| Author | Affiliation |
| Catherine S. Erickson, MD | Oregon Health and Science University, Department of Emergency Medicine, Portland, Oregon |
| Michael M. Liao, MD, MSc | Denver Health Medical Center, Department of Emergency Medicine, Denver, Colorado; University of Colorado School of Medicine, Department of Emergency Medicine, Aurora, Colorado; Colorado School of Public Health, Department of Epidemiology, Aurora, Colorado |
| Jason S. Haukoos, MD, MSc | Denver Health Medical Center, Department of Emergency Medicine, Denver, Colorado; University of Colorado School of Medicine, Department of Emergency Medicine, Aurora, Colorado |
| Erica Douglass, MD | Denver Health Medical Center, Department of Emergency Medicine, Denver, Colorado; University of Colorado School of Medicine, Department of Emergency Medicine, Aurora, Colorado |
| Margaret DiGeronimo, MD | Denver Health Medical Center, Department of Emergency Medicine, Denver, Colorado; University of Colorado School of Medicine, Department of Emergency Medicine, Aurora, Colorado |
| Eric Christensen, RN | Denver Health Medical Center, Department of Emergency Medicine, Denver, Colorado |
| Emily Hopkins, MSPH | Denver Health Medical Center, Department of Emergency Medicine, Denver, Colorado |
| Brooke Bender, MPH | Denver Health Medical Center, Department of Emergency Medicine, Denver, Colorado |
| John L. Kendall, MD | Denver Health Medical Center, Department of Emergency Medicine, Denver, Colorado; University of Colorado School of Medicine, Department of Emergency Medicine, Aurora, Colorado |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Our primary objective was to describe the time to vessel penetration and difficulty of long-axis and short-axis approaches for ultrasound-guided small vessel penetration in novice sonographers experienced with landmark-based small vessel penetration.
Methods
This was a prospective, observational study of experienced certified emergency nurses attempting ultrasound-guided small vessel cannulation on a vascular access phantom. We conducted a standardized training, practice, and experiment session for each participant. Five long-axis and five short-axis approaches were attempted in alternating sequence. The primary outcome was time to vessel penetration. Secondary outcomes were number of skin penetrations and number of catheter redirections. We compared long-axis and short-axis approaches using multivariable regression adjusting for repeated measures, vessel depth, and vessel caliber.
Results
Each of 10 novice sonographers made 10 attempts for a total of 100 attempts. Median time to vessel penetration in the long-axis and short-axis was 11 (95% confidence interval CI [7-12]) and 10 (95% CI [6-13]) seconds, respectively. Skin penetrations and catheter redirections were equivalent and near optimal between approaches. The median caliber of cannulated vessels in the long-axis and short-axis was 4.6 (95% CI [4.1-5.5]) and 5.6 (95% CI [5.1-6.2]) millimeters, respectively. Both axes had equal success rates of 100% for all 50 attempts. In multivariable regression analysis, long-axis attempts were 32% (95% CI [11%-48%]; p=0.009) faster than short-axis attempts.
Conclusion
Novice sonographers, highly proficient with peripheral IV cannulation, can perform after instruction ultrasound-guided small vessel penetration successfully with similar time to vessel penetration in either the long-axis or short-axis approach on phantom models. [West J Emerg Med. 2014;15(7):824-830.]
INTRODUCTION
Many emergency department (ED) patients are characterized as having difficult peripheral intravenous (IV) access due to underlying medical conditions, such as obesity, dehydration, and a history of intravenous drug abuse. Historically, failed attempts at peripheral IV access lead to physician-attempted central venous access. However, placing central venous catheters is costly and puts patients at increased risk for complications.1
An alternative for those with difficult IV access is the placement of IV peripheral catheters under ultrasound guidance. Prior studies have shown that physicians, nurses, and technologists can use ultrasound guidance to obtain successful peripheral venous access when landmark approaches have failed.2-4 However, suboptimal technique leads to unnecessary early complications and morbidity; including posterior wall penetration, arterial punctures, hematoma formation, excessive needle punctures and redirections within the skin, and delays in obtaining access.5 Long-axis and short-axis approaches remain the primary methods for ultrasound guidance. Each has distinct advantages and disadvantages that may either increase or decrease complications.6
To our knowledge, there are only a few prior studies comparing long-axis and short-axis approaches. These studies found short-axis to be faster, but each reported different times to vessel penetration and complications.7-9 Ultrasound-guided vessel cannulation requires combining skills in cannulation and ultrasound usage. Prior studies were potentially confounded by the inclusion of sonographers with varying proficiency with standard landmark IV placement. Studying ultrasound-guided approaches may be improved by removing inexperience in placing peripheral lines as a confounding factor.
The primary aim of this study was to describe the time to vessel penetration and difficulty of long-axis and short-axis approaches for ultrasound-guided small vessel penetration in novice sonographers experienced with landmark-based small vessel cannulation.
METHODS
This was a prospective observational study of novice sonographers performing vessel penetration on block phantom models designed to simulate peripheral vessels to assess the performance of long-axis and short-axis approaches. The novice sonographers were proficient in placing landmark-guided peripheral intravenous lines. The Colorado Multiple Institutional Review Board approved this study.
The inclusion criteria were full-time nurses at our institution who were both registered nurses and certified emergency nurses who had no prior hands-on ultrasound experience. Denver Health Medical Center is a Level I trauma center with an annual census of approximately 55,000 annual ED patient visits. All certified emergency nurses at our institution have extensive experience with the technical skill of obtaining landmark-based IV access.
The primary outcome was time to vessel penetration. Secondary outcomes were number of skin penetrations and number of catheter redirections. Time to vessel penetration was defined as the time from placing the ultrasound probe on the phantom surface to successful penetration. We defined successful vessel penetration as the point at which artificial blood became visibly present in the catheter chamber and the needle tip was confirmed by real-time ultrasound as being within the vessel lumen. Both artificial blood and needle tip were required before time was stopped. A skin penetration was defined as the number of times the catheter penetrated the phantom surface and was completely withdrawn prior to vessel penetration. We defined a catheter redirection as any insertion of the catheter after the first insertion that was visibly different from the preceding axis of insertion without fully withdrawing the catheter.
All data were collected over two consecutive days. Each subject received one hour of didactics followed by hands-on instruction by the principal study investigator. The didactic session included a description of ultrasound physics, transducer orientation, vessel identification, and techniques for performing ultrasound guidance of vessel penetration. Each subject practiced vessel identification without attempting cannulation on a volunteer human model to demonstrate proficiency with both approaches. Following didactics and the hands-on training, each subject was given two practice attempts on a single phantom model.
Ultrasound guidance was performed in real-time using a General Electric (Fairfield, CT) LOGIQ e with a 4-12 MHz linear transducer. All subjects used a single operator technique. Five different phantom block models (Blue Phantom, Kirkland, WA) were used for the study. Each block was of similar size, but contained two or more vessels with slight differences in vessel position, depth, and caliber.
Immediately following the two practice attempts, subjects performed 10 vessel penetrations using ultrasound guidance, alternating between using long-axis and short-axis approaches. Subjects, blinded to the study question, could initially decide which axis approach to begin with, but subsequent attempts followed an alternating sequence. Only one short-axis and one long-axis approach were attempted on each block phantom before moving on to the next block phantom. Subjects were not allowed to access the same vessel twice. Additionally, once a vessel was identified, and the first skin puncture attempted, subjects could not change the axis approach or the target vessel.
Two first-year emergency medicine residents blinded to the study purpose and trained by the principal investigator performed data collection. Residents were trained by the principal investigator in data collection on the same model until no errors were made in data collection. They recorded time to vessel penetration, number of skin penetrations, and number of catheter redirections. They also confirmed that when the flash was visualized, ultrasound images confirmed that the needle tip was in the vessel lumen. After successful vessel penetration, the observer measured the target vessel’s depth and caliber using the ultrasound machine. The reference point under which measurements were obtained was the point of catheter entry into the target vessel. We defined vessel depth as the distance from the phantom’s surface to the anterior wall of the target vessel. Vessel caliber was defined as the distance from the anterior to posterior wall of the target vessel.
Descriptive statistics included median and 95% confidence intervals (CI). We estimated CI for medians using percentile bootstrap with 2,500 repetitions.10 The difference between long-axis and short-axis was calculated as long-axis minus short-axis for each outcome. Given nonparametric paired data, we used the Wilcoxon signed rank sum test with associated binomial exact 95% CI for bivariate comparison. We stratified data into attempts 1 through 5 prior to analysis, each attempt representing one single pair of long-axis and short-axis consecutive attempts; attempt 1 corresponding to the first long-axis and short-axis attempts, and attempt 5 corresponding to the last long-axis and short-axis attempts.
We also performed multivariable analyses to evaluate the relationship between long-axis and short-axis approaches and the outcomes, while adjusting for repeated measures and potential confounders. The comparison of long-axis versus short-axis for the primary outcome of time to vessel penetration was performed using a multivariable linear mixed model accounting for two within subject repeated measures, namely axis and attempts.11 We adjusted the model for vessel depth and vessel caliber to control for potential confounding. Additionally, the outcome of time to vessel penetration was log transformed to address non-normal residuals. Interaction terms were not evaluated in the model. For the secondary outcomes of skin penetration and catheter redirection, we performed a multivariable generalized linear model with a Poisson distribution accounting for the two within subject repeated measures of axis and attempts. The model was again adjusted for vessel depth and vessel caliber, and no interaction terms were evaluated in this secondary model. Significance was defined as p <0.05 for all analyses. No adjustment for multiple comparisons was performed, nor did we performa priori power calculation. All statistical analyses were performed using SAS Version 9.2 (SAS Institute, Inc., Cary, NC) or Stata Version 10.1 (Stata Corporation, College Station, TX).
RESULTS
We studied 10 subjects, each completing 10 attempts at vessel penetration on a phantom mode, for a total of 100 attempts (50 in short-axis and 50 in long-axis). There were no missing data. Subjects had a median of seven (IQR 5 to 10) years of experience as registered nurses and a median of two (IQR 1 to 4) years of experience as certified emergency nurses.
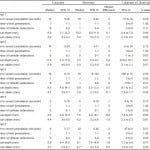
Median time to vessel penetration in the long-axis was 11 seconds (95% CI [7-12]) and for the short-axis was 10 seconds (95% CI [6-13]). For long-axis, skin penetrations and catheter redirections were 1 (95% CI [1-1]) and 0 (95% CI [0-0]), respectively; and for short-axis, 1 (95% CI [1-1]) and 0 (95% CI [0-1]), respectively. The median caliber of cannulated vessels in the long-axis was 4.6 (95% CI [4.1-5.5]) millimeters and in the short-axis was 5.6 (95% CI [5.1-6.2]) millimeters. Median depth of cannulated vessel in the long-axis and short-axis were 8.9 (95% CI [7.4-11.8]) and 7.9 (95% CI [7.4-10.2]) millimeters, respectively.
The median times to vessel penetration in the long-axis and short-axis are reported in the table for each pair of attempts (i.e., long-axis and short-axis done consecutively). Bivariate analysis comparing long-axis versus short-axis showed that no significant differences existed for time to vessel penetration, skin penetration, or catheter redirection. Differences were present in vessel depth and vessel caliber between long-axis and short-axis with the long-axis approach allowing novice sonographers to penetrate a slightly smaller and deeper vessel, by approximately one millimeter. Both approaches had near-optimal median counts for skin penetrations and catheter redirections, namely one skin penetration and zero catheter redirection prior to successful vessel penetration.
Table. Summary of data for long-axis and short-axis ultrasound-guided approaches stratified by paired long-axis and short-axis attempts.
Figure. Individual data for all three outcomes versus vessel depth or vessel caliber, stratified by axis approach.
Both long-axis and short-axis had equal success rates of 100% for all 50 attempts in each orientation. For the outcome time to vessel penetration, the final mixed linear model, adjusting for repeated measures, vessel depth, and vessel caliber, showed that the geometric mean of the long-axis attempts was 32% (95% CI 11% to 48%; p=0.009) faster than short-axis attempts. For skin penetration, the multivariable generalized linear model using Poisson distribution, adjusting for repeated measures, vessel depth, and vessel caliber, showed that the prevalence of skin penetrations of the long-axis attempts was 20% (95% CI 93% to -843%; p=0.46) lower than short-axis attempts. For catheter redirections, the multivariable generalized linear model using Poisson distribution, adjusting for repeated measures, vessel depth, and vessel caliber, showed that the prevalence of catheter redirections of long-axis attempts was 73% (95% CI 58% to 83%; p<0.0001) lower than short-axis attempts. A graphical representation of the data for all three outcomes versus vessel depth or vessel caliber, stratified by axis approach is presented in the figure. These graphs show that long-axis attempts tend to cluster more towards the optimal end of the scale for all three outcomes compared to short-axis attempts.
DISCUSSION
Obtaining rapid peripheral IV access is essential for diagnosis and treatment in many ED patients. For patients with difficult IV access, peripheral access using ultrasound guidance has been shown to be an effective alternative to central venous access.2,12,13 Long-axis and short-axis are the two primary approaches to ultrasound guidance of vessel cannulation; however, the optimal approach remains unclear. Our results show that in novice sonographers proficient in landmark placed peripheral catheters, long-axis was 32% faster than short-axis in time to vessel cannulation. Although statistically significant, a 32% improvement in speed translates to only three seconds improvement if 10 seconds is used as the baseline. This suggests no clinically significant difference in our subject population. Number of skin penetrations and catheter redirections were optimal for both approaches.
Blaivas et al. compared directly long-axis versus short-axis in novice sonographers using a phantom model.8 This study found that the short-axis approach was almost three minutes faster than the long-axis approach (mean 2.4 minutes short-axis versus 5.0 minutes long-axis), but they noted that average skin penetrations (mean 4 short-axis versus 6 long-axis) and catheter redirections (mean 14 short-axis versus 18 long-axis) were similar. Our results differ in that our time to vessel penetration was within seconds, not minutes, despite similar definitions of the outcome time to vessel penetration; and that the approach did not significantly influence time to vessel penetration. Additionally, our median skin penetrations and catheter redirections were nearly optimal for both long-axis and short-axis approaches. Although model and ultrasound machine differences may have played a part in these differences, one condition of our study was that all novice sonographers were expert in the technique of landmark-based peripheral IV placement. A potential explanation is that our optimal outcomes were a result of studying subjects proficient in landmark-based peripheral IV placement. Blaivas et al. used emergency medicine residents, and their technical proficiency with IV placement was unclear.
Mahler et al. published a randomized trial comparing short-axis and long-axis approaches on live patients with four practitioners (half of whom were ED nurses) experienced with ultrasound-guided IV access.7 Although also not statistically significant, they found that short-axis was faster than long-axis (median 34 seconds short-axis versus 91 seconds long-axis) for insertion time, defined as time from first needle stick to blood return in catheter. Numbers of skin penetrations were similar (mean 1.5 short-axis versus 1.4 long-axis). Perhaps again, one explanation for their results showing faster access times and fewer complications in comparison with Blaivas et al. is the inclusion of ED nurses who were likely proficient in landmark-based peripheral IV placement.8
Stone et al. studied long-axis versus short-axis in 22 medical students and 17 emergency medicine interns using similar block phantoms.9 Their outcomes were time to visible artificial blood in syringe and, separately, needle-tip visibility based on still images taken at the time of initial artificial blood flash. Time to flash was again faster for short-axis (12.4 seconds) versus long-axis (14.8 seconds), though not statistically significant. Different from our study, confirmation of needle-tip visibility in vessel lumen was not necessary for the time outcome. In fact, based on still images needle tip was only visible in 62% of long-axis attempts and 23% of short-axis attempts. Our results, which showed 100% success in visualizing needle tip in vessel lumen, are potentially related to our use of real-time ultrasound and direct observation as opposed to single still images.
We caution that while our study may provide evidence that practitioners proficient in landmark-based peripheral IV placement can perform ultrasound-guided small vessel penetration in both long axis and short axis with similar rates of vessel penetration, it does not provide evidence that proficiency with landmark-based peripheral IV placement is critical for performing ultrasound guided small vessel cannulation. Our study did not directly address this hypothesis; however, we believe this is an important hypothesis that may benefit from future investigation. We also believe the additional studies with a more robust subject population and with live models or patients, potentially classified as “difficult access” patients, would be useful to expand knowledge in the area of ultrasound guided peripheral access.
LIMITATIONS
One limitation is that our study was performed on a simulated model, not live humans. Although our model is commonly used for teaching purposes, it may not fully simulate the comparable human experience. Ultrasound is most frequently used when patients have had numerous attempts to obtain access (i.e., the difficult access patient). The block model may have important differences compared to this specific population. Our sample size of subjects was small, thus may not be representative of novice sonographers proficient with the technical aspect of IV placement. Our observers who performed data collection were ultrasound interested and had completed the residency ultrasound procedure requirement; however, it is possible with highly specialized ultrasound attending physicians that data collection would be more accurate.
There may be additional, important reasons to prefer short-axis or long-axis in the placement of peripheral IV catheters not considered in our study, including but not limited to sonographer preference, patient factors, ability to visualize needle tip.6,9 Considering additional factors on a per patient basis is important when deciding on the best approach.
It is possible that our definition of successful vessel penetration (an initial “flash” of artificial blood in the catheter chamber and visualization of the needle tip on ultrasound images) may not always represent appropriate placement in the vessel lumen as threading the catheter will increase time to securing a peripheral IV. Specifically, in the short-axis view, sometimes the needle shaft is mistaken for the needle tip within the vessel, and the needle tip has already traveled outside the vessel. It is unclear how frequently this may have occurred. We chose time to vessel penetration because it can be more difficult to thread a small catheter on a phantom model than it is on live subjects; and this is also a potential limitation. This would bias our results by overinflating our success rate and shortening our time to vessel penetration.
CONCLUSION
Novice sonographers, highly proficient with peripheral IV cannulation, can perform after instruction ultrasound-guided small vessel penetration successfully with similar time to vessel penetration in either long- or short-axis approach on phantom models. Optimal technique with ultrasound-guided vessel cannulation may first require proficiency with the technical skill of placing peripheral IV catheters.
ACKNOWLEDGEMENTS
Footnotes
Supervising Section Editor: Shane Summers, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Catherine Erickson, Oregon Health and Science University, Department of Emergency Medicine, 3181 SW Sam Jackson Park Road Portland, OR 97239. Email: erickcat@ohsu.edu.
Submission history: Submitted May 8, 2014; Revision received July 21, 2014; Accepted September 4, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348:1123-33.
- Costantino TG, Parikh AK, Satz WA, et al. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med. 2005;46:456-61.
- Bauman M, Braude D, Crandall C. Ultrasound-guidance vs. standard technique in difficult vascular access patients by ED technicians. Am J Emerg Med. 2009;27:135-40.
- Blaivas M, Lyon M. The effect of ultrasound guidance on the perceived difficulty of emergency nurse-obtained peripheral IV access. J Emerg Med. 2006;31:407-10.
- Kumar A, Chuan A. Ultrasound guided vascular access: efficacy and safety. Best Pract Res Clin Anaesthesiol. 2009;23:299-311.
- Abboud PA, Kendall JL. Ultrasound guidance for vascular access. Emerg Med Clin North Am. 2004;22:749-73.
- Mahler SA, Wang H, Lester C, et al. Short- vs long-axis approach to ultrasound-guided peripheral intravenous access: a prospective randomized study. Am J Emerg Med. 2010.
- Blaivas M, Brannam L, Fernandez E. Short-axis versus long-axis approaches for teaching ultrasound-guided vascular access on a new inanimate model. Acad Emerg Med. 2003;10:1307-11.
- Stone MB, Moon C, Sutijono D, et al. Needle tip visualization during ultrasound-guided vascular access: short-axis vs long-axis approach. Am J Emerg Med. 2010;28:343-7.
- Haukoos JS, Lewis RJ. Advanced statistics: bootstrapping confidence intervals for statistics with “difficult” distributions. Acad Emerg Med. 2005;12:360-5.
- Moser EB. Repeated Measures Modeling with PROC MIXED (Paper 188-29). Cary, NC: SAS Institute, Inc.; 2004.
- Stokowski G, Steele D, Wilson D. The use of ultrasound to improve practice and reduce complication rates in peripherally inserted central catheter insertions: final report of investigation. J Infus Nurs. 2009;32:145-55.
- Stein J, George B, River G, et al. Ultrasonographically guided peripheral intravenous cannulation in emergency department patients with difficult intravenous access: a randomized trial. Ann Emerg Med. 2009;54:33-40.