Original Research
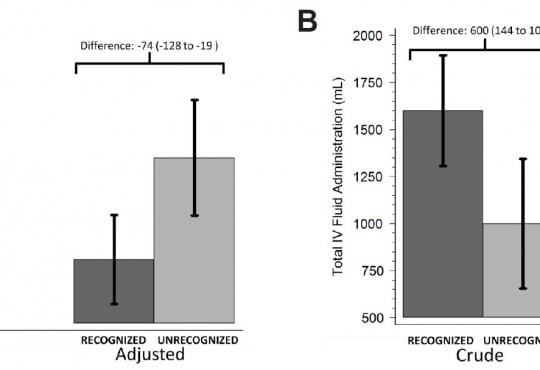
Population Health Research Design
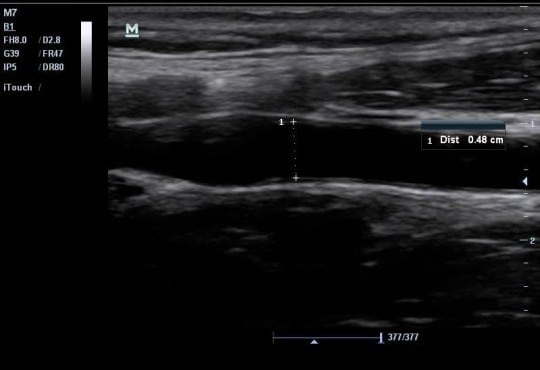
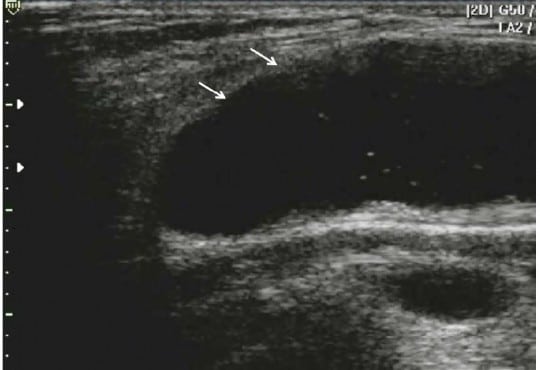
Validation of ICD-9 Codes for Stable Miscarriage in the Emergency Department
Westjem Read More
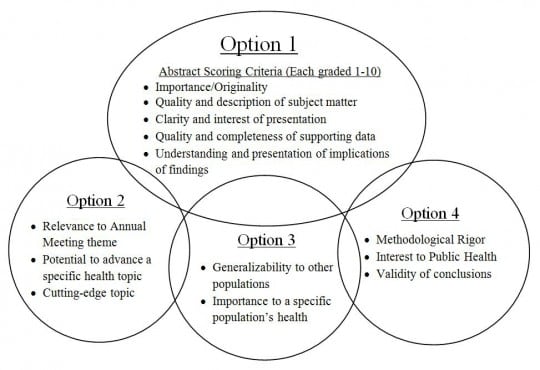
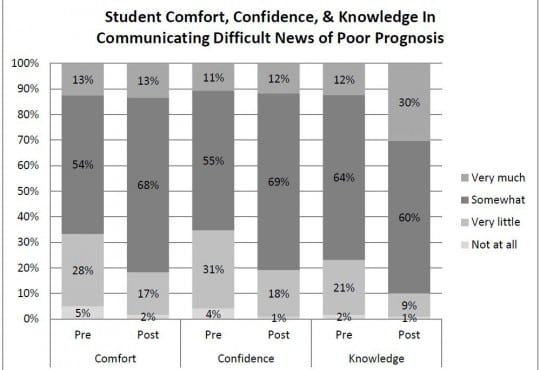
Population Health Research Design
How do Medical Societies Select Science for Conference Presentation? How Should They?
Westjem Read More
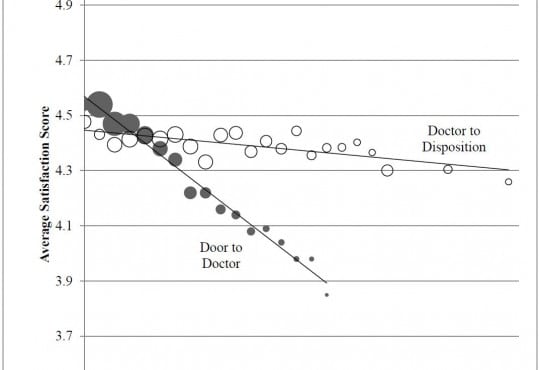
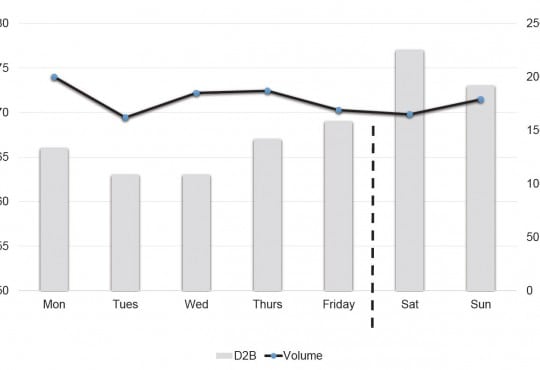
Emergency Department Operations