| Author | Affiliation |
|---|---|
| Karis L. Tekwani, MD | Advocate Christ Medical Center, Department of Emergency Medicine, Oak Lawn, Illinois |
| Yaniv Kerem, MD | University of Chicago Medical Center, Section of Emergency Medicine, Chicago, Illinois |
| Chintan D. Mistry, MD | Advocate Christ Medical Center, Department of Emergency Medicine, Oak Lawn, Illinois |
| Brian M. Sayger, DO | Advocate Christ Medical Center, Department of Emergency Medicine, Oak Lawn, Illinois |
| Erik B. Kulstad, MD, MS | Advocate Christ Medical Center, Department of Emergency Medicine, Oak Lawn, Illinois |
ABSTRACT
Introduction:
Emergency department (ED) crowding has been shown to negatively impact patient outcomes. Few studies have addressed the effect of ED crowding on patient satisfaction. Our objective was to evaluate the impact of ED crowding on patient satisfaction in patients discharged from the ED.
Methods:
We measured patient satisfaction using Press-Ganey surveys returned by patients that visited our ED between August 1, 2007 and March 31, 2008. We recorded all mean satisfaction scores and obtained mean ED occupancy rate, mean emergency department work index (EDWIN) score and hospital diversion status over each 8-hour shift from data archived in our electronic tracking board. Univariate and multivariate logistic regression analysis was calculated to determine the effect of ED crowding and hospital diversion status on the odds of achieving a mean satisfaction score ≥ 85, which was the patient satisfaction goal set forth by our ED administration.
Results:
A total of 1591 surveys were returned over the study period. Mean satisfaction score was 77.6 (standard deviation [SD] ±16) and mean occupancy rate was 1.23 (SD ± 0.31). The likelihood of failure to meet patient satisfaction goals was associated with an increase in average ED occupancy rate (odds ratio [OR] 0.32, 95% confidence interval [CI] 0.17 to 0.59, P < 0.001) and an increase in EDWIN score (OR 0.05, 95% CI 0.004 to 0.55, P = 0.015). Hospital diversion resulted in lower mean satisfaction scores, but this was not statistically significant (OR 0.62, 95% CI 0.36 to 1.05). In multivariable analysis controlling for hospital diversion status and time of shift, ED occupancy rate remained a significant predictor of failure to meet patient satisfaction goals (OR 0.34, 95% CI 0.18 to 0.66, P = 0.001).
Conclusion:
Increased crowding, as measured by ED occupancy rate and EDWIN score, was significantly associated with reduced patient satisfaction. Although causative attribution was limited, our study suggested yet another negative impact resulting from ED crowding.
INTRODUCTION
Emergency department (ED) crowding is a major issue facing many of the nation’s emergency departments.1–5 The etiology of crowding is believed to be multifactorial, with the following key elements contributing to its cause: a decrease in hospital capacity, an increase in closures of a significant number of EDs, an increase in ED patient volumes, a shortage in nursing staff, an increase in the complexity of patient management and the inability to transfer patients from the ED to inpatient units.4 ED crowding has been associated with adverse medical outcomes and substandard patient care, including delays in door-to-needle time for patients with acute myocardial infarction, increased death after admission and poor performance on pneumonia quality of care measures.6–11A recent meta-analysis found crowding to be associated with an increase in transport delays, ambulance diversion and patients leaving the ED without being seen.12 A recent study focusing on patients who were admitted to the ED suggested that poor ED service, as indicated by ED hallway use and prolonged boarding time, was not only associated with a decreased satisfaction in the ED, but also predicted a lower satisfaction with the entire hospitalization.13 Patient satisfaction is an important issue for EDs and has been recognized as a measure of quality of healthcare.14
Determining the correlation between ED crowding and patient satisfaction could have substantial impact, as patient satisfaction can play a key role in physician evaluations, compensation, medico-legal action and improvement in patient care. No studies, to our knowledge, have evaluated the effect of ED crowding on patient satisfaction in patients discharged directly from the ED.
The purpose of our study was to investigate the association between patient satisfaction, as measured using Press-Ganey surveys (www.pressganey.com), and ED crowding, as measured by the ED occupancy rate, emergency department work index (EDWIN) score and hospital diversion status. We hypothesized that there would be an inverse relationship between patient satisfaction and ED crowding in patients discharged directly from the ED.
MATERIALS AND METHODS
Study Design and Setting
We conducted a retrospective, cohort study of all patients who were discharged from the ED and completed Press-Ganey patient satisfaction surveys between August 1, 2007 and March 31, 2008. The study was performed in a large, tertiary care, suburban, teaching hospital ED. Our ED has an annual census of greater than 85,000 patients, with an average of 230 patients seen in the ED on a daily basis. This study was approved by our local institutional review committee.
Methods of Measurement
Crowding was measured using the following 3 metrics: ED occupancy rate, modified EDWIN score and hospital diversion status. The ED occupancy rate was defined as the total number of patients in the ED divided by the total number of ED licensed beds.15 We determined the EDWIN score by calculating patient number and acuity, number of attending physicians on duty and total bed availability.11, 16, 17 The higher the EDWIN score the more crowded the ED. We measured patient satisfaction using the Press-Ganey survey, a commonly used measure of patient satisfaction in the ED.
Press-Ganey surveys were distributed, at random, to both adult and pediatric patients discharged from the ED over an 8-month period. Press-Ganey selects patients randomly to distribute surveys, using a read-skip methodology, as follows: The system reads the first patient record, then skips the next 7 records, then reads the next record, then skips the next 7 records. This method is continued until the maximum number of patients is reached. A maximum of 2000 patients were provided with a survey each month, which translated to approximately 40% of the patients discharged from the ED in a given month. The surveys were collected by Press-Ganey, with an average response rate of 10–12%.
Patients were instructed to complete the survey by scoring questions within the following categories: arrival, tests, nurses, doctors, family or friends, personal issues, overall assessment and personal/insurance information. Each question was scored on a 5-point Likert scale, with a score of 1 corresponding to “very poor” and a score of 5 corresponding to “very good.” Each score on the Likert scale was then converted to a mean satisfaction score (1=0, 2=25, 3= 50, 4=75, 5=100). Each patient was also asked to designate his or her time of arrival, which corresponded to one of 3 8-hour shifts: 7:00am–3:00pm, 3:00pm–11:00pm and 11:00pm–7:00am.
We recorded all mean satisfaction scores and obtained mean ED occupancy rate, mean EDWIN score and hospital diversion status over each 8-hour shift. These data were archived in our electronic tracking board. We considered hospital diversion status positive if our ED was on diversion at any point during the 8-hour shift. Our hospital went on diversion when there was no available monitored bed to take a new patient admitted from the ED.
We calculated the original EDWIN score using the following formula: Σniti/Na(BT-BA), where ni was the number of patients in the ED in triage category i, ti was the triage category, Na was the number of attending physicians on duty, BT was the number of treatment bays and BA was the number of admitted patients in the ED. The triage category (ti) was defined by the Emergency Severity Index (ESI), a measure commonly used in North America to stratify patients into 5 groups based on their acuity, required resources and timeliness.18 To assign higher numerical values to higher severity patients, the EDWIN score reverses the standard ordinal ranking of triage categories so that ESI-1 patients (highest acuity) are assigned a value of 5, ESI-2 patients a value of 4, ESI-3 patients a value of 3, ESI-4 patients a value of 2 and ESI-5 patients (lowest acuity) a value of 1. In the original derivation of the EDWIN score, the authors found “an active but manageable ED has an EDWIN score less than 1.5, a busy ED has an EDWIN between 1.5 and 2, and a crowded ED has a score greater than 2.” 16
Our ED information system and electronic tracking board (Picis ED PulseCheck, Wakefield, Mass.) automatically calculated and provided a “modified” EDWIN score in real-time. To avoid “divide by zero” computational errors, the EDWIN score available on our electronic tracking board varied from the standard EDWIN score in the following 2 ways: 1) admitted patients were not removed from the variable ni in the numerator (standard calculation of EDWIN score excludes admitted patients from variable ni); and 2) the number of treatment bays, BT, denoted all beds available for patient care in the ED, including hallway beds (standard calculation only includes licensed treatment bays). In our study, BT was 117, rather than the 50 licensed beds for our ED. The result of these modifications was a lowering of the numerical value of our score when compared to the original description of the EDWIN score, but it still varied by a full order of magnitude between lowest and highest value. Given that we used this modified EDWIN score that involved changes to both the numerator and the denominator of the original EDWIN score, there is no proportional correlation to the original EDWIN score; therefore, it is difficult to draw conclusions about the score at which a “busy” and “crowded” ED would occur.
Primary Data Analysis
We calculated Spearman correlation (ρ) to determine the association between ED crowding and patient satisfaction scores (with Spearman correlation coefficients ranging from −1 to 1, with values closest to −1 indicating a strong inverse association and values closest to 1 indicating a strong positive association). We calculated univariate and multivariate logistic regression analysis to determine the effect of ED crowding and hospital diversion status on the odds of achieving a mean satisfaction score ≥ 85, which was the patient satisfaction goal set forth by our ED administration. Model parameters were specified and input as forced predictors into our model. We performed statistical analyses using SPSS version 16.0 (SPSS Inc., Chicago, IL). For all analyses, P ≤ 0.05 denoted statistical significance, with no adjustment for multiple comparisons.
RESULTS
A total of 1591 surveys were returned over the course of our study period, encompassing 497 8-hour shifts. Our analysis revealed a mean patient satisfaction score of 77.6, with a standard deviation of 16.5. The mean occupancy rate was 1.23 (SD ± 0.31), and the mean EDWIN score was 0.30 (SD ± 0.08). Occupancy rate was inversely correlated with patient satisfaction (Spearman’s ρ = −0.16, P < 0.001). The EDWIN score was inversely correlated with patient satisfaction (Spearman’s ρ = −0.11, P= 0.02). We also found a statistically significant decrease in the likelihood of meeting patient satisfaction goals (mean satisfaction score ≥ 85) with an increase in average ED occupancy rate (odds ratio [OR] 0.32, 95% confidence interval [CI] 0.17 to 0.59, P < 0.001). Likewise, we noted a significant decrease in the likelihood of meeting patient satisfaction goals (mean satisfaction score ≥ 85) with an increase in the EDWIN score (OR 0.05, 95% CI 0.004 to 0.55, P = 0.015). Analysis of the effect of hospital diversion on patient satisfaction goals revealed slightly lower mean satisfaction scores when the ED was on diversion, but this difference was not statistically significant (OR 0.62, 95% CI 0.36 to 1.05). In multivariable analysis controlling for hospital diversion status and time of shift, ED occupancy rate remained a significant predictor of failure to meet patient satisfaction goals (OR 0.34, 95% CI 0.18 to 0.66, P = 0.001).
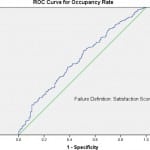
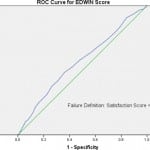
To evaluate the characteristics of the occupancy rate and EDWIN score as instruments predictive of ED satisfaction, we plotted receiver operating characteristic (ROC) curves using the binary outcome of meeting patient satisfaction goals as set by our ED administration (mean satisfaction score ≥ 85). The area under the curve (AUC) for occupancy rate was 0.59 (95% CI 0.54 to 0.65, P ≤ 0.001) as seen in Figure 1. The AUC for the EDWIN score was 0.57 (95% CI 0.52 to 0.62, P = 0.012) as seen in Figure 2. The AUC values obtained were small, which limited our ability to use a single cutoff value to obtain high sensitivity and specificity. That said, an ED occupancy rate < 90% suggested approximately 90% sensitivity for meeting a mean satisfaction score ≥ 85, while and ED occupancy rate > 151% provided approximately 90% specificity for failure to meet a mean satisfaction score ≥ 85.
Figure 2. Receiver operating characterstic (ROC) curve for emergency department work index (EDWIN) score.
DISCUSSION
ED crowding is a phenomenon that continues to burden the healthcare system. The number of patients passing through EDs in the United States continues to increase, along with a decrease in the number of EDs available for their care.4 An increase in patient volume, with a concomitant decrease in available facilities to treat these patients, will further complicate the issue of ED crowding. This issue goes beyond a patient’s contentment with his or her visit to the ED; it has been associated with unfavorable medical outcomes and poor patient care.6–11, 19, 20 ED crowding may also impact hospital revenue and has even been shown to impact physician job satisfaction.21–23 Needless to say, ED crowding is a complex issue affecting many aspects of patient care.
Interestingly, at least 1 recent study did not find an association between ED crowding and adverse outcomes. This study measured time to percutaneous coronary intervention for patients with ST-segment elevation myocardial infarction (STEMI). As suggested in that study, higher acuity conditions, such as STEMI, may result in a diversion of resources away from other lower acuity conditions, which can lead to unfavorable outcomes overall.24
What makes our study different from other studies evaluating patient satisfaction was that we evaluated patients discharged directly from the ED. We used ED crowding metrics to show that the more crowded the ED, the more dissatisfied the patient. Our analysis revealed a statistically significant decrease in patient satisfaction goals with an increase in both occupancy rate and EDWIN score. Although hospital diversion status was correlated with a slight decrease in patient satisfaction goals, this was not clinically significant.
LIMITATIONS
This study was non-randomized and took place at a single institution. Those individuals who returned the Press-Ganey survey may not have been representative of all patients. Furthermore, our response rate was uncertain and likely low, as is common for patient satisfaction surveys. As a result, this study might have been subject to selection bias. The scale of our EDWIN score differed from that described in the original literature, which potentially limited the generalizability of our results. Avoidance of a divide by zero error in the implementation of electronic real-time calculation of the EDWIN score resulted in a larger denominator than would have otherwise existed. As such, our EDWIN score calculation resulted in a lower value than would normally have been calculated. Despite the lower numerical value of our EDWIN score, the range of our score was wide (almost a full order of magnitude existed between the lowest and highest values), which may have served to maintain the sensitivity of the score at the expense of transferability between different sites. Nevertheless, the validity of the EDWIN score had been inconsistent in studies published since its original description.17, 25
Another consideration was that patient satisfaction survey data obtained from Press-Ganey were only available in 8-hour shift increments, which may have limited the sensitivity of our analysis. Individual patient data were not available. As such, it was plausible that greater crowding variability existed within each distinct 8-hour period.
CONCLUSION
Increased crowding, as measured by ED occupancy rate and EDWIN score, was significantly associated with reduced patient satisfaction. Although causative attribution was limited, our study suggested yet another negative impact resulting from ED crowding.
Footnotes
Supervising Section Editor: Jeffrey Druck, MD
Submission history: Submitted November 27, 2011; Revision received April 26, 2012; Accepted July 16, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.11.11456
Address for Correspondence: Yaniv Kerem, MD, University of Chicago Medical Center, Section of Emergency Medicine, 5841 S. Maryland Avenue, Chicago, IL 60637
Email: ykerem@uchicago.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. American College of Emergency Physicians Crowding. Ann Emerg Med. 2006;47:585.
2. Instite of Medicine The future of emergency care in the United States health system. Ann Emerg Med. 2006;48:115–120. [PubMed]
3. Gibbs N. “Do you want to die?” The crisis in emergency care is taking its toll on doctors, nurses–and patients. Time. 1990;135:58–60. 62–55. [PubMed]
4. Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006;355:1300–1303.[PubMed]
5. Moskop JC, Sklar DP, Geiderman JM, et al. Emergency department crowding, part 1–concept, causes, and moral consequences. Ann Emerg Med. 2009;53:605–611. [PubMed]
6. Derlet RW, Richards JR. Emergency department overcrowding in Florida, New York, and Texas.South Med J. 2002;95:846–849. [PubMed]
7. Miro O, Antonio MT, Jimenez S, et al. Decreased health care quality associated with emergency department overcrowding. Eur J Emerg Med. 1999;6:105–107. [PubMed]
8. Pines JM, Hollander JE, Localio AR, et al. The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Acad Emerg Med. 2006;13:873–878. [PubMed]
9. Schull MJ, Vermeulen M, Slaughter G, et al. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med. 2004;44:577–585. [PubMed]
10. Sprivulis PC, Da Silva JA, Jacobs IG, et al. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust.2006;184:208–212. [PubMed]
11. Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20:402–405. [PMC free article][PubMed]
12. Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136. [PubMed]
13. Pines JM, Iyer S, Disbot M, et al. The effect of emergency department crowding on patient satisfaction for admitted patients. Acad Emerg Med. 2008;15:825–831. [PubMed]
14. Ross CK, Steward CA, Sinacore JM. A comparative study of seven measures of patient satisfaction. Med Care. 1995;33:392–406. [PubMed]
15. McCarthy ML, Aronsky D, Jones ID, et al. The emergency department occupancy rate: a simple measure of emergency department crowding? Ann Emerg Med. 2008;51:15–24. 24 e11–12.[PubMed]
16. Bernstein SL, Verghese V, Leung W, et al. Development and validation of a new index to measure emergency department crowding. Acad Emerg Med. 2003;10:938–942. [PubMed]
17. Weiss SJ, Ernst AA, Nick TG. Comparison of the National Emergency Department Overcrowding Scale and the Emergency Department Work Index for quantifying emergency department crowding. Acad Emerg Med. 2006;13:513–518. [PubMed]
18. Wuerz RC, Milne LW, Eitel DR, et al. Reliability and validity of a new five-level triage instrument. Acad Emerg Med. 2000;7:236–242. [PubMed]
19. Begley CE, Chang Y, Wood RC, et al. Emergency department diversion and trauma mortality: evidence from houston, Texas. J Trauma. 2004;57:1260–1265. [PubMed]
20. Johnson KD, Winkelman C. The effect of emergency department crowding on patient outcomes: a literature review. Adv Emerg Nurs J. 2011;33:39–54. [PubMed]
21. Bayley MD, Schwartz JS, Shofer FS, et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med.2005;45:110–117. [PubMed]
22. Krochmal P, Riley TA. Increased health care costs associated with ED overcrowding. Am J Emerg Med. 1994;12:265–266. [PubMed]
23. Rondeau KV, Francescutti LH. Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction. J Healthc Manag. 2005;50:327–340. 341–322. discussion.[PubMed]
24. Harris B, Bai JC, Kulstad EB. Crowding Does Not Adversely Affect Time to Percutaneous Coronary Intervention for Acute Myocardial Infarction in a Community Emergency Department. Ann Emerg Med. 2011
25. Jones SS, Allen TL, Flottemesch TJ, et al. An independent evaluation of four quantitative emergency department crowding scales. Acad Emerg Med. 2006;13:1204–1211. [PubMed]