| Author | Affiliation |
|---|---|
| William C Manson, MD | Emory University, Department of Emergency Medicine, Atlanta, Georgia |
| James G Ryan, MD | New York Hospital Queens, Department of Emergency Medicine, Queens, New York |
| Heidi Ladner, MD | New York Hospital Queens, Department of Emergency Medicine, Queens, New York |
| Sanjey Gupta, MD | New York Hospital Queens, Department of Emergency Medicine, Queens, New York |
ABSTRACT
Introduction:
We compared the immediate cosmetic outcome of metallic foreign-body removal by emergency medicine (EM) residents with ultrasound guidance and conventional radiography.
Methods:
This single-blinded, randomized, crossover study evaluated the ability of EM residents to remove metallic pins embedded in pigs’ feet. Before the experiment, we embedded 1.5-cm metallic pins into numbered pigs’ feet. We randomly assigned 14 EM residents to use either ultrasound or radiography to help remove the foreign body. Residents had minimal ultrasound experience. After a brief lecture, we provided residents with a scalpel, laceration kit, a bedside portable ultrasound machine, nipple markers, paper clips, a dedicated radiograph technician, and radiograph machine 20 feet away. After removal, 3 board-certified emergency physicians, who were blinded to the study group, evaluated the soft-tissue model by using a standardized form. They recorded incision length and cosmetic appearance on the Visual Analog Scale.
Results:
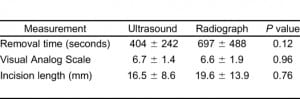
In total, 28 foreign bodies were removed. No significant difference in the time of removal (P = 0.12), cosmetic appearance (P = 0.96), or incision length (P = 0.76) was found.
Conclusion:
This study showed no difference between bedside ultrasound and radiography in assisting EM residents with metallic foreign-body removal from soft tissue. No significant difference was found in removal time or cosmetic outcome when comparing ultrasound with radiography.
INTRODUCTION
Foreign bodies embedded in soft tissue present a diagnostic and therapeutic dilemma to emergency physicians (EP). Patients often complain of the sensation of a foreign body under the skin, but conventional radiography often provides little information to the EP except in the case of metallic foreign bodies. In addition, a significant amount of litigation results from retained foreign bodies not discovered by EPs.1
The typical foreign body is often metal, glass, wood, or plastic. Materials such as plastic and wood are very difficult to visualize on radiographs, but recent studies have shown that EPs can identify these foreign bodies with excellent accuracy by using bedside ultrasound.2–4 Traditionally, the EP might attempt to remove the foreign body or refer the patient to a surgeon. Concerns about the cosmetic outcome of the wound often limit the physician’s ability to remove the foreign body successfully. Removal of a foreign body by an EP or surgeon may result in extensive devitalized tissue and a jagged wound larger than the original. However, no study to date has evaluated whether EPs might achieve an improved cosmetic outcome when using bedside ultrasound to remove a foreign body.
The objective of this study is to determine whether ultrasound guidance of foreign-body removal improves cosmetic outcome. Our hypothesis was that the overall cosmetic outcome would be no different when using bedside ultrasound compared with conventional radiography, but the time to foreign-body removal would be less with ultrasound.
METHODS
Study Design
This study was a single-blinded, crossover, randomized, in vitro study of the ability of EPs to remove pins embedded in pigs’ feet, by using ultrasound guidance and traditional radiography. The study was approved by the Institutional Review Board. The study was conducted in the emergency department (ED) of an academic teaching hospital, separate from patient-care areas but near the radiograph machine.
Inclusion Criteria/Subjects
We included 14 emergency medicine (EM) residents from a 3-year EM residency program as our subjects. Seven residents were in the first year, and 7, in their second year of training. Two of the 14 residents had completed an organized ultrasound elective, which is a required rotation during the second year of residency. We obtained consent from each participating resident. We randomized subjects to begin the study with either ultrasound or radiography to avoid bias in second-attempt improvement.
Interventions
In the preparation for the in vitro model, pigs’ feet were numbered for identification purposes. The principal investigator used a hemostat to embed a 1.5-cm metallic pin into each of the pig’s feet. Each pin was embedded at approximately 30 degrees to the surface and 1 cm below the surface. The pins were placed in random directions, relative to the toe.
Before the experiment, we presented to the residents a 30-minute lecture on foreign-body localization and removal techniques. Equal weight was placed on conventional radiographs and ultrasound techniques.
Each subject was asked to remove pins from 2 different pigs’ feet. When using radiography, the resident was provided with nipple markers, paper clips, a dedicated radiography suite located 20 feet from the worksite, and a radiography technician dedicated to the study. Two orthogonal radiograph images were taken of the pig’s foot, including anterior–posterior and lateral views. The SonoSite Titan (SonoSite, Inc, Bothell, Washington) portable bedside ultrasound machine was placed at the work sites of residents assigned to ultrasound. Residents used the superficial 10–5 MHz linear probe to locate the foreign bodies. All residents used the same probe. For both procedures, we provided subjects with a standard laceration-repair kit and a disposable number 10 scalpel. We did not provide residents a standoff pad or saline offset to identify the foreign body with ultrasound. We did not allow residents to inject fluid into the pig’s foot to affect visualization on ultrasound.
As the residents used ultrasound to identify and remove the foreign body, we instructed them to use dynamic rather than static guidance. For the purpose of this study, we defined dynamic guidance as direct visualization of the foreign body with ultrasound while guiding the hemostat to the foreign body. We defined static guidance as identifying the foreign body with ultrasound, putting the probe aside, and then proceeding with the removal. We did not require residents to demonstrate real-time visualization of the hemostat tip touching the foreign body. We encouraged residents to keep the linear transducer in contact with the skin of the pig’s foot, but did not require it.
Measurements
During the experiment, we recorded the time elapsed to remove the foreign body. Research assistants performed the time recording. The assistants had no research duties other than stopping and starting the stopwatch. Timing began when the resident approached the bedside and ended when the foreign body was removed. When using radiographs, time included marking the pig’s foot, transporting the model, performing and interpreting the radiograph, and removing the foreign body. When using ultrasound, time began when the subject turned on the ultrasound machine and ended when the foreign body was removed. The subjects were not allowed to ask for assistance when removing the foreign body or interpreting the radiograph or ultrasound image.
After removal of all foreign bodies, 3 reviewers rated the cosmetic outcome of each pig’s foot. All 3 reviewers are board-certified EPs with at least 5 years of experience in EM. We recorded the overall cosmetic appearance according to the Visual Analog Scale (VAS), a validated scale for cosmetic outcomes.5–7 In addition, we recorded the length of the incision. The reviewers were blinded to imaging modality and to the identity of the resident who performed the procedure.
Statistical Analysis
To determine differences in time, VAS, and incision length, we analyzed the matched-pair data by using the Wilcoxon Signed-Rank Test. We calculated an inter-rater agreement by using an intraclass correlation coefficient based on the mixed model. We performed all analyses by using SAS statistical software (SAS Institute, Inc, Cary, North Carolina); P < 0.05 was considered significant.
RESULTS
In total, 14 subjects performed the removal of 28 foreign bodies. All 28 foreign bodies were removed. No significant difference was noted between the removal time for ultrasound and radiographs (404 seconds and 698.6 seconds; P = 0.1189). No significant difference were present between the mean VAS for ultrasound and radiographs (6.7 versus 6.6; P = 0.96). No significant difference occurred between the mean incision length by using ultrasound compared with radiograph (16.5 mm versus 19.6 mm; P = 0.76). See Table.
To determine the agreement in cosmetic scoring between the 3 evaluators, we calculated a correlation coefficient. The intraclass correlation coefficient was 0.77 for the VAS.
DISCUSSION
The results of the study showed that ultrasound was not significantly different from conventional radiography for metal foreign bodies before removal in regard to cosmetic outcome, length of incision, and time used in the ED. Nevertheless, a trend favored the use of ultrasound, in regard to length of time. This study chose not to examine the setup time of bedside ultrasound, as this issue varies significantly within different hospitals.
Traditionally, the EP localizes a foreign body with conventional radiographs and clinical skill. However, this method gives the EP only a general guide to locate the foreign body. Recent studies have shown that EPs can accurately locate various foreign bodies with bedside ultrasound.3,4,8,9These studies have also used in vitro models such as a chicken leg, pig foot, or human cadaver. In addition, ultrasound has been shown to improve the outcome of central venous access of the internal jugular vein when dynamically used during the procedure.10–12 However, this study intended to show that the EP could also use dynamic bedside ultrasound guidance during removal of a foreign body to improve the cosmetic outcome. A randomized controlled study with live human beings would not be possible for ethical reasons. However, the flesh of a chicken leg or pig’s foot resembles human flesh and is an inexpensive and effective way of simulating a human study.
Although localization of foreign bodies has been studied, no one has yet studied removal under dynamic ultrasound guidance. This is the first study to evaluate the actual removal of a soft-tissue foreign body under dynamic assistance with ultrasound. In 1991, Schlager et al9 first studied the use of bedside ultrasound to locate soft tissue foreign bodies. However, it was only in 1997 that any literature suggested dynamic procedural guidance with bedside ultrasound to remove a foreign body. By using a soft-tissue model, Turner et al8 concluded that ultrasound located soft-tissue foreign bodies of all types. Although they suggested the potential use of dynamic ultrasound-guided retrieval, they did not study the removal of foreign bodies. Schlager13 provides a summary of the sonographic localization of soft-tissue foreign bodies, and also mentions the potential for dynamic ultrasound-guided removal. Orlinsky et al2 in 2000 showed that EPs with minimal training have similar success with soft-tissue foreign body localization with ultrasound, when compared with experienced ultrasound technicians. Additionally, Dean et al14 described a novel technique of using a water-filled latex glove as an acoustic window to enhance the ability of ultrasound to identify soft-tissue foreign bodies. More recently, studies have shown that certain institutions are regularly using ultrasound guidance to remove various foreign bodies.15,16 However, no study has yet compared the effectiveness of dynamic ultrasound guidance with conventional radiographic localization.
Because many previous authors have theorized that dynamic, ultrasound-guided soft-tissue foreign-body removal might be superior, the authors of this study were surprised that this small study did not show a dramatic benefit. By extrapolating the SOAP-3 trial, in which Milling et al10 demonstrated improved success with ultrasound-guided central venous access, one might assume that ultrasound would facilitate the removal of soft-tissue foreign bodies. However, this initial study suggests that ultrasound guidance is at least as good as conventional radiography. Time of removal was not statistically different between the ultrasound and radiograph groups. In addition, cosmetic outcome showed no statistical difference. However, it is possible that the results could be different if additional subjects were studied, or if the studied subjects had greater levels of training in both ultrasound and foreign-body removal. Additionally, further studies are needed to determine whether ultrasound is superior to radiography for other radiolucent foreign bodies, such as plastic and organic matter.
The authors also firmly believe that routine use of conventional radiographs to locate foreign bodies is not indicated. Certainly, a subset of cases favors plain films, such as deep-tissue metallic or glass foreign bodies. However, a recent article by Orlinsky et al17 strongly argued against routine use of radiographs in cases of suspected superficial foreign bodies. Their study indicated that radiographs gave more information than physical examination alone in only 1.5% of patients. Given these findings, we did not choose to study the comparison between radiographs plus ultrasound versus radiographs alone. However, a recent review article (Weinberger et al18) noted a prevalence rate of 0.6% to 4.3% of retained foreign bodies detected by radiography after adequate exploration. Perhaps another way to look at this study’s results is that ultrasound performed as well as radiography. Nevertheless, many EPs may find more comfort in obtaining a radiograph first, and then using the ultrasound to assist dynamically in removal.
LIMITATIONS
The current study was limited by only studying metallic foreign bodies, which are easily identified by conventional radiography. Ultrasound is most useful in identifying radiolucent foreign bodies, such as plastic or wood. The previously quoted studies demonstrated that ultrasound and radiography have similar abilities in locating metallic foreign bodies; however, ultrasound is superior to radiographs in locating plastic, wood, and other organic matter. We believe that these foreign bodies are more frequently encountered in daily practice and are more easily missed. Additionally, organic matter foreign bodies are more likely to cause an inflammatory reaction, and thus more likely to produce a poor outcome. The authors chose to compare the removal of metallic foreign bodies, as it more fairly compared the 2 methods. Nevertheless, a strict interpretation of the data of this study does not allow generalization of the results to other types of foreign bodies. However, ultrasound is likely superior to radiographs in removal of plastic and wood foreign bodies, given that this article suggests that ultrasound is at least as good as radiography in assisting metallic foreign-body removal. Further studies will be needed to confirm these suspicions.
In addition to the issues discussed, this study has other limitations. This study did not explore the incidence of extension of initial incision or the creation of a second incision. Furthermore, all foreign bodies were removed, which is not consistent with actual practice in EM. Residents were asked to continue with the procedure until the foreign body was removed, which is when recording time stopped. Also, the subjects were EM residents in their first or second year of training. Bedside ultrasound and radiography interpretation are both actively taught during the residency, and none of the residents claimed to be an expert in foreign-body removal. The residents were still in the process of learning how to perform ultrasound and interpret radiographs, and therefore were not fully proficient with these skills. Further training in EM would likely serve to improve the cosmetic outcome and minimize time equally in both groups. Additionally, we chose to use an in vitro model, because a live human model was impractical for ethical reasons. The authors believe that the pig’s-foot model was a reasonable and inexpensive alternative. Additionally, the final cosmetic appearance was not studied, as the deceased pigs’ feet were not capable of wound closure and healing. This study examined cosmesis only immediately after removal, rather than 2 weeks after healing of the wound.
Despite the unfamiliarity with pig-foot anatomy and advanced ultrasound techniques, the residents were not given assistance from other physicians when interpreting the radiograph or ultrasound. A human cadaver would also have been a reasonable model, but the pig’s foot was much more accessible and inexpensive, making the study easier to reproduce. Also, we chose not to use a water bath or standoff pad in this study. As Dean et al14 demonstrated, the fluid-filled latex glove may improve the acoustics of image acquisition. However, we thought the acoustic spacer would interfere with incision and removal of the foreign body.
Last, the authors chose not to study the set-up time for ultrasound to make the study more applicable to other EDs and patient populations. Although this artificial construction facilitates the research study, the reality may be different in the clinical setting. Even in well-organized EDs, some time is spent searching for the portable ultrasound machine. In some EDs, a staff member will position the ultrasound machine at the bedside for the physician; however, most EPs must locate, transport, and set up the machine themselves. Set-up time for radiography also varies from place to place and does not take into account waiting for radiographs when several patients are ahead in line. In this study, the radiography technician was dedicated to the pigs’ feet “patients.” In actual ED conditions, the patient will be waiting in a queue with other patients, often out of the control of the EP. Even though the setup for ultrasound takes time of the physician, it is under complete control of the EP. However, in a real-time situation, it may be more efficient to order the radiograph and come back to the patient in 20 minutes.
CONCLUSION
Given that prior studies showed that EPs were able to locate soft-tissue foreign bodies with ultrasound, it would seem a natural conclusion that bedside ultrasound would assist with removal. However, this study shows no advantage of time or cosmetic outcome with real-time use of the portable ultrasound in removing metallic foreign bodies from soft tissue. Nevertheless, this represents the most challenging comparison between ultrasound and radiography. Further studies will likely demonstrate that non–radio-opaque foreign bodies are more easily removed with the dynamic assistance of ultrasound. In particular, removal with ultrasound guidance should be considered in patients with poor follow-up or in patients that insist on removal in the ED. Additionally, the physician may consider obtaining radiographs before ultrasound removal. This study did not attempt to evaluate physicians with significant skill with ultrasound, such as those that have completed EM ultrasound fellowships. It is the belief of the authors that the more-relevant question involves novice sonologists, as that represents the majority of practicing EPs. In the end, this study supports an EP’s comfort level or skill with removal of soft tissue foreign bodies, with the assistance of either radiographs or bedside ultrasound.
Footnotes
Supervising Section Editor: J. Christian Fox, MD
Submission history: Submitted February 28, 2010; Revision received June 3, 2010; Accepted July 6, 2010
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2010.6.1885
Address for Correspondence: William C. Manson, MD
Emory University, Department of Emergency Medicine, 49 Jesse Hill Jr Dr, Atlanta, GA 30303
E-mail: wmanson@emory.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Kaiser CW, Slowick T, Spurling KP, et al. Retained foreign bodies. J Trauma. 1997;;43:107–111.[PubMed]
2. Orlinsky M, Knittel P, Feit T, et al. The comparative accuracy of radiolucent foreign body detection using ultrasonography. Am J Emerg Med. 2000;;18:401–403. [PubMed]
3. Saboo SS, Saboo SH, Soni SS, et al. High-resolution sonography is effective in detection of soft tissue foreign bodies: experience from a rural Indian center. J Ultrasound Med. 2009;;28:1245–1249. [PubMed]
4. Crystal CS, Masneri DA, Hellums JS, et al. Bedside ultrasound for the detection of soft tissue foreign bodies: a cadaveric study. J Emerg Med. 2009;;36:377–380. [PubMed]
5. Karounis H, Gouin S, Eisman H, et al. A randomized, controlled trial comparing long-term cosmetic outcomes of traumatic pediatric lacerations repaired with absorbable plain gut versus nonabsorbable nylon sutures. Acad Emerg Med. 2004;;11:730–735. [PubMed]
6. Holger JS, Wandersee SC, Hale DB. Cosmetic outcomes of facial lacerations repaired with tissue-adhesive, absorbable, and nonabsorbable sutures. Am J Emerg Med. 2004;;22:254–257. [PubMed]
7. Mattick A, Clegg G, Beattie T, et al. A randomised, controlled trial comparing a tissue adhesive (2-octylcyanoacrylate) with adhesive strips (Steristrips) for paediatric laceration repair. Emerg Med J.2002;;19:405–407. [PMC free article] [PubMed]
8. Turner J, Wilde CH, Hughes KC, et al. Ultrasound-guided retrieval of small foreign objects in subcutaneous tissue. Ann Emerg Med. 1997;;29:731–734. [PubMed]
9. Schlager D, Sanders AB, Wiggins D, et al. Ultrasound for the detection of foreign bodies. Ann Emerg Med. 1991;;20:189–191. [PubMed]
10. Milling TJ, Jr, Rose J, Briggs WM, et al. Randomized, controlled clinical trial of point-of-care limited ultrasonography assistance of central venous cannulation: the Third Sonography Outcomes Assessment Program (SOAP-3) Trial. Crit Care Med. 2005;;33:1764–1769. [PubMed]
11. Gann M, Jr, Sardi A. Improved results using ultrasound guidance for central venous access. Am Surg. 2003;;69:1104–1107. [PubMed]
12. Caridi JG, Hawkins IF, Jr, Wiechmann BN, et al. Sonographic guidance when using the right internal jugular vein for central vein access. AJR Am J Roentgenol. 1998;;171:1259–1263. [PubMed]
13. Schlager D. Ultrasound detection of foreign bodies and procedure guidance. Emerg Med Clin North Am. 1997;;15:895–912. [PubMed]
14. Dean AJ, Gronczewski CA, Costantino TG. Technique for emergency medicine bedside ultrasound identification of a radiolucent foreign body. J Emerg Med. 2003;;24:303–308. [PubMed]
15. Callegari L, Leonardi A, Bini A, et al. Ultrasound-guided removal of foreign bodies: personal experience. Eur Radiol. 2009;;19:1273–1279. [PubMed]
16. Visvanathan V, McGill D, Singh S, et al. Ultrasound-assisted removal of an airgun pellet from the hand. J Plast Reconstr Aesthet Surg. 2008;;61:234–235. [PubMed]
17. Orlinsky M, Bright AA. The utility of routine x-rays in all glass-caused wounds. Am J Emerg Med.2006;;24:233–236. [PubMed]
18. Weinberger LN, Chen EH, Mills AM. Is screening radiography necessary to detect retained foreign bodies in adequately explored superficial glass-caused wounds? Ann Emerg Med. 2008;;51:666–667. [PubMed]


