint–based curriculum improved emergency medicine resident documentation for the care of elderly patients in the ED compared with a non–age-specific chief complaint–based curriculum.
INTRODUCTION
Adult learning theory asserts that information presented in the context in which it is used will enhance both the efficiency of the learning process as well as the retention of new knowledge.1 Chief complaint includes curricular components that not only provide contextual knowledge but also address specific segments of the intellectual domain of emergency medicine (EM) as outlined in the Model of Clinical Practice of Emergency Medicine.2,3 The chief complaints included in the model address some presentations specific to the pediatric patient but neglect the age-related differences of geriatric presentations, other than elder abuse. Geriatric chief complaints may represent a high-yield curricular focus area, because geriatric patients account for 12% to 21% of all emergency department (ED) visits and 33% to 56% of hospital admission from the ED.4–7
We hypothesized that a geriatric chief complaint–based didactic curriculum derived from a practice-based curriculum analysis would improve resident documentation of the medical care provided for elderly patients in the ED while optimizing the use of didactic time dedicated to geriatric EM.
METHODS
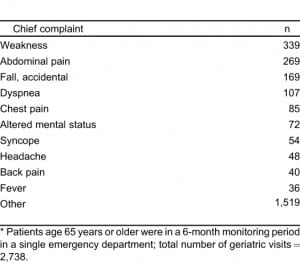
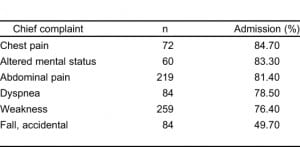
The study protocol was approved by the local institutional review committee. Study subjects included 18 residents: 6 postgraduate year (PGY) 1, 6 PGY2, and 6 PGY3 residents in a PGY1 to PGY3 EM program. Prior to the inception of the geriatric chief complaint lecture series, a general chief complaint lecture series addressing the non–age-specific approach to abdominal pain and weakness as well as other chief complaints related to falls (eg, dizziness, trauma topics) was presented in the first month of the conference schedule. We determined the chief complaints for the new geriatric lecture series through a practice-based curriculum development analysis. For patients 65 years of age or older, we determined the most frequent chief complaints encountered in the ED over a 6-month period by review of electronic records. We then determined the higher acuity chief complaints by hospital admission rates. We developed a geriatric chief complaint curriculum consisting of 1-hour presentations addressing each of the chief complaints determined to be high frequency and high acuity. This was presented by geriatric and EM faculty members as an additional component of the scheduled didactic curriculum.
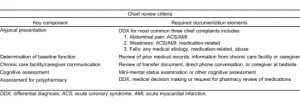
The 3 highest frequency chief complaints—falls, abdominal pain, and weakness—were selected for chart review. A pre- and postcurriculum implementation chart review assessed each resident’s documentation of key components derived from the model of care for elders in the ED developed by the Society for Academic Emergency Medicine Geriatric Task Force as follows: differential diagnosis/patient evaluation considers atypical presentations of common diseases, determination of baseline function, chronic care facility/caregiver communication, cognitive assessment, and assessment of polypharmacy.8,9 The criteria for the chart review for each key component, developed prior to the initiation of the study, are listed in Table 1. For atypical presentation, charts were required to have 1 of the listed atypical presentations. Charts with 2 or more of the listed chief complaints were categorized according to the primary diagnosis entry.
Each resident (n = 18) received 5 pre- and postimplementation documentation reviews performed by a single reviewer blinded to whether the documentation was completed in the pre- or postimplementation time period, within 6 months preceding and 6 months after implementation of the geriatric chief complaint curriculum. Residents documented patient encounters by using an electronic ED information system (WellSoft Corporation, Somerset, New Jersey). We calculated 95% confidence intervals for pre- and postimplementation chart review measures and determined statistical significance by 2-tailed z test for 2 proportions, with statistical significance at 0.003 by Bonferroni correction.
RESULTS
All residents in the EM residency program participated in the study. The participants included 6 residents per class for 3 residency classes currently in training (n = 18). All participants attended the 3 faculty presentations that addressed the selected chief complaints. The 3 most frequent chief complaints for patients 65 years or older were weakness, abdominal pain, and falls, and all 3 accounted for high hospital admission rates (Tables 2 and 3). Each resident received 5 pre- and 5 postimplementation chart reviews (for a total of 90 pre-implementation and 90 postimplementation charts) for each chief complaint.
For the selected chief complaint of falls, 1 of 5 measures demonstrated statistically significant improvement; only cognitive assessment improved by a significant margin (Table 4). For the chief complaint of abdominal pain, cognitive assessment and assessment of polypharmacy demonstrated statistically significant improvement in documentation of the measures, whereas differential diagnosis/patient evaluation, which considers atypical presentations of common diseases, determination of baseline function, and chronic care facility/caregiver communication, were not significantly different. For weakness, differential diagnosis/patient evaluation, which considers atypical presentations of common diseases, chronic care facility/caregiver communication, and cognitive assessment, demonstrated statistically significant improvement. Conversely, determination of baseline function and assessment of polypharmacy were not significantly improved from the pre-implementation measurements.
DISCUSSION
Clinical presentation or chief complaint–based curricular components may meet the curricular needs of many postgraduate medical training programs. Didactic instruction in EM is especially well suited to the clinical presentation curriculum model. The clinical practice of EM requires the recognition of patterns in a patient’s presentation suggestive of a specific diagnosis. Patients rarely present to the ED with a known diagnosis but rather with a chief complaint that represents a set of clinical signs and symptoms. For the specialty of EM, the evaluation of chief complaints comprises an important segment of the intellectual domain for the specialty, as defined in The Model of Clinical Practice of Emergency Medicine.2 The model refers to clinical pattern recognition as “both the hallmark and cornerstone of the clinical practice of EM, guiding the diagnostic tests and therapeutic interventions during the entire patient encounter.”2(p746) For most EM residency programs, didactic curriculum follows the Model of the Clinical Practice of Emergency Medicine—a framework that is based initially on organ system pathology, with subsequent inclusion of general chief complaints. Although the model includes a general consideration of age as a component of physician tasks, no specific chief complaints are identified as geriatric curricular components. Geriatric EM curricula in the medical literature recommend the inclusion of specific geriatric chief complaints, such as abdominal pain, in residency curricula.10 However, The Model of the Clinical Practice of Emergency Medicine, as well as current Residency Review Committee for Emergency Medicine requirements, do not include geriatric-specific chief complaints. They only address elder abuse and neglect as the sole geriatric condition.3 Program directors and other decision makers in graduate medical education must identify the chief complaints worthy of specific geriatric focus in a residency curriculum, if any.
Others have noted the lack of geriatric EM in residency program curricula.11,12 One program designed to increase geriatric education of EM residents, the Geriatrics Education for Specialty Residents (GSR) Program, funded by the John A. Hartford Foundation, supported our study. GSR provides funding for specialty-specific initiatives from academic training centers to develop, initiate, and evaluate programs designed to increase geriatric education of residents in anesthesiology, EM, general surgery and surgical subspecialties, gynecology, physical medicine and rehabilitation, and urology.13 Despite the efforts of programs such as GSR to include geriatrics in the didactic curricula of subspecialty training programs, Accreditation Council for Graduate Medical Education (ACGME) mandated program requirements addressing specific geriatric curricular components are lacking.14The Residency Review Committee for Emergency Medicine requires evidence of teaching the approach for the evaluation and management of general chief complaints of patients presenting to the ED, such as abdominal pain, but it does not require specific demographic considerations, such as geriatric abdominal pain.15 Our findings revealed that, prior to the current study, our EM residency program included general chief complaint didactics but lacked geriatric clinical presentations. Although our past curriculum met ACGME program requirements, we determined from our practice analysis that high-frequency, high-acuity clinical presentations in the elderly—specifically abdominal pain, weakness, and falls—were neglected. This lack of geriatric EM training during residency was confirmed by studies addressing the past residency training of practicing emergency physicians, a majority of whom indicated that inadequate time was spent on geriatric EM.16
The inclusion of general chief complaints in the requirements for EM residency programs resulted from a practice analysis performed by experts from the American College of Emergency Physicians and the University Association for Emergency Medicine (the current Society for Academic Emergency Medicine). This initial practice-based curriculum development model led to the publication of the Core Content of EM, and subsequent revisions resulted in The Model of Clinical Practice of Emergency Medicine.2–4 On a local level, we performed a similar practice analysis to optimize the use of increasingly limited didactic time, and our selection of high-yield segments of the EM problem domain addressing the geriatric chief complaints followed a practice-based curriculum development model. Prior to the study, the didactic curriculum for our training program lacked a structured geriatric EM curriculum, with only 4 hours of geriatric topics (1.4%) of a total of 286 hours. The 4 hours included ACGME-mandated topics addressing the identification and management of elder abuse and trauma topics with special consideration of the geriatric patient.14 The orientation month included a chief complaint lecture series addressing abdominal pain, weakness, and the general approach to the trauma patient, but it did not include geriatric-specific topics. To optimize didactic time, the amount of time devoted to a specific curricular component should reflect the relative importance of the knowledge and/or skill to clinical practice. The number of topics covered in the didactic curriculum is additionally limited by duty-hour regulations, making the selection of high-yield topics critical to the effectiveness of the training program. Practice-based curriculum development allows for a focus on curricular components that meet the educational definition of high yield, either high frequency or high acuity.
Finally, although we postulated that clinical presentation–based learning would improve medical care of elders by residents in the ED on the basis of theoretical grounds, little objective data existed to support our hypothesis prior to our study. One key measure of the efficacy of a curricular component is retention of knowledge by the learners. Improved learning and retention of knowledge are central to successful instruction, and 1 prior study suggests that presentation-based instruction results in improved retention of medical knowledge.17 Our findings also suggest that the new medical knowledge acquired through the geriatric chief complaint–based curriculum resulted in an improvement in patient care as documented in the medical records for these patients.
LIMITATIONS
The study findings are limited by 2 major factors. The first and most significant limitation is that the data from our study were collected through a chart review rather than through direct bedside observation of the residents’ clinical activities. Thus, we may misinterpret documentation deficiencies as deficiencies in patient care or medical knowledge. However, because the described limitation impacts both the pre- and postimplementation chart reviews, it is likely that deficiencies in resident documentation would be evenly distributed between pre- and postimplementation charts. Charts were also reviewed by a single reviewer, limiting our ability to assess the consistency of the chart review.
Second, progressive clinical experience and attending-resident interactions are both highly variable and highly influential. Clearly, as residents progress through training and benefit from increased clinical experience, the patient care they provide and their documentation of this care are likely to improve. Another variable aspect of the resident’s clinical experience during this study period is the input of the attending physician for each case. Because different attending physicians provided clinical supervision, their inputs on each case presentation likely affected the patient care and documentation of each encounter.
CONCLUSION
A geriatric chief complaint–based curriculum derived from a practice-based curriculum analysis improved EM resident documentation of the approach to the care of elderly patients in the ED compared with a non–age-specific chief complaint–based curriculum, as evidenced by improved documentation of patient encounters.
Footnotes
Supervising Section Editor: Teresita M. Hogan, MD
Submission history: Submitted September 23, 2009; Revision received May 7, 2010; Accepted October 18, 2010
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2010.10.1722
Address for Correspondence: Michael C. Wadman, MD
University of Nebraska College of Medicine, Department of Emergency Medicine, 981150 Nebraska Medical Center, Omaha, NE 68198-1150
E-mail: mwadman@unmc.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Knowles MS. The Adult Learner: A Neglected Species. 4th ed. Houston, TX: Gulf Publishing Company;; 1990. pp. 35–44.
2. Hockberger RS, Binder LS, Graber MA, et al. The Model of the Clinical Practice of Emergency Medicine. Ann Emerg Med. 2001;;37:745–770. [PubMed]
3. 2007 EM Model Review Task Force, Thomas HA, Beeson MS, et al. The 2005 Model of the Clinical Practice of Emergency Medicine: the 2007 update. Ann Emerg Med. 2008;;52:e1–e17.
4. Gerson LW, Skvarch L. Emergency medical service utilization by the elderly. Ann Emerg Med.1982;;11:610–611. [PubMed]
5. Sanders AB. Care of the elderly in emergency departments: conclusions and recommendations.Ann Emerg Med. 1992;;21:830–834. [PubMed]
6. Sanders AB. Older persons in the emergency department. J Am Geriatr Soc. 2001;;49:1390–1392.[PubMed]
7. Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med.2002;;39:238–247. [PubMed]
8. Meldon SW, Ma OJ, Woolard R. Geriatric Emergency Medicine. New York, NY: McGraw-Hill;; 2004. pp. 1–3.
9. Wilber ST, Gerson LW. A research agenda for geriatric emergency medicine. Acad Emerg Med.2003;;10:251–260. [PubMed]
10. Jones J, Dougherty J, Cannon L, et al. A geriatrics curriculum for emergency medicine training programs. Ann Emerg Med. 1986;;15:1275–1281. [PubMed]
11. Wilber ST, Gerson LW, Terrell KM, et al. Geriatric emergency medicine and the 2006 Institute of Medicine reports from the committee on the future of emergency care in the U.S. Health System.Acad Emerg Med. 2006;;13:1345–1351. [PubMed]
12. Berger E. Geriatrics and the IOM: did report forget the elderly? Ann Emerg Med. 2006;;48:723–725. [PubMed]
13. Eisner J. The Geriatrics Education for Specialty Residents (GSR) program. The American Geriatrics Society Web site. 2009. Available at:http://specialists.americangeriatrics.org/gsr_program.php#overview. Accessed August 7.
14. Bragg EJ, Warshaw GA. ACGME requirements for geriatric medicine curricula in medical specialties: progress made and progress needed. Acad Med. 2005;;80:279–285. [PubMed]
15. Accreditation Council for Graduate Medical Education (ACGME) ACGME program requirements for graduate medical education in emergency medicine. ACGME Web site. 2009. Available at:http://www.acgme.org/acWebsite/downloads/RRC_progreq/110emergencymed07012007.pdf. Accessed August 7.
16. McNamara RM, Rousseau E, Sanders AB. Geriatric emergency medicine: a survey of practicing emergency physicians. Ann Emerg Med. 1992;;21:796–801. [PubMed]
17. Woloschuk W, Mandin H. Retention of basic science knowledge: a comparison between body system-based and clinical presentation curricula. Teach Learn Med. 2004;;16:116–122. [PubMed]


