| Author | Affiliation |
|---|---|
| Gillian Schmitz, MD | University of California at San Diego, Department of Emergency Medicine, San Diego, California |
| Tress Goodwin, MD | Washington Hospital Center, Department of Emergency Medicine, Washington, DC |
| Adam Singer, MD | Stony Brook University and Medical Center, Department of Emergency Medicine, Stony Brook, New York |
| Chad S. Kessler, MD, MHPE | Jesse Brown VA Medical Center, Department of Emergency Medicine, Chicago, Illinois |
| David Bruner, MD | Naval Medical Center, Department of Emergency Medicine, Portsmouth, Virginia |
| Hollynn Larrabee, MD | West Virginia University, Department of Emergency Medicine, Morgantown, West Virginia |
| Larissa May, MD | George Washington University, Department of Emergency Medicine, Washington, DC |
| Samuel D. Luber, MD | University of Texas Health Science Center at Houston, Department of Emergency Medicine, Houston, Texas |
| Justin Williams, MD | University of Texas Health Science Center at San Antonio, Department of Emergency Medicine, San Antonio, Texas |
| Rahul Bhat, MD | Washington Hospital Center, Department of Emergency Medicine, Washington, DC |
ABSTRACT
Introduction:
Cutaneous abscesses are commonly treated in the emergency department (ED). Although incision and drainage (I&D) remains the standard treatment, there is little high-quality evidence to support additional interventions such as pain control, type of incision, and use of irrigation, wound cultures, and packing. Although guidelines exist to support clinician management of abscesses, they do not clearly specify these additional interventions. This study sought to describe the ED treatments administered to adults with uncomplicated superficial cutaneous abscesses, defined as purulent lesions requiring incision and drainage that could be managed in an ED or outpatient setting.
Methods:
Four hundred and seventy-four surveys were distributed to 15 EDs across the United States. Participants were queried about their level of training and practice environment as well as specific questions regarding their management of cutaneous abscesses in the ED.
Results:
In total, 350 providers responded to the survey (74%). One hundred eighty-nine respondents (54%) were attending physicians, 135 (39%) were residents, and 26 (7%) were midlevel providers. Most providers (76%) used narcotics for pain management, 71% used local anesthetic over the roof of the abscess, and 60% used local anesthetic in a field block for pain control. More than 48% of responders routinely used irrigation after (I&D). Eighty-five percent of responders used a linear incision to drain the abscess and 91% used packing in the wound cavity. Thirty-two percent routinely sent wound cultures and 17% of providers routinely prescribed antibiotics. Most providers (73%) only prescribed antibiotics if certain historical factors or physical findings were present on examination. Antibiotic treatment, if used, favored a combination of 2 or more drugs to cover both Streptococcus and methicillin-resistant Staphylococcus aureus (47%). Follow-up visits were most frequently recommended at 48 hours unless wound was concerning and required closer evaluation.
Conclusion:
Variability exists in the treatment strategies for abscess care. Most providers used narcotic analgesics in addition to local anesthetic, linear incisions, and packing. Most providers did not irrigate, order wound cultures, or routinely prescribe oral antibiotics unless specific risk factors or physical signs were present. Limited evidence is available at this time to guide these treatment strategies.
INTRODUCTION
Skin and soft tissue infections, particularly those caused by community-acquired methicillin resistant Staphylococcus aureus (MRSA) are common presentations to the emergency department (ED).1–3 Multiple consensus documents and textbooks offer procedure guidelines for management of simple cutaneous abscesses, yet there is little evidence to support these practices (Table 1).4–10 The only consensus on treatment is incision and drainage (I&D), but specific recommendations regarding incision type, irrigation, packing, pain management, wound cultures, and timing for follow-up visits vary widely. One study demonstrated variation by provider type and experience, suggesting practice patterns for I&D technique are not standardized, even within a single institution.11 Our objective was to determine variability of practice patterns nationwide for treatment of uncomplicated superficial abscesses.
Table 1. Current procedural guidelines for incision and drainage of simple cutaneous abscesses.
METHODS
Study Design and Population
This was a cross-sectional survey of ED providers, including resident physicians, attending physicians, and midlevel providers (physician assistants and nurse practitioners). Surveys were distributed to a convenience sample of 474 ED providers from 15 EDs across the United States. Study sites were selected from home institutions of a network of researchers across the country who had previously studied or published articles on abscess care. Surveys were distributed to all full-time physicians and residents rotating in the ED during the study period. The 9 sites, comprising 15 EDs, were chosen from academic centers, community teaching departments, and military EDs from different parts of the country, including urban and suburban locations, to optimize generalizability. Surveys were distributed in either paper or electronic format to all ED providers working in their department at each site during the study period. This study received an exempt status from the local institutional review committee.
Survey Content and Administration
The survey was designed to examine practice patterns of ED providers for the management of uncomplicated superficial cutaneous abscesses. The questionnaire, developed by members of the research team, was based upon a literature review of current recommendations for abscess management and was reviewed and revised by a research committee at Washington Hospital Center. The final survey consisted of 15 questions in total to determine provider demographics and the 4 categories of management strategies: pain management, irrigation, I&D/packing, and culture/antibiotic use. Questions were close-ended and consisted of categorical and yes/no responses. For some questions, participants could select more than 1 answer, if appropriate. The survey used an encrypted Internet-based survey tool (SurveyMonkey;http://www.surveymonkey.com) to collect and analyze responses. Each survey site had a unique identifier to determine the site response rate.
Between October 1 to 31, 2010, surveys were distributed to each provider working in the ED of participating institutions. Participants had the option of either answering the survey online or completing a hard copy, but were limited to 1 submission per responder. To preserve anonymity while preventing multiple entries by 1 individual and allow tracking by each study site, we enabled a tool on SurveyMonkey that assigned tracking codes to participants at each site. Results from paper surveys were entered online by a study investigator. Participation was voluntary and a small incentive in the form of a drawing for a small prize was offered. All responses were anonymous, though participants were asked to provide an e-mail address if they wished to participate in the prize drawing.
We collected the background demographics of the survey participants, including provider type (midlevel provider, resident, fellow, or attending physician) and type of practice setting (academic, community, military, rural, urban). We measured use of specific interventions for abscess management: pain control, irrigation, packing, wound cultures, antibiotic use, and follow-up instructions.
Data Analysis
Responses were analyzed by using standardized tabulations. Descriptive statistics were used to describe demographic variables and percentages were used to summarize categorical data. Comparison of responses by provider type was completed by using the chi-square test; Fisher exact test was used when appropriate. Results were calculated on the basis of the number of respondents to a particular question.
To identify the association between provider type and management strategies, unadjusted and adjusted odds ratios and 95% confidence intervals were calculated by using logistic regression with StatXact, version 9.0.0 (March 17, 2010; Cytel Corporation, Cambridge, Massachusetts).
RESULTS
Demographics
Of the 474 eligible participants, 350 providers (74%) responded to the survey (Appendix; online only). Of the respondents, 189 (54%) were attending physicians, 135 (39%) were residents, and 26 (7%) were midlevel providers. Respondents were asked about the type of environment in which they practiced and were allowed to indicate more than 1 if they worked at multiple different hospitals. Two hundred and seventy-three (78%) worked at a university-affiliated hospital; 66 (19%), at a community hospital; 65 (19%), at a military hospital; 64 (18%), only in an urban environment; and 3 (<1%), only in a rural environment.
Pain Management
Overall, most respondents (76%) provided narcotics in addition to local anesthesia. There was no significant difference between midlevel providers and physicians providing oral or intravenous analgesia before incision and drainage (Table 2). Seventy-one percent of all responders administered local anesthetic over the roof of the abscess and 60% used a field block, with no significant difference between provider type.
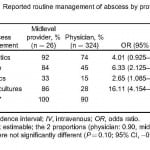
Table 2. Reported routine management of abscess by provider type.
Irrigation
As a group, ED providers were about equally likely to use irrigation versus no irrigation after incision and drainage: 48% versus 52%, respectively. Midlevel providers were significantly more likely to use irrigation than residents and attending physicians: 84% versus 45%, respectively, (Table 2). Of those who reported using irrigation, almost all (94%) used saline, 4% used tap water, and 1% used betadine. Additionally, of the providers using irrigation, most irrigated under high pressure (66%), with either a splash guard or angiocatheter, and 34% rinsed out the wound cavity without high pressure. There was no clear consensus on the amount of irrigation to use. Forty-eight percent of irrigators used 50 cc or less, or enough to rinse out the wound until only irrigation fluid returned. Only 36% used 100 cc per centimeter of abscess size and 16% indicated there was no specific volume they routinely used.
Incision and Drainage/Packing/Follow-Up Instructions
The most common type of incision was linear among attending physicians (87%), residents (88%), and midlevel providers (56%). Elliptical incisions were less common for attending physicians (7%), residents (7%), and midlevel providers (36%). Cruciate incisions were rarely reported (6%). No providers indicated that they used needle aspiration as treatment of abscesses.
Most providers used packing in the wound cavity (91%) and this was consistent for attending physicians (94%), residents (86%), and midlevel providers (100%). Seventy-five percent of all providers filled the wound with packing, while 24% used only a small wick to keep the cavity open. Patients were instructed to return in 24 hours by 15% of providers, at 48 hours by 32% of providers, and at “48 hours unless wound is concerning and needs closer evaluation” by 47% of providers.
Culture/Antibiotic Use
Most providers (68%) do not routinely culture the wound cavity. There were significantly more midlevel providers who routinely ordered wound cultures than attending physicians and residents: 86% versus 28%, respectively, (Table 2), The routine use of antibiotics after every incision and drainage in healthy patients with uncomplicated abscesses was rare (17%). Antibiotics were reserved for use if the patient was diabetic or immunocompromised (58%), had a history of MRSA (24%), or surrounding cellulitis (74%).
If antibiotics were used, 33% of all providers used trimethoprim-sulfamethaxole alone, 8% used cephalexin alone, 8% used clindamycin alone, and 47% used a combination of 2 or more drugs for MRSA and Streptococcus coverage. Midlevel providers were more likely to use a combination of 2 different antibiotics. Virtually all respondents (99%) allowed wounds to heal by secondary intention rather than primary closure after incision and drainage (drainage followed by immediate suture repair).
DISCUSSION
Most texts and guidelines suggest incision and drainage as the treatment for uncomplicated superficial cutaneous abscesses; however, there is no standard definition of the procedure and little evidence to support the additional steps involved. This survey is unique in that it evaluated previously unaddressed issues including use of pain control, irrigation, wound cultures, and packing. Significant variation exists with regard to the management of cutaneous abscesses. Our study attempted to describe variability in clinical practice to establish a basic understanding of the current management of emergency providers nationwide and compare management strategies to existing guidelines.
Incision and drainage has been considered to be one of the more painful procedures performed in the ED, second only to nasogastric tube insertion.12 Providing adequate pain management is a challenge, as the lower pH of the infected tissue reduces the effectiveness of local anesthetic. Our study demonstrated that most providers treat pain associated with I&D with local lidocaine and often with additional oral or intravenous narcotics. Although most references recommend at least local anesthesia, there is some discrepancy regarding the need for additional systemic pain management.4–10 The difference in abscess size, location, and patient’s pain threshold may account for this variability in practice. No randomized controlled trials to date have compared the effectiveness in pain reduction of these various techniques, and additional research in this area will likely yield improved patient care and satisfaction.
Irrigation, though recommended by most textbooks and cited guidelines,4–10 is routinely done by only about half of respondents. There is little consensus on the type and volume of fluid that should be used to irrigate the cavity. Although 1 single-site study found that physician assistants were less likely to use irrigation than attending physicians and residents, our study demonstrated the opposite.11 In fact, less than half of the physicians surveyed routinely used irrigation after I&D, compared with 84% of midlevel providers. This is possibly because of the additional time required to irrigate, the undesired effect of purulent discharge splashing under high pressure, and lack of evidence to support its routine use. No randomized controlled trials have investigated the theoretical benefit of reducing the bacterial load in abscesses through copious irrigation.
Most texts and guidelines recommend a wide incision and often cite insufficient drainage as the cause of treatment failure. Continuing the incision over the entire length of the abscess theoretically allows for adequate room to probe loculations, facilitates subsequent packing changes, and allows for adequate drainage. However, a recent study in a pediatric population calls this standard practice into question. In a study with 115 patients, using 2 small incisions (4–5 mm) far apart on the abscess and a loop drain tied on top of the skin, the success rate was 94.5%, as measured by need for additional intervention.13 Large incisions produce large scars, and cosmetic outcome may be an important factor for patient satisfaction. Although it has not been studied in ED patients, primary closure has been used in the operating room under general anesthesia and has been shown to reduce cost, reduce time for wound healing, and improve cosmetic appearance.14–16 Although no studies have compared outcome with incision type, needle aspiration alone is commonly associated with higher rates of treatment failure.17 Our study demonstrates that most providers use linear incisions and very few perform needle aspirations unless it is used diagnostically to determine if a lesion contains purulent discharge. Primary closure of abscess cavities was rarely reported.
The use of gentle packing is generally recommended by current guidelines to prevent premature wound closure and allow continuous drainage after I&D.9 However, the theory behind wound packing is based on consensus guidelines rather than evidence-based data and is performed at the discretion of the provider.18 Furthermore, a small pilot study challenged this mantra by demonstrating that packing may cause increased pain and is not associated with improved outcome.19 Our study demonstrated that almost all providers routinely used packing and frequent wound repacking visits despite the lack of supporting evidence and increased pain and inconvenience to the patient. Further randomized controlled trials are needed to determine the effects of packing on clinical outcomes.
Although the 2011 Infectious Diseases Society of America guidelines recommend wound cultures in certain circumstances, the routine use of wound cultures in uncomplicated abscesses in otherwise healthy individuals is often unnecessary in the ED.20 While the prevalence of MRSA is variable geographically, it has become the most common cause of skin and soft tissue infections and is often treated empirically. Our study reflects the fact that although most physicians do not routinely order wound cultures, many midlevel providers still attempt to identify an organism. Wound cultures are costly and results are neither available immediately nor likely to change management. Although cultures may be needed in some instances, it is unclear why this was more routine practice among midlevel providers.10
Perhaps the most surprising result of our study is that only 17% of providers indicated that they routinely give oral antibiotics after I&D. While this practice follows guidelines (Clinical Infectious Disease, Center of Disease Control), textbooks,4–10 and recommendations from recent studies,21,22it is significantly less than the antibiotic use of 53% to 80% reported in previous studies.1,11 This survey suggests that physicians are perhaps now reserving the routine use of antibiotics for specific cases. Most providers stated that they would select antibiotics with MRSA coverage, but would not routinely prescribe them unless there were certain risk factors such as a history of MRSA, immunodeficiency, or surrounding cellulitis. The variability in the number and types of antibiotic coverage may be influenced by local susceptibilities and desire to cover both MRSA and other bacteria.
As we continue to improve our practice as emergency care providers and move toward more evidence-based care, many of these practices will likely be challenged, and perhaps what has been “standard” will be replaced by less invasive, less painful, and more effective treatment of even our most routine patient presentations.
LIMITATIONS
The study was limited by its survey design, predominantly closed-answer format and sampling strategy. Some of the survey questions were not stratified by patient or wound factors and it is possible that provider management may vary on the basis of specific variables (ie, abscess location) that were not queried. The survey relies on self-reported practices and thus, the accuracy of actual practice patterns cannot be assured. Attempts were made to include various practice settings nationwide, but the sampling technique introduces some selection bias. While the response rate of 74% is higher than that of most survey studies,23,24 the 26% who did not respond may also represent a source of selection bias.
CONCLUSION
Current guidelines recommend incision and drainage without defining a standard treatment method. This study shows a large variation of practice patterns for the management of uncomplicated superficial abscesses in the ED. Despite this variability in clinical practice, certain trends were identified. Most providers used oral or intravenous analgesia in addition to local anesthetic, linear incisions, and packing. Most physicians did not use irrigation, order wound cultures, or routinely prescribe oral antibiotics unless specific risk factors or physical signs were present. Further research into ideal management of uncomplicated superficial abscesses is needed to create evidence-based guidelines and optimize treatment in the ED.
Appendix.
Footnotes
We would like to acknowledge Dr Joel Michalek, Vice Chair for the Department of Epidemiology and Biostatistics at University of Texas, San Antonio Health Sciences Center, for his assistance with statistical analysis.
Supervising Section Editor: Robert W. Derlet, MD
Submission history: Submitted July 18, 2011; Revision received September 24, 2011; Accepted October 24, 2011
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.9.6856
Address for Correspondence: Gillian Schmitz, MD, University of California at San Diego, Department of Emergency Medicine, 200 W Arbor Dr, San Diego, CA 92103
E-mail: GillianMD@gmail.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355:666–674. [PubMed]
2. Pallin DJ, Egan DJ, Pelletier AJ, et al. Increased US emergency department visits for skin and soft tissue infections, and changes in antibiotic choices during the emergence of community-acquired methicillin-resistant Staphylococcus aureus. Ann Emerg Med. 2008;51:291–298. [PubMed]
3. Woolard R, Degutis LC, Mello M, et al. Public health in the emergency department: surveillance, screening, and intervention—funding and sustainability. Acad Emerg Med. 2009;16:1138–1142.[PubMed]
4. Butler K. Incision and drainage. In: Roberts J, Hedges J, editors. Clinical Procedures in Emergency Medicine. 5th ed. Philadelphia, PA: Elsevier, Inc; 2010. pp. 657–691.
5. Meislin H, Guisto J. Soft tissue infections, simple cutaneous abscesses. In: Marks J, Hockberger R, Walls R, editors. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 7th ed. Philadelphia, PA: Mosby Elsevier, Inc; 2010. pp. 1836–1847.
6. Folstad S. Soft tissue infections. In: Tintinalli JE, Ruiz E, Krome RL, editors. Emergency Medicine: A Comprehensive Study Guide. 6th ed. New York, NY: McGraw-Hill; 2004. pp. 985–986.
7. Beard JM, Osborn J. Common office procedures. In: Rakel R, editor. Textbook of Family Medicine.8th ed. Philadelphia, PA: Elsevier, Inc; 2011. p. 564.
8. Kronfol R, Downey K. Technique of incision and drainage for skin abscess. UpToDate. Web site. Available at: http://www.uptodate.com/contents/technique-of-incision-and-drainage-for-skin-abscess. Accessed December 30, 2010.
9. Hammond SP, Baden LR. Management of skin and soft-tissue infection—polling results. New Engl J Med. 2008;359:e20. [PubMed]
10. Liu C, Bayer A, Cosgrove S, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52:e18–55. [PubMed]
11. May L, Harter K, Yadav K, et al. Practice patterns and management strategies for purulent skin and soft-tissue infections in an urban academic ED [published online ahead of print January 27, 2011] Am J Emerg Med. doi: 10.1016/j.ajem.2010.11.033.. [Cross Ref]
12. Singer AJ, Richman PB, Kowalkska A. Comparison of patient and practitioner assessments of pain from commonly performed emergency department procedures. Ann Emerg Med. 1999;33:652–658.[PubMed]
13. Freedman S, Sivabalasundaram V, Bohn V, et al. The treatment of pediatric gastroenteritis: A comparative analysis of pediatric emergency physicians’ practice patterns. Acad Emerg Med.2011;18:38–45. [PubMed]
14. Abraham N, Doudle M, Carson P. Open versus closed surgical treatment of abscesses: a controlled clinical trial. Aust N Z J Surg. 1997;67:173–176. [PubMed]
15. Stewart MP, Laing MR, Krukowski ZH. Treatment of acute abscesses by incision, curettage and primary suture without antibiotics: a controlled clinical trial. Br J Surg. 1985;72:66–67. [PubMed]
16. Edino ST, Ihezue CH, Obekpaa PO. Outcome of primary closure of incised acute soft-tissue abscesses. Niger Postgrad Med J. 2001;8:32–36. [PubMed]
17. Gaspari RJ, Resop D, Mendoza M, et al. A randomized controlled trial of incision and drainage versus ultrasonographically guided needle aspiration for skin abscesses and the effect of methicillin-resistant Staphylococcus aureus. Ann Emerg Med. 2011;57:483–491. [PubMed]
18. Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005;41:1373–1406. [PubMed]
19. Gerald F, Dominici P, Giraldo P, et al. Routine packing of simple cutaneous abscesses is painful and probably unnecessary. Acad Emerg Med. 2008;16:470–473.
20. Schmitz G. How do you treat an abscess in the era of increased community associated methicillin-resistant Staphylococcus aureus (MRSA)? J Emerg Med. 2011;41:276–281. [PubMed]
21. Schmitz GR, Bruner D, Pitotti R, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus infection. Ann Emerg Med. 2010;56:283–287.[PubMed]
22. Duong MD, Markwell S, Peter J, et al. Randomized, controlled trial of antibiotics in the management of community-acquired skin abscesses in the pediatric patient. Ann Emerg Med.2010;55:401–407. [PubMed]
23. Asch D, Jedrziewski K, Christakis N. Response rates to surveys published in medical journals. J Clin Epidemiol. 1997;10:1229–1236.
24. Cummings S, Savitz L, Konrad T. Reported response rates to mailed physician questionnaires.Health Serv Res. 2001;35:1347–1355. [PMC free article] [PubMed]