| Author | Affiliation |
|---|---|
| William J. Meurer, MD, MS | University of Michigan Medical School, Department of Emergency Medicine, Ann Arbor, Michigan University of Michigan Medical School, Department of Neurology, Ann Arbor, Michigan |
| Cemal B. Sozener, MD | University of Michigan Medical School, Department of Emergency Medicine, Ann Arbor, Michigan |
| Zhenzhen Xu, PhD | University of Michigan School of Public Health, Department of Biostatistics, Ann Arbor, Michigan |
| Shirley M. Frederiksen, BSN, MS | University of Michigan Medical School, Department of Emergency Medicine, Ann Arbor, Michigan |
| Allison M. Kade, BA | University of Michigan Medical School, Department of Emergency Medicine, Ann Arbor, Michigan |
| Michael Olgren, MD | Saint Mary’s Healthcare, Department of Emergency Medicine, Grand Rapids, Michigan |
| Sanford J. Vieder, DO | Botsford Hospital, Department of Emergency Medicine, Farmington Hills, Michigan |
| John D. Kalbfleish, PhD | University of Michigan School of Public Health, Department of Biostatistics, Ann Arbor, Michigan |
| Phillip A. Scott, MD | University of Michigan Medical School, Department of Emergency Medicine, Ann Arbor, Michigan |
ABSTRACT
Introduction:
Emergency physician (EP) turnover is a significant issue that can have strong economic impact on hospital systems, as well as implications on research efforts to test and improve clinical practice. This work is particularly important to researchers planning randomized trials directed toward EPs because a large degree of turnover within a physician group would attenuate the effectiveness of the desired intervention. We sought to determine the incidence and factors associated with EP workforce changes.
Methods:
In an attempt to determine EP turnover and workforce change, data from the INSTINCT (INcreasing Stroke Treatment through INterventional behavior Change Tactics) trial were used. The INSTINCT trial is a prospective, cluster-randomized, controlled trial evaluating a targeted behavioral intervention to increase appropriate use of tissue plasminogen activator in acute ischemic stroke. Individual EPs staffing each of the study hospitals were identified at baseline and 18 months. Surveys were sent to EPs at both intervals. Models were constructed to investigate relationships between physician/hospital characteristics and workforce change.
Results:
A total of 278 EPs were identified at baseline. Surveys were sent to all EPs at baseline and 18 months with a response rate of 72% and 74%, respectively. At 18 months, 37 (15.8%) had left their baseline hospital and 66 (26.3%) new EPs were working. Seven EPs switched hospitals within the sample. The total number of EPs at 18 months was 307, a 10.8% overall increase. Among the 24 hospitals, 6 had no EP departures and 5 had no new arrivals. The median proportion of EP workforce departing by hospital was 16% (interquartile range [IQR] = 4%–25%; range = 0%–73%), and the median proportion added was 21% (IQR = 7%–41%; range = 0%–120%). None of the evaluated covariates investigating relationships between physician/hospital characteristics and workforce change were significant.
Conclusion:
EP workforce changes over an 18-month period were common. This has implications for emergency department directors, researchers, and individual EPs. Those planning research involving interventions upon EPs should account for turnover as it may have an impact when designing clinical trials to improve performance on healthcare delivery metrics for time-sensitive medical conditions such as stroke, acute myocardial infarction, or trauma.
INTRODUCTION
Emergency physician (EP) turnover is a considerable issue throughout the country. While there is very limited information available on turnover rates of EPs, current estimates suggest that about 9% of physicians from all specialties leave their practice each year.1 An EP may choose to leave his/her hospital group for one of a variety of reasons, including lack of job satisfaction, desire for geographical change, spousal employment opportunity, or a combination of such factors.2 In addition, the EP may belong to a group or contract organization that loses its contract with a hospital. Turnover significantly impacts hospitals through lost productivity and recruiting and relocation costs; remaining faculty may have decreased morale.3,4
An EP departure from a practice can have multiple effects. As well as having an immediate economic impact on the hospital system,5 departures can also affect efforts to study and improve clinical practice through quality improvement efforts and knowledge translation initiatives. Accounting for EP turnover is important when designing clinical trials to improve performance on healthcare delivery metrics for time-sensitive medical conditions such as stroke, acute myocardial infarction, or trauma. Past work has little information regarding hospital level EP workforce change, with most prior investigations focused on EP decisions to leave the specialty.6,7
Given the importance of estimating EP turnover rates, we have analyzed prospectively collected data on emergency department (ED) practices within the INSTINCT (INcreasing Stroke Treatment through INterventional behavior Change Tactics) trial—a prospective, cluster-randomized, controlled trial evaluating an intervention to increase appropriate use of tissue plasminogen activator (tPA) in acute ischemic stroke. Our primary objective was to estimate and describe EP turnover within Michigan; our secondary objective was to identify provider and hospital level factors which were associated with EP workforce changes.
METHODS
Study Design
This study is based on data collected in the INSTINCT trial. This multi-center, cluster-randomized trial was designed to test the ability of targeted educational interventions to increase the appropriate use of tPA for the treatment of ischemic stroke. Data for this study were obtained from 2 surveys administered to emergency physicians associated with the participating hospitals at times separated by approximately 18 months. These surveys were designed to assess emergency physician attitudes, beliefs, and behavior regarding acute stroke treatment as part of the overall trial protocol, but also provided data over time allowing us to analyze EP turnover during the study period. The design and reporting of this study was facilitated by the recommendations of the STROBE statement, a reporting guideline considered essential for good reporting of observational studies.8
Human Subjects Protection
The University of Michigan Institutional Review Board (IRBMED) and local IRBs approved the INSTINCT trial and the surveys.
Study Setting and Population
Emergency physicians in practice at hospitals participating in the INSTINCT trial were included. Physicians were determined to be in practice by the local principal investigator and were included if they were in a permanent position at the participating site. Residents were not included. The intervention within INSTINCT was randomized at the hospital level. Hospitals were selected from the population of acute care hospitals in Michigan. Hospitals were excluded if they were affiliated with the INSTINCT emergency medicine residency, self-identified as an academic comprehensive stroke center, experienced more than 100,000 annual ED visits, or experienced fewer than 100 annual inpatient stroke discharges. These design elements were used to facilitate matched pairs of hospitals to serve as control and intervention sites within the overall trial.
Study Protocol
Within Michigan, each participating hospital had a local principal investigator. The local principal investigator provided the clinical coordinating center with a list of names and contact information for all emergency physicians in practice at the site and their relevant contact information at 2 time points: prior to any educational intervention within Michigan, and again 18 months later after all interventions had occurred. This contact information was used to solicit participation in the INSTINCT trial survey. In addition, the local principal investigator annually provided information regarding the hospital ED volume, teaching status, and other institutional level variables. Each physician identified was assigned a unique identifier by the data management center. Physicians who migrated between sites were accounted for in this process.
Measurements
The emergency physicians present for the baseline survey were categorized based on their location at 18 months. The following categories were used: “stayed at hospital,” “left all Michigan hospitals (departure),” or “transferred to a different Michigan hospital.” Obversely, physicians present within the hospitals at 18 months were categorized as follows: present at the same hospital as at first survey, new (not previously working at the Michigan hospital), or transferred from a different Michigan hospital. Age, gender, years in practice, and other physician level factors were self reported by the survey respondents.
Statistical Analysis
Descriptive statistics regarding hospital and survey respondent characteristics were calculated as means or proportions as appropriate, and absolute counts and proportions of each type of physician disposition over the course of the study were obtained. The medians and interquartile ranges for the proportions of each type of event (physician loss, physician addition, and overall physician change) were calculated at the hospital level.
We constructed several models to investigate the relationships between physician/hospital characteristics and turnover. Since we expected physicians within hospitals to be more alike than physicians across hospitals (clustering or within hospital correlation), we used methods which accounted for these different types of variability. In general, the uncertainty (or standard error) for parameter estimation in a model should increase in these situations.9Logistic regression models were used to explore the following relationships:
Model 1: The outcome was physician departure and the model covariates were age, gender, hospital teaching status, hospital treatment/control allocation within INSTINCT, and the total number of emergency physicians practicing at that hospital, again with adjustment for within hospital correlation.
We used Poisson regression to examine factors associated with changes in overall number of physicians within each ED.
Model 2: The outcome variable was the total number of physicians at the 18-month survey and the offset (denominator) was the number of physicians at baseline; therefore, the modeled outcome can be considered the proportion of original physicians who were still practicing at 18 months. We included the following hospital level covariates: mean age, proportion female, proportion responding to survey, teaching status, and treatment/control allocation within INSTINCT. Since this model was at the hospital level, we adjusted for within pair correlation.
Model 3: We used logistic regression to investigate the association between treatment/control allocations within INSTINCT and the odds of a physician returning at 18 months from baseline with a weight variable proportional to the number of physicians in each hospital at 18 months.
Statistical analyses were performed using SAS version 9.2 (SAS Corporation, Cary, North Carolina).
RESULTS
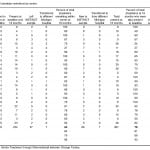
The hospital characteristics and demographic characteristics of physicians responding to the surveys are given in Table 1. While some internal characteristics of these hospitals changed during the course of the study, there was no addition or removal of hospitals from the trial throughout its course.
Table 1. Hospital and physician characteristics at baseline and 18 months.
At baseline, 278 emergency physicians were identified at the 24 Michigan hospitals, of which 199 (72%) returned the baseline survey. At 18 months, 307 physicians were identified within the INSTINCT sample and 344 surveys were sent (included physicians present at baseline who left), and 255 (74%) responded. Complete information regarding the population of physicians working at all sites at both time points was captured from the INSTINCT trial site principal investigators.
At 18 months, 37 (15.8%) had left their baseline hospital and 66 (26.3%) new EPs were working. Seven EPs switched hospitals within the sample. The total number of EPs at 18 months was 307, a 10.8% overall increase. Among the 24 hospitals, 6 had no EP departures and 5 had no new arrivals. The median proportion of EP workforce departing by hospital was 16% (interquartile range [IQR] =3.8%–25%; range =0%–73%), and the median proportion added was 21% (IQR =7%–41%; range = 0%–120%).
The disposition of physicians by hospital is given in Table 2, along with the proportion of physicians remaining at 18 months (accounting for physician loss) and the proportion of physicians at 18 months who were present at baseline (accounting for proportion of physicians at the later time point who likely had opportunity to receive intervention but may have moved to a different hospital within the trial). Six of the 24 hospitals (25%) experienced no physician loss. At 18 months, 5 hospitals (20.8%) were staffed entirely by physicians who were present at baseline, although 4 of these hospitals (16.6%) reported a lower total number of physicians.
Table 2. Disposition of physician workforce by center.
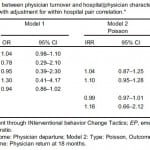
The results of the models are presented in Table 3. None of the evaluated predictor variables in the models achieved statistical significance. In assessing whether hospital or physician level variables are predictive of the propensity for physicians to move, we used methods that allowed for the possibility of intraclass (intrahospital) correlation (ICC), a measure that estimates how alike members within a cluster (ED) behave with respect to an outcome (leaving their position). There was no evidence of such correlation, and an analysis based on independence gives essentially equivalent results. Therefore, one could ignore the number of hospitals (clusters) when trying to estimate how much emergency physician turnover one could expect when planning future studies (ie, reasonable to assume ICC = 0).
Table 3. Measurements of association between physician turnover and hospital/physician characteristics. Model 1 is with adjustment for within hospital correlation. Model 2 is with adjustment for within hospital pair correlation.
DISCUSSION
In this investigation, we found that changes in emergency physician workforce were common. The overall incidence of physician departure was higher than we anticipated when initially planning the INSTINCT trial. We did not find any specific factors that were strongly predictive of physician turnover at either the hospital or provider levels. We observed substantial variability between sites, as several sites had no turnover and some sites had near complete turnover. A major strength of our work is that our methodology allowed us to have migration information even on those who did not respond to our survey via the site principal investigators.
This work has important implications for several groups, including emergency department directors, researchers, and emergency physicians in practice. While it is likely that many groups providing staffing to emergency departments have data on the workforce changes within their sites, we believe this is the first report of specific provider level changes within a geographic sampling of emergency departments. In addition, it is likely that private emergency physician groups or contract organizations consider this type of information to be proprietary, and perhaps as a consequence it has not been disseminated in the peer-reviewed literature. The importance of this work to researchers planning cluster-randomized trials directed at emergency physicians in practice is clear. It is plausible that a large degree of turnover within a site would attenuate the effectiveness of intervention with the actual intended audience for the intervention becoming a moving target. This could occur either from the loss of many physicians or the addition of a large number of physicians due to expansion. From the perspective of the individual emergency physician in practice, this work provides a description of the amount of turnover that may be expected within a community emergency department. When considering employment at a site, one could use our report as an estimate of a baseline expected rate of turnover.
Our findings raise additional questions that will be useful areas of future research. We have hypothesized that increased physician turnover may adversely affect the benefit seen from targeted behavior change interventions. In this study, we have quantified the degree of physician turnover within our sites. Upon the primary analysis of the main INSTINCT outcomes (the improvements in the proportion of patients who were appropriately receiving intravenous tPA for stroke and the degree of knowledge change among ED physicians regarding thrombolytic use), we plan to measure the association between turnover and the efficacy of the main INSTINCT trial educational intervention. While it is intuitive that an association will be found between these factors of turnover and effectiveness of the intervention, it is also possible that the intervention may be resistant to turnover and may exert its main effect at the hospital level. Additional research with larger cohorts of emergency physicians with a more diverse geographic and demographic distribution that includes smaller hospitals and academic health centers may provide additional insight into emergency physician migration patterns.
LIMITATIONS
This investigation has several important limitations. The sampling frame for INSTINCT was at the hospital level. Only community hospitals with more than 100 stroke diagnoses were included. In addition, hospitals with formal comprehensive stroke programs were excluded. On the other hand, this investigation does provide a sample of hospitals that might be expected to be reflective of many community hospitals throughout the United States. It should be noted, however that all the included hospitals were within the lower peninsula of Michigan, and our findings in this investigation may not be generalizable to other settings. The state of Michigan has experienced economic challenges during the period in which this study was performed. This may lead to additional turnover due to economic stresses and migration to other states, although it may also lead to fewer turnovers due to difficulty finding alternative employment opportunities. Physician turnover rates were determined as a secondary analysis within a clinical trial with broader specific aims. We did not collect data on the longevity of physicians within their positions or the reasons that physicians ultimately left their positions. Finally, we did not observe enough physician departure events to draw any strong inferences relating hospital and physician level factors and their influence on turnover.
CONCLUSIONS
In summary, the incidence of emergency physician turnover is relatively common in our hospital sample. Further research is needed to better describe emergency physician turnover in more varied geographic settings. This has a significant impact on decisions made by emergency department directors, researchers, and individual level EPs. Planners of research efforts that involve targeted educational interventions upon emergency physicians to test and improve their clinical practice should take workforce changes into account in the modeling of their investigations.
Footnotes
Supervising Section Editor: Jeffrey Druck, MD
Submission history: Submitted May 16, 2011; Revision received August 8, 2011; Accepted August 22, 2011
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.8.6798
Address for Correspondence: William J. Meurer, MD, MS, University of Michigan, Department of Emergency Medicine, Taubman Center B1354 SPC 5303, 1500 E Medical Center Dr, Ann Arbor, MI 48109-5303
E-mail: wmeurer@umich.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed the following information: This work was funded by the National Institutes of Health R01-NS050372. The first author also received salary support from the Emergency Medicine Foundation. The INSTINCT trial is registered with Clinicaltrials.gov (identifier NCT00349479).
REFERENCES
1. Turck JE. Caring for the Country: Physician Retention at Cortland Regional Medical Center [thesis] Cortland, NY: State University of New York; 2009.
2. Pathman DE, Williams ES, Konrad TR. Rural physician satisfaction: its sources and relationship to retention. J Rural Health. 1996;12:366–377. [PubMed]
3. Misra-Hebert AD, Kay R, Stoller JK. A review of physician turnover: rates, causes, and consequences. Am J Med Qual. 2004;19:56–66. [PubMed]
4. Demmy TL, Kivlahan C, Stone TT, et al. Physicians’ perceptions of institutional and leadership factors influencing their job satisfaction at one academic medical center. Acad Med. 2002;77:1235–1240. [PubMed]
5. Buchbinder S, Wilson M, Melick C. Estimates of costs of primary care physician turnover. Am J Manag Care. 1999;5:1431–1438. [PubMed]
6. Reinhart MA, Munger BS, Rund DA. American Board of Emergency Medicine Longitudinal Study of Emergency Physicians. Ann Emerg Med. 1999;33:22–32. [PubMed]
7. Hall KN, Wakeman MA. Residency-trained emergency physicians: their demographics, practice evolution, and attrition from emergency medicine. J Emerg Med. 1999;17:7–15.[PubMed]
8. von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (strobe) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. [PubMed]
9. Wears RL. Advanced statistics: statistical methods for analyzing cluster and cluster-randomized data. Acad Emerg Med. 2002;9:330–341. [PubMed]