| Author | Affiliation |
|---|---|
| Abigail Hankin, MD, MPH | Emory University School of Medicine, Department of Emergency Medicine, Atlanta, Georgia |
| Stanley Wei, MD | Saint Joseph’s Mercy Care Services, Atlanta, Georgia |
| Juron Foreman, MD | Emory University School of Medicine, Department of Emergency Medicine, Atlanta, Georgia |
| Debra Houry, MD, MPH | Emory University School of Medicine, Department of Emergency Medicine, Atlanta, Georgia |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction:
Homicide is the second leading cause of death among youth aged 15–24. Prior cross-sectional studies, in non-healthcare settings, have reported exposure to community violence, peer behavior, and delinquency as risk factors for violent injury. However, longitudinal cohort studies have not been performed to evaluate the temporal or predictive relationship between these risk factors and emergency department (ED) visits for injuries among at-risk youth. The objective was to assess whether self-reported exposure to violence risk factors in young adults can be used to predict future ED visits for injuries over a 1-year period.
Methods:
This prospective cohort study was performed in the ED of a Southeastern US Level I trauma center. Eligible participants were patients aged 18–24, presenting for any chief complaint. We excluded patients if they were critically ill, incarcerated, or could not read English. Initial recruitment occurred over a 6-month period, by a research assistant in the ED for 3–5 days per week, with shifts scheduled such that they included weekends and weekdays, over the hours from 8AM-8PM. At the time of initial contact in the ED, patients were asked to complete a written questionnaire, consisting of previously validated instruments measuring the following risk factors: a) aggression, b) perceived likelihood of violence, c) recent violent behavior, d) peer behavior, e) community exposure to violence, and f) positive future outlook. At 12 months following the initial ED visit, the participants’ medical records were reviewed to identify any subsequent ED visits for injury-related complaints. We analyzed data with chi-square and logistic regression analyses.
Results:
Three hundred thirty-two patients were approached, of whom 300 patients consented. Participants’ average age was 21.1 years, with 60.1% female, 86.0% African American. After controlling for participant gender, ethnicity, or injury complaint at time of first visit, return visits for injuries were significantly associated with: hostile/aggressive feelings (Odds ratio (OR) 3.5, 95% Confidence interval (CI): 1.3, 9.8), self-reported perceived likelihood of violence (OR 10.1, 95% CI: 2.5, 40.6), and peer group violence (OR 6.7, 95% CI: 2.0, 22.3).
Conclusion:
A brief survey of risk factors for violence is predictive of increased probability of a return visit to the ED for injury. These findings identify a potentially important tool for primary prevention of violent injuries among at-risk youth seen in the ED for trauma-related and non-traumatic complaints.
INTRODUCTION
Violent injury is a disturbingly common phenomenon among North American youth. Injuries due to violence are the second leading cause of death among adolescents aged 15–191 and accounted for over 600,000 visits to U.S. hospitals in 2008.2 The consequences of violence during the adolescent and young adult years go far beyond the physical injuries, and include depression, post-traumatic stress disorder (PTSD), substance use, and poor academic achievement. Furthermore, several studies suggest that non-fatal violent injuries in adolescents often precede fatal violence and homicides,3,4 a fact that underscores the importance of identifying at-risk youth before violence escalates.
Emergency departments (EDs) are an important societal safety net, serving patients who are acutely ill or are unable to obtain medical care through other clinical settings.5 In many communities, EDs are the only providers of medical care for patients who are uninsured or under-insured.6 Due to this unique role of EDs in our society, they have been identified as important sites for screening and prevention of public health problems. Examples of public health interventions that have been implemented via ED-based screening and education/prevention efforts include: HIV testing and education,7 screening and interventions for victims of Intimate Partner Violence,8 as well as risky drug/alcohol use.9
In several communities across the U.S., EDs and trauma departments have implemented interventions aimed at preventing future violence among youth who present after a violent injury.10 However, it is important to note that the majority of ED-based violence-prevention programs have focused on secondary and tertiary prevention of violence, enrolling patients only after an initial hospital visit due to violence, with only 1 published study that focused on primary prevention of peer aggression and violence among patients presenting to the ED, regardless of presenting complaint.11
In this study we sought to determine if specific violence risk factors could be used to identify young adults at risk for an ED visit for an injury-related complaint over a 1-year period after an initial ED visit for any complaint (trauma-related or non-trauma-related) to allow targeted use of violence prevention resources and services.
METHODS
Study Design
This study utilized a prospective cohort design, using an initial survey of risk factors among patients presenting to the ED for any complaint, with follow up at 12 months via electronic medical record review.
Setting
Enrollment took place in the ED of a large, urban safety-net hospital in the Southeastern U.S. The ED sees over 105,000 patient visits annually. During the time this study was completed, this ED served as the metropolitan region’s only Level I trauma center and its only public hospital.
Protocol
Eligible patients were 18–24 years old, presenting to the ED for any complaint during study hours. Patients were excluded if they were critically ill, incarcerated, had an acute psychiatric emergency, or if they were unable to read or write in English.
A research assistant (RA) approached all eligible patients, and informed them about the study. The research assistant had a master’s degree in public health, and received specialized training about clinical research ethics and study subject recruitment. The RA was present in the ED for 8-hour shifts, 3 to 5 days per week, from June through December 2009, varying to include weekends and weekdays, and to include patients presenting during the day as well as the evening.
The questionnaire was composed of 6 different survey instruments, which were selected based on survey risk factors identified in the literature as being associated with increased risk of violence.12 The survey has previously been described in our initial study.13 Briefly, we assessed: Hostile/aggressive behavior, using the Hostility portion of the Product-Symptom Checklist-90.14 Self-perceived likelihood of violence, and recent history of violent behavior were measured using Likelihood of Violence and Delinquency Scale and Aggressive Behavior Scales of the Sage Baseline Survey, respectively.15 We assessed peer-group violence using the Friend’s Delinquent Behavior scale from the Denver Youth Survey,16 and exposure to community violence was assessed using the Children’s Exposure to Community Violence survey.17
The full survey instrument consisted of a 6-page multiple-choice survey, which required approximately 10–15 minutes for completion. The RA was trained to approach patients only during natural periods of waiting during the ED visit (in the waiting room, while awaiting transport for a test, or while awaiting a test result); the survey was administered either in a private patient care area, or, if the patient was in the waiting room, they were escorted to an adjacent private area to complete the survey. Participants were offered a $5 gift certificate to compensate for their time.
We classified participants as high or low risk according to previously described methods.13 We defined “high risk” exposure as a response higher than the midpoint on a given scale, e.g., 4 or greater out of 5 possible responses on more that 50% of items within a given assessment.
We performed follow up via medical record review at 12 months following the index visit. For completion of record review, the patients’ electronic medical records were reviewed to determine whether they had had any subsequent return visits to the ED, and, if a visit had occurred, whether that visit was due to an injury-related complaint. Designation of visits as injury-related vs. non-injury related was made based on review of a) chief complaint as recorded by the triage nurse, b) history of present illness as recorded by the physician(s) caring for the patient, and (c) final diagnosis/diagnostic code. If any of these elements suggested that the patient’s visit had been prompted by an injury, we counted the patient as an “Injury Visit.” Review of all charts was completed by two emergency physicians based on pre-determined diagnostic criteria, and inter-rater reliability was calculated. Due to limitations in patient disclosure and clinician documentation (Rodriguez, 1999), we did not attempt to discriminate between intentional versus unintentional etiology of injury.
Statistical Analysis
We analyzed data using SAS 9.3 (SAS Institute, Inc., Cary, NC). We used logistic regression to estimate the odds ratio (OR) of return visit for injury comparing those with and without violence risk factors. A multivariate analysis using logistic regression was performed to estimate the OR of return visit for injury while controlling for potential confounding by known risk factors for violence, including gender, race/ethnicity (specified as Non-Hispanic Black versus other), and initial ED visit for violence. Inter-rater reliability for chart review results was determined using Cohen’s kappa statistic calculation.
RESULTS
The RA approached 332 patients, of whom 300 patients consented; medical record abstractions were performed on 286 of these patients. (We excluded14 patients because their medical chart could not be located – a hospital-wide transition from paper charts to electronic medical records was completed between the initial survey and follow-up completion, and may have contributed to loss of some follow-up data). Among the 286 patients, participants’ average age was 21.1 years, with 167 (60.1%) female, 240 (86.0% Non-Hispanic Black, 15 (5.4%) Non-Hispanic White, and 11 (4.7%) Hispanic. One-hundred eighty-eight (34.3%) participants reported a high rate of exposure to at least one risk factor for violence, as measured by the survey instrument (Figure). When evaluated by specific risk categories, 42 (14.7%) participants reported hostile or aggressive impulses, 15 (5.2%) reported that they anticipated that they would participate in violent behavior in the near future, and 17 (5.9%) participants reported recent participation in violence. Twenty-three (8.0%) participants reported exposure to high rates of peer group violence, 62 (21.7%) participants reported exposure to high rates of community violence, and 21 (7.3%) reported a negative future outlook (Table 1).
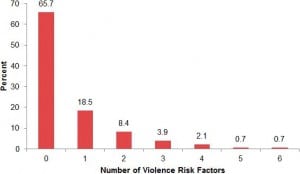
Co-occurrence of violence risk factors among 286 patients in a Southeastern emergency department.
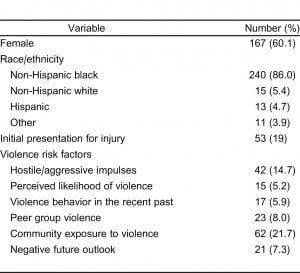
Demographic and violence risk factors among 286 patients presenting to a Southeastern emergency department and included in the analytic cohort.
Of the 286 participants initially enrolled in the study, based on medical record review at 12 months following initial visit, 62 (21.7%) patients were seen for repeat ED visit during the follow-up period, with 18 (6.3%) seen in the ED for a visit due to an injury-related complaint during the 12 month follow-up period. Inter-rater reliability for the return visits analysis was excellent, with a kappa >0.9.
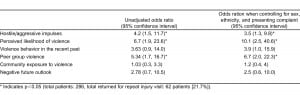
Return visit for injury at 12 months was positively associated with high risk factor exposure at the initial ED visit. When adjusted for ethnicity, sex, and presenting complaint, patients who reported high rates of hostile/aggressive feelings showed an odds ratio of 3.5 (95% Confidence Interval [CI]: 1.3, 9.8) for return injury visit, compared with those who did not show high rates of hostile/aggressive feelings. Participants who reported a high likelihood of future violent behavior showed an odds ratio of 10.1 (95% CI: 2.5, 40.6) for return injury visit. We also observed a statistically significant relationship with patients who reported peer group violence (OR 6.7, 95% CI: 2.0, 2.3); recent violent behavior was just below the threshold for statistical significance (OR 3.9, 95% CI: 1.0, 15.9) (Table 2).
DISCUSSION
This study assessed the correlation between patients’ responses to a written survey about exposures to risk factors for violence with those patients’ risk of returning to the ED for an injury-related complaint in the subsequent 12 months. We found that patients’ report of risk factor exposure was strongly predictive of a return visit for an injury complaint, and that the relationship between survey results and injury visit remained significant even when controlling for factors traditionally associated with injury, including sex, race, and reason for initial ED visit.
With respect to specific risk factor exposures, we found that peer group violence, self-reported likelihood of future violence, and responses on a scale of hostile/aggressive impulses were all significantly associated with risk of repeat visit for violence, whereas community exposure to violence, report of violent behavior in the recent past, and negative future outlook were not significantly associated with risk of repeat visit for injury. Much of the existing literature about trauma recidivism has previously focused on demographics and on characteristics of the initial traumatic event – such as mechanism of injury, rather than individual risk factor exposure among patients.18–21 One small, single-site study did descriptively assess characteristics of young adults who were seen for a repeat incident of trauma within a 4-year span, and identified living “in a neighborhood where crime is pervasive” as a common characteristic, but did not compare the group with recurrent violence with patients who had presented for only a single violent injury.22 Another study, using a sample of 100 adolescent and young adult trauma victims, did find factors including use of weapons, history of fighting, and past arrests to be associated with increased risk of firearm injury versus other causes of injury, and “use of alcohol on weekdays, past arrest, and higher education levels” to be associated with recurrent injury.23 The high prevalence of reported exposure to community violence across patients who did and did not experience repeat injury visits might mask more subtle differences in exposures to community violence and/or presence of “safe havens” in some communities that may ameliorate the effects of community violence exposure. Additionally, self-report of recent violent behavior, while not statistically significant in this sample, does show a trend towards an effect; given the small sample size, and potential patient concerns about disclosing recent violence perpetration, this relationship might be predictive of repeated injury visits in a larger cohort, and/or if patients are more confident of the confidentiality of information disclosed through the survey, such as if the survey were administered through a computer interface rather than on paper.24
These findings suggest the potential for the use of the risk factor survey as a means of identifying youth at risk for future injury, and for directly targeting those youth at risk for violent injury.
Compared to untargeted interventions, prevention interventions that focus on patients who screen positive for the risk factors studied would allow for a more focused use of resources and would allow clinicians and social service agencies to provide services focused specifically on those individuals at highest risk for violent injury.
LIMITATIONS
This study faces several limitations. First, the study was conducted at a single ED, situated in the inner city of a large city; further, multi-site studies would be necessary to determine the extent to which these finding would generalize beyond the study population. Although this study is limited by the geographical setting of the study site, it is important to emphasize the importance of understanding and addressing the causes of violence in settings like the study site. Public hospitals in large urban centers treat patients at high risk for violent injuries, and focusing prevention efforts in these settings has the potential for broad impact on rates of violent injury in the U.S.
An additional limitation is the use of medical record data to identify return visits for injury complaints. While this method faces the risk of patients being lost to follow up if a patient was seen at another hospital for an injury complaint, this method was chosen because it offered more accurate and inclusive follow-up data at 12 months, when compared with alternative methods, such as follow up via personal surveys or via the trauma registries. While patients may have been lost to follow up due to injury visits to other EDs, the probability of loss to follow up was mitigated by the choice of a study site that served as the only public hospital and the only Trauma 1 Center serving the metropolitan area. When considering potential missed patients in the medical record follow up, it is unlikely that there would have been a systemic bias in losses to follow up which would have biased the findings of this study.
Finally, a relatively small number of patients (6%) of the total sample returned for an injury visit at one year following initial visits. While this number was enough to find statistically significant relationships, repeating the study with multiple sites and a larger initial sample would allow for narrower confidence intervals, a more precise assessment of relative risk relationships, and a better understanding of the observed relationship between the risk factors and the injury outcome. Additionally, a relatively small number of patients in the original sample reported risk factor exposure, again suggesting a benefit to studying this survey’s predictive value in a larger patient population or across multiple clinical sites.
CONCLUSION
In this study we found a high correlation between ED patient’s reports of exposure to risk factors for violence (including peer group violence, self-assessed risk of future violence, and hostile/aggressive feelings) and return visit to the ED for injury complaints, with odds ratios ranging from 3.5 to 10.1. These findings remained significant even when controlling for patient gender, ethnicity, and patient complaint at initial visit (i.e., injury vs. non-injury complaint). These findings suggest a new approach to studying risk factors for repeat ED visits for traumatic injuries among young adults seen in the ED, and suggest a novel approach by which EDs and/or trauma services might identify a high-risk population that might benefit from targeted interventions to prevent injuries before they occur. Future research should explore how these separate scales or items from the scales may be combined to optimally identify this high-risk population.
ACKNOWLEDGMENT
This work was funded by the Emory Center for Injury Control, which provided the pilot grant through CDC grant 5R49 CE001494.
Footnotes
Supervising Section Editor: Monica H. Swahn, PhD, MPH
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.