| Author | Affiliation |
|---|---|
| Vu Huy Tran, MD | Albert Einstein College of Medicine, Jack D. Weiler Hospital, Bronx, New York |
| Mathew Nelson, DO | Hofstra North Shore-LIJ School of Medicine, Department of Emergency Medicine, Hempstead, New York |
| Joshua Nogar, MD | Hofstra North Shore-LIJ School of Medicine, Department of Emergency Medicine, Hempstead, New York |
| Robert M. Bramante, MD | Hofstra North Shore-LIJ School of Medicine, Department of Emergency Medicine, Hempstead, New York |
Introduction
Case report
Discussion
ABSTRACT
Ketamine associated urinary dysfunction has become increasingly more common worldwide. Point-of-care ultrasound (POCUS) is an established modality for diagnosing hydronephrosis in the emergency department. We describe a case of a young male ketamine abuser with severe urinary urgency and frequency in which POCUS performed by the emergency physician demonstrated bilateral hydronephrosis and a focally thickened irregular shaped bladder. Emergency physicians should consider using POCUS evaluate for hydronephrosis and bladder changes in ketamine abusers with lower urinary tract symptoms. The mainstay of treatment is discontinuing ketamine abuse.
INTRODUCTION
Ketamine induced urinary dysfunction (KAUD) is a syndrome first described in the literature in 2007. Patients suffer from irritative lower urinary tract symptoms and can develop varying degrees of hydronephrosis and interstitial cystitis. We describe a case of a young man with a history of heavy ketamine abuse who presented to the emergency department (ED) with lower urinary tract irritation and flank pain.
Why should an emergency physician (EPs) be aware of this?
Although previously unreported in United States ED literature, ketamine associated urinary dysfunction has become increasingly more common in EDs worldwide. Point-of-care ultrasound (POCUS) is an established modality for diagnosing hydronephrosis in the ED. EPs should consider using POCUS evaluate for hydronephrosis and bladder changes in ketamine abusers with lower urinary tract symptoms. The mainstay of treatment is discontinuing ketamine abuse.
CASE REPORT
Twenty four-year-old Chinese-American male with a history of ketamine abuse (3–5 times daily for 4 years), as well as cocaine and intravenous drug abuse, who presented to the ED with bilateral flank pain for 2 weeks. He noted 2 days of increasing pain, described as dull, waxing and waning. Associated symptoms included fever, chills, urinary frequency, dysuria, urgency, and more recently, urinary incontinence (requiring diapers). There was no history of weakness, bowel incontinence, or saddle anesthesia. On physical examination, the patient appeared uncomfortable and anxious. He complained of severe urgency, requiring frequent urination during the interaction. Mild bilateral costo-vertebral tenderness was noted, with an otherwise unremarkable abdominal and genitourinary examination. Neurologic examination was normal except for slight ataxia when performing tandem gait.
The treating ED physician performed POCUS that revealed bilateral moderate hydroureteronephrosis and a contracted bladder with an irregular shape and areas of focal wall thickening. The patient complained of frequency and urgency throughout the study and requested multiple times to pause the exam to urinate. Pain was elicited on suprapubic transducer application.
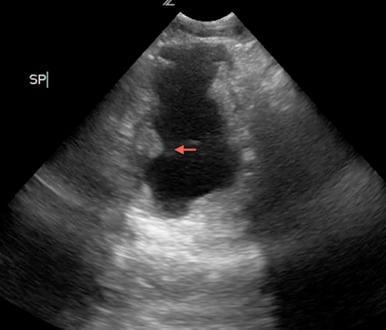
Figure 2
Transverse view of the bladder shows a small, irregularly shaped bladder wall with areas of focal thickening (arrow).
Laboratory studies revealed an elevated creatinine (1.32 mg/dL) and urinalysis was positive for red blood cells (5–10/high powered field), white blood cells (10–25/hpf), few bacteria, protein (75 md/dL) and trace leukocyte esteraste. The remainder of his lab work (CBC, chemistry, coagulation profile) was negative.
A computed tomography was ordered to rule out obstructive pathology and ultimately confirmed our POCUS findings. The final reading was “moderate bilateral hydroureteronephrosis, and a small deformed urinary bladder.” A urology consult was obtained. An outpatient workup was recommended for ketamine induced urinary tract disease. The patient was sent home with antibiotics for a urinary tract infection and encouraged to discontinue ketamine abuse. Upon review, the urine culture was negative and the patient was lost to follow up.
DISCUSSION
Ketamine is an N-methyl-D-aspartate receptor antagonist, used therapeutically as a dissociative anesthetic. Recreationally, it is frequently abused at raves, parties, and nightclubs. Patients with acute ketamine toxicity most often present to EDs with neurologic complaints such as confusion, loss of consciousness, agitation, and drowsiness. Recent literature suggests that many patients with chronic ketamine abuse also experience ketamine-associated urinary tract dysfunction (KAUD). To our knowledge, this is the first case of KAUD associated with bilateral hydronephrosis reported from a United States ED. This may be due to the fact that recreational ketamine occurs with much higher frequency outside the U.S., especially in East and South-East Asian countries.1–3
Ketamine associated urinary tract dysfunction (KAUD) is a syndrome first described by Shahani et al in 2007.4 Since then, there has been over 110 cases reported in the literature.5 About 20–30% of patients who abuse ketamine suffer from lower urinary tract symptoms (LUTS).6,7 Since most cases of KAUD have been reported in case reports, case series, and letters, the true prevalence of this disease is unknown. In a recent large community–based study, Pal et al1, report a prevalence of LUTS of 30% among recent users. Furthermore, they conclude that recent ketamine users had increased odds of LUTS compared with non-users.
The exact mechanism of ketamine associated urinary destruction is unknown. Some proposed mechanisms include: direct epithelial damage, microvascular injury, or immune-related damage to the urinary tract by ketamine or its metabolites.6,9 Damage to the lower urinary tract damage is more common than upper urinary tract, although the latter occurs relatively frequently. These symptoms can be attributed to chronic inflammation, low bladder capacities, decreased bladder compliance, and/or detrusor overactivity.9 Symptoms can become quite debilitating, causing frequent urination every 15–45 minutes, as described in our case.
Currently, this disease entity is a diagnosis of exclusion that typically occurs after ruling-out obstructive lesions. Patients with severe irritative lower urinary tract symptoms, a history of ketamine abuse, and no other cause for symptoms should be considered to have KAUD.5 We believe point-of-care ultrasound is a safe, rapid, first-line imaging modality to consider in patients with suspected KAUD. POCUS for the detection of hydronephrosis in the ED has a sensitivity and specificity of 80–87% and 82–83%, respectively.10,11 In addition, it is rapid, available, and free of ionizing radiation. One limitation of POCUS is the ability to rule out obstructing lesions and masses.
Although the true incidence of positive findings of renal and bladder ultrasound in patients with KAUD is unknown, recent case series and reports suggest sonographic findings are frequent. Mason et al12 reported that 12 of 23 patients in their case series had positive finding on renal ultrasound that included bladder wall thickening and small bladder volumes. Thirteen percent of these patients were found to have upper urinary tract involvement. Four patients were unable to fill their bladder and had to stop in the middle of the exam to empty their bladders.12
Chu et al9 described 59 patients from two hospitals in Hong Kong with ketamine-associated cystitis. Fifty-one percent of these patients had unilateral hydronephrosis, while 44% had bilateral hydronephrosis. They report that most of these patients showed hydronephrosis and hydroureter that extended down to the vesiculo-uteric junction. It is postulated that upper tract involvement likely results from long-term decrease in bladder compliance.9,12 Tsai et al8, reported 5 of 11 patients in their case series had bilateral hydronephrosis. These patients exhibited detrusor overactivity with small bladder capacities on urodynamic studies.8
Currently, the mainstay of therapy has been the discontinuation of ketamine use. Most patients have sterile pyuria where antibiotics are ineffective.9 Other treatment modalities have included antimuscarinics and steroids, which have demonstrated limited efficacy for KAUD.8 Surgical interventions (augmentation enterocystoplasty, ureteroplasty, cystectomy9, and ileal neobladder12) have been performed for patients with continued use and refractory symptoms.
Ketamine associated urinary dysfunction is becoming an increasingly common and recognized syndrome associated with chronic ketamine abuse. Emergency physicians should consider the use of point-of-care ultrasound as a first-line imaging modality in patients with suspected KAUD. Patients should be advised to discontinue ketamine abuse and referred to a urologist to exclude alternative causes.
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Robert M. Bramante, MD. Hofstra North Shore-LIJ Medical Center Department of Emergency Medicine, 300 Community Drive, Manhasset, NY 11030. Email: rbramante@nshs.edu. 7 / 2014; 15:382 – 384
Submission history: Revision received November 24, 2013; Submitted March 10, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 Pal R, Balt S, Erowid E Ketamine is associated with lower urinary tract signs and symptoms. Drug Alcohol Depend. 2013; 132:189-194
2 Morgan EJ, Curan HV Ketamine use: a review. Addiction. 2012; 107:27-38
3 Wood D, Cottrell A, Baker SC Recreational ketamine: from pleasure to pain. BJU Int. 2011; 107:1881-1884
4 Shahani R, Streutker C, Dickson B Ketamine-associated ulcerative cystitis: a new clinical entity. Urology. 2007; 69:810-812
5 Middela S, Pearce I Ketamine-induced vesicopathy: a literature review. Int J Clin Pract. 2011; 65:27-30
6 Chu PS, Ma WK, Wong SC The destruction of the lower urinary tract by ketamine abuse: a new syndrome?. BJU Int. 2008; 102:1616-1622
7 Muetzelfeltdt L, Kamboj SK, Rees H Journey through the K-hole: phenomenological aspects of ketamine use. Drug Alcohol Depend. 2008; 95:219-229
8 Tsai TH, Cha L, Lin CM Ketamine-associated bladder dysfunction. Int J Urol. 2009; 16:826-829
9 Chu PS, Kwok SC, Lam KM Street ketamine – associated bladder dysfunction: a report of ten cases. Hong Kong Med J. 2007; 13:311-313
10 Watkins S, Bowra J, Sharma P Validation of emergency physician ultrasound in diagnosing hydronephrosis in ureteric colic. Emerg Med Australas. 2007; 19:188-195
11 Gaspari RJ, Horst K Emergency Ultrasound and Urinalysis in the Evaluation of Flank Pain. Acad Emerg Med. 2005; 12:1180-1184
12 Mason K, Cottrell AM, Corrigan AG Ketamine-associated lower urinary tract destruction: a new radiological challenge. Clin Radiol. 2010; 65:795-800