| Author | Affiliation |
|---|---|
| Zlatan Coralic, PharmD, BCPS | University of California San Francisco, Department of Emergency Medicine, San Francisco, California; University of California San Francisco, Department of Clinical Pharmacy, San Francisco, California |
| Hemal K. Kanzaria, MD, MS | University of California Los Angeles, Department of Emergency Medicine, Los Angeles, California |
| Lisa Bero, PhD | University of California San Francisco, Department of Clinical Pharmacy, San Francisco, California |
| John Stein, MD, MAS | University of California San Francisco, Department of Emergency Medicine, San Francisco, California |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
Appendix
ABSTRACT
Introduction
Emergency department clinical pharmacists (EPh) serve a relatively new clinical role in emergency medicine. New EPh may still face barriers prior to working in the emergency department (ED), including staff acceptance. We aimed to assess staff perceptions of a university hospital EPh program 1 year after implementation.
Methods
We sent an electronic survey consisting of 7 multiple-choice questions, 17 5-point Likert-scale questions, and 1 free-text comment section to ED providers and nurses. The qualitatively validated survey assessed staff’s general perceptions of the EPh and their clinical work.
Results
We received responses from 14 attending physicians, 34 emergency medicine residents, 5 mid-level providers, and 51 nurses (80% response rate). Overall, the ED staff strongly supported the presence of an EPh. All of the respondents consulted the EPh at least once in their previous 5 ED shifts. Most respondents (81%) felt the EPh’s availability for general consultation and aid during resuscitations served as the major contribution to medication and patient safety. The participants also expressed that they were more likely to consult a pharmacist when they were located in the ED, as opposed to having to call the main pharmacy.
Conclusion
The EPh model of practice at our institution provides valuable perceived benefit to ED providers.
INTRODUCTION
Background
Emergency department clinical pharmacists (EPh) have had a presence in emergency medicine since the 1970s.1 However, it is only within the last decade that evidence has begun to emerge supporting the clinical benefits of an EPh’s bedside practice in the emergency department (ED).2 The EPhs are doctors of pharmacy and are usually residency trained or have training in critical or ambulatory pharmacotherapy.3 While the duties of an EPh vary institutionally, most EPhs provide multiple services including: 1) face-to-face consultations with emergency physicians, residents, nurses and patients, 2) active assistance with medication management in resuscitations, and 3) provision of distributive services (i.e., order processing and drug supply management). New EPhs may face barriers to practicing within the emergency medicine (EM) clinical team, including institutional financial support, clinical training, and staff’s acceptance and unfamiliarity with clinical pharmacists.
Importance
The EPh serves a relatively new clinical role within EM practice, one that is just starting to be recognized and accepted by the EM community and the national pharmacist societies.4 The published literature to date supporting EPh practice has been positive showing cost avoidance5,6 and reduction in adverse drug events.7–9 However, EDs may be concerned if the addition of pharmacist in the ED may lead to staff’s dissatisfaction and delays in patient care.10
Goals of this investigation
The primary goal of this investigation was to assess staff perceptions of an EPh program at a university hospital ED 1 year after implementation of the program.
METHODS
Setting and Description of the EPh Program
In October 2009, 2 full-time clinical pharmacists established an EPh program in our institution’s ED with the intent of providing clinical and distributive pharmacy services. Prior to the EPh program, the level of service provided by central pharmacy to the ED included stocking of automated medication dispensing machines and remote order verification. One of the EPhs was a recent general pharmacy residency graduate, while the other had worked as an intensive care unit clinical pharmacist for 3 years. Neither pharmacist had previous experience in emergency medicine or had relevant relationships with the ED staff. Both of the EPhs were certified in basic life support, advanced cardiovascular life support, and pediatric advanced life support. The University of California San Francisco Medical Center Department of Pharmacy funded the EPh program. The annual funds necessary to support a benefited pharmacist 8-hour shift 7-days per week (1.4 full time equivalents) was approximately $ 270,000.
The ED has 30 patient rooms with an estimated 40,000 visits per year and is located in an academic setting with a 4-year EM residency training program. The two EPhs initially provided 8 hours per day coverage and were physically present in the ED 7 days per week. The initial hours of coverage were from 15:30 until midnight and were chosen to cover the period with the highest patient volume. After 4 months, the hours of coverage expanded to 12 hours per day (noon until midnight) after additional funding was obtained. The EPh program was implemented following the general guidelines published by the Agency for Healthcare Research and Quality,3 and focused on improving medication safety and quality of care delivered through prospective and retrospective review of medication orders, EPh bedside response to all resuscitations, in-person medication-related consultations, and rapid preparation of all urgent medications (e.g., rapid sequence intubation medications, thrombolytics etc.).
Survey Design and Selection of Participants
The survey tool we used was originally developed from qualitative work and has been used previously to assess staff perceptions of EPhs at a different institution.11 The survey participants identified themselves only by their role in the ED (e.g., nurse, resident) and the researchers remained blinded to the individual participant. All of the participants provided electronic consent prior to taking the survey. There were no incentives offered for completing the survey. The survey consisted of 7 multiple-choice questions, 17 5-point Likert-scale questions (1 – strongly agree, 5 – strongly disagree), and 1 free-text comment section. We further categorized the free-text comments into general praise, constructive feedback, and negative comments. The ED staff was identified using the department’s roster of providers. The University of California San Francisco Committee on Human Research approved this study through expedited review.
Data Collection and Processing
In January 2011, 1 year and 3 months after the implementation of the EPh program, we sent the survey electronically via institutional e-mail to the ED staff using software available in the public domain (SurveyMonkey. com, LLC; Palo Alto, California). Participants were allowed a 2-week period to respond to the survey with 1 e-mail reminder sent after the first week. We excluded incomplete surveys (less than 20% answered questions) from the final analysis. The survey was advertised at the institution’s residency teaching conference and nursing shift-change to encourage participation.
Primary data analysis
Survey results were exported and analyzed in Microsoft Excel (Microsoft Corporation, Redmond, WA). The results of the survey are presented using descriptive statistics.
RESULTS
Characteristics of Study Subjects
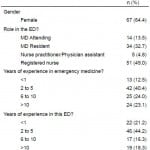
Of the 130 individuals contacted to participate in this study, we received survey responses from 104 (80% response rate) (Table 1). Two participants answered only the first page of the survey (questions 1–4), and we excluded their results from the final analysis. There were a total of 29 attending physicians, 36 residents, 57 nurses, and 8 mid-levels eligible to participate. Clinicians, including attending physicians, EM residents, nurse practitioners, and physician assistants, accounted for 51% of respondents, while nurses accounted for 49%. There were 49 (47.1%) participants who had greater than 6 years of experience in EM.
Table 1. Demographics of participants surveyed regarding perceptions of emergency department (ED) clinical pharmacists (n=104).
Main results
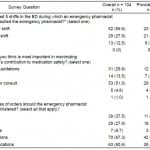
Respondents’ general perceptions to EPhs are shown in Table 2. Overall, ED providers at our institution supported the presence of an EPh. All of the participants consulted the EPh at least once in their last 5 shifts. Most respondents felt the EPh’s availability for general consultation and aid during resuscitations served as the major contribution to medication and patient safety. Participants felt that the EPh should review high risk (67.3%) and rarely used medications (60.6%). The nurses felt stronger (54.9%) about the EPh reviewing all medication orders when compared to providers (20.8%).
Table 2. Staff’s general perceptions of the emergency department (ED) clinical pharmacist.
Survey respondents strongly agreed or agreed that EPh were useful in various clinical situations, including the selection of an appropriate antibiotic (89%), advice on other non-antibiotic medications (94%), drug choice in pregnancy (91%), consultations regarding drug interactions (100%) and toxicology-related cases (85%), assistance with procedural sedation (82%), and resuscitations (96%). The survey participants also felt that the EPh was useful in making medication decisions based on clinical efficacy (87%) and less so based on medication pricing (58%).
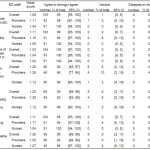
The responses to perceptions of the EPh’s role in the ED are shown in Table 3. The survey participants strongly agreed that EPhs have a beneficial role in the care of EM patients. The participants also strongly agreed with consulting EPh when they were located in the ED, as opposed to having to call the main pharmacy, with a mean Likert score 1.03. Furthermore, the participants strongly agreed that the EPh was a valuable teaching resource for the ED staff with a mean Likert score of 1.11.
Table 3. Staff’s responses concerning the role of the emergency department clinical pharmacist (EPh).
 The free-text responses were provided by 62 (60%) participants, and were further categorized into general praise 51 (82.4%), constructive feedback 10 (16%) and 1 negative comment (1.6%), with unedited examples shown in the Appendix. The constructive feedback themes included: increasing hours of EPh coverage, having a dedicated ED pharmacist, encouraging a pharmacist teaching role with the residents, prospective interventions, medication in-services, and increasing training time for new EPhs.
The free-text responses were provided by 62 (60%) participants, and were further categorized into general praise 51 (82.4%), constructive feedback 10 (16%) and 1 negative comment (1.6%), with unedited examples shown in the Appendix. The constructive feedback themes included: increasing hours of EPh coverage, having a dedicated ED pharmacist, encouraging a pharmacist teaching role with the residents, prospective interventions, medication in-services, and increasing training time for new EPhs.
DISCUSSION
This is the first study that evaluates the perceptions of ED staff towards EPh only 1 year after the start of an EPh program. In general, the respondents were very supportive of the EPh. One prior study evaluated a well-established EPh program and showed similar results.11 Our findings contribute further, indicating that within a short time, the EPh program can be integrated into the EM model to provide support to physicians, nurses, and patients.
Study participants indicated frequent EPh consultation. While nursing staff more often consulted the EPh multiple times during their 5 most recent shifts, all participants consulted the EPh at least once in the same time period. This difference may be due to nurses encountering medication-related issues more frequently in the ED than physician providers (i.e. medication compatibilities, rate of administration, location of medications, high-risk medication double-checks). The difference might also reflect a nurses’ initiative to verify the safety of ordered medications prior to administration, as medications in the ED are usually administered without safety mechanisms found in other areas of the hospital. For example, most floor patients receive patient-specific medications that have been verified, labeled, or packaged by pharmacists adding a safety layer which usually does not exist in an ED environment. Furthermore, our EPh’s workstation was adjacent to the resuscitation rooms in close proximity of the main nursing station, which could further explain this difference. Nevertheless, providers and nurses frequently consulted the EPh in person during the study period. The provider-nurse-pharmacist face-to-face interaction may be especially important during resuscitations when high-risk medications are administered at the point of care, usually from verbal orders, in a high-stress environment.
A recent controversial mandate proposed by The Joint Commission to reduce medication errors was the recommendation for prospective pharmacist review of all non-urgent medications administered in the ED. Although later revised and liberated in interpretation due to the EM community’s concern about delay in therapy,10 the mandate did identify an important issue of medication safety in EM. Our EPhs review medication orders prospectively and retrospectively; however, EPh triage their time based on patients’ acuity, dedicating most time to prospective provider consultations (~50%), clinical participation in resuscitations and emergent clinical scenarios (~20%), and order review and administrative tasks (~30%). Our survey did not reflect any perceived delays in care other than 1 negative comment, and the majority of participants strongly agreed that the EPh presence improves quality of care in the ED. Further, recent multicenter study of comparable EPh programs found a significant interception of medication errors via EPh consultative activities, and to a lesser extent, via order review.8 In another study, the bedside presence of EPh was associated with decreased door-to-balloon time in ST-segment elevation myocardial infarction.12 The potential of ED pharmacist to reduce door-to-medication administration times and impact on clinical patient outcomes need further study.
Realistically, it would be challenging to implement a prospective review of all medications ordered and administered in the ED due to frequent emergent situations and clinical scenarios in which delaying therapy would be unethical (i.e. pain control). It is our opinion that the most benefit from EPh’s presence in the ED will be gained by proactive clinical support and triaged prospective review of medications based on clinical urgency and the likelihood of the medications causing harm.
The cost containment data associated with EPh presence in the ED has been limited to studies performed in individual institutions.5–6 The average baseline salary of a hospital pharmacist at our institution ranges from $130,000 $150,000 per year.13 However, one prospective observational study showed that during a 4-month period, pharmacist interventions in the ED similar to those performed by our EPhs reduced cost by $192,923 via prevention of additional treatments, drug cost avoidance, and provision of drug consultations.5 In another study, the investigators found a total cost avoidance of $1,029,776 in the same time frame via prevention of drug interactions/incompatibilities, therapeutic recommendations, and avoidance of adverse drug events and medication errors.6 Furthermore, our model of EPh practice may represent a financially sound approach to incorporating a pharmacist into the ED, as the EPh fulfilled central pharmacy distributive needs (order processing and dispensing) while physically providing clinical support in the ED via interventions similar to those previously described.
Our survey indicated that only 58% of participants found the EPh useful in decisions based on medication pricing. This may reflect the general medication practice in the ED, where the cost of commonly prescribed medications is infrequently used for clinical decision-making.
One of the concerns voiced in our survey was the heavy reliance of nurses and residents on the EPh for medication-related support. Especially for residents who subsequently practice at sites where EPh are not available, it is possible that EPh may have a detrimental effect on their training. Our group adjusted the EPh practice by extending a bedside teaching role with the residents and the nurses, including periodic medication related in-services. Further, by popular demand from EM residents, a 4-week clinical pharmacy elective was created focusing on drug therapies relevant to EM. The elective has been filled with EM residents 10 out of 25 months since it became available and with pharmacy residents for the remainder of the time. The impact of these added interventions are currently being investigated.
LIMITATIONS
The limitations of our study include that our EPh program was established at a single university teaching hospital and that the results may not be generalizable to other ED settings. Additionally, one EPh was a residency-trained pharmacist while the other had experience in critical care, and our results may not reflect pharmacists with different levels of training. The EPh was physically present in the ED up to 12 hours per day, and acceptance of programs with less presence and visibility might vary.
The ED staff’s perceptions of existing pharmacy services prior to the implementation of the EPh were not collected. Since the EPh was a novel intervention, there is a possibility that participants may have over-estimated the benefit of the EPh due to the prior minimal pharmacy support.
We are limited by the survey design and response rate, especially from the attending physicians. The results may have been subject to recall bias, and it is also possible that there was significant non-response bias. However, even if those with highly negative attitudes were more likely to not respond, our results would not vary substantially. For example, we performed a sensitivity analysis showing that if all 26 eligible participants who did not respond put all of their responses in the “strongly disagree” category, the overall Likert-mean score would change to 2.08, or “agree” overall.
CONCLUSION
The EPh model of practice at our institution, based on a model proposed by Faribanks,3 maximizes the use of clinical pharmacists in the ED and provides valuable perceived benefit to providers. Influence on patient outcomes and the highest-impact model of practice for EPh will need to be addressed with future studies.
Appendix
Footnotes
Address for Correspondence: Zlatan Coralic, PharmD, BCPS. 505 Parnassus Avenue M39, San Francisco, CA 94143. Email: zlatan.coralic@ucsfmedctr.org. 3 / 2014; 15:205 – 210
Submission history: Revision received April 29, 2013; Submitted November 18, 2013; Accepted November 22, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. Dr. Hemal Kanzaria is supported by the Robert Wood Johnson Foundation Clinical Scholars program.
REFERENCES
1. Elenbaas RM, Waeckerle JF, McNabney WK. The clinical pharmacist in emergency medicine. Am J Hosp Pharm. 1977; 34:843-846.
2. Rudis MI, Attwood RJ. Emergency medicine pharmacy practice. J Pharm Pract. 2011; 24:135-145.
3 . Clinical pharmacists in emergency medicine. Agency for Healthcare Research and Quality 2008. Available at: http://www.ahrq.gov/downloads/pub/advances2/vol4/advances-fairbanks_20.pdf. Last accessed December 14, 2012.
4. Eppert HD, Reznek AJ ASHP. Guidelines on Emergency Medicine Pharmacist Services. Am J Health Syst Pharm. 2011; 68:e81-e95.
5 Ling JM, Mike LA, Rubin J, et al. Documentation of pharmacist interventions in the emergency department. Am J Health Syst Pharm. 2005; 62:1793-1797.
6. Lada P, Delgado G. Documentation of pharmacists’ interventions in an emergency department and associated cost avoidance. Am J Health Syst Pharm. 2007; 64:63-68.
7. Rothschild JM, Churchill W, Erickson A, et al. Medication errors recovered by emergency department pharmacists. Ann Emerg Med. 2010; 55:513-521.
8. Patanwala AE, Sanders AB, Thomas MC, et al. A prospective, multicenter study of pharmacist activities resulting in medication error interception in the emergency department. Ann Emerg Med. 2012; 59:369-373.
9. Cesarz JL, Steffenhagen AL, Svenson J, et al. Emergency department discharge prescription interventions by emergency medicine pharmacists. Ann Emerg Med. 2013; 61:209-214.e1.
10. Medication reconciliation standard letter to the Joint Commission. American College of Emergency Physicians, 2006. Avaliable at: http://www.acep.org/Clinical—Practice-Management/Medication-Reconciliation-Standard-Letter-to-Joint-Commission—May-2006/. Last accessed December 14, 2012.
11. Fairbanks RJ, Hildebrand JM, Kolstee KE, et al. Medical and nursing staff highly value clinical pharmacists in the emergency department. Emerg Med J. 2007; 24:716-718.
12. Acquisto NM, Hays DP, Fairbanks RJT, et al. The Outcomes of Emergency Pharmacist Participation during Acute Myocardial Infarction. J Emerg Med. 2012; 42:371-378.
13 . University of California Title and Pay Plan, 2012. Available at: http://ucsfhr.ucsf.edu/index.php/staffing/tpp_detail?tc=9247. Last accessed December 14, 2012.