| Author | Affiliation |
|---|---|
| Brad D. Gable, MD, MS | Summa Akron City Hospital, Department of Emergency Medicine, Akron, Ohio; Ohio University Heritage College of Osteopathic Medicine, Athens, Ohio |
| Aimee K. Gardner, PhD | University of Texas Southwestern Medical Center, Dallas, Texas |
| Dan H. Celik, MD | Summa Akron City Hospital, Department of Emergency Medicine, Akron, Ohio |
| Mary Colleen Bhalla, MD | Summa Akron City Hospital, Department of Emergency Medicine, Akron, Ohio; Northeast Ohio Medical University, Department of Emergency Medicine, Rootstown, Ohio |
| Rami A. Ahmed, DO | Summa Akron City Hospital, Department of Emergency Medicine, Akron, Ohio; Northeast Ohio Medical University, Department of Emergency Medicine, Rootstown, Ohio |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
Appendix
ABSTRACT
Introduction
Obesity is prevalent in the United States. Obese patients have physiologic differences from non-obese individuals. Not only does transport and maintenance of these patients require use of specialized equipment, but it also requires a distinct skill set and knowledge base. To date, there is no literature investigating simulation as a model for educating pre-hospital providers in the care of bariatric patients. The purpose of this study was to determine if a 3-hour educational course with simulation could improve paramedics’ knowledge and confidence of bariatric procedures and transport. This study also examined if prior experience with bariatric transport affected training outcomes.
Methods
Our study took place in August 2012 during paramedic training sessions. Paramedics completed a pre- and post-test that assessed confidence and knowledge and provided information on previous experience. They had a 30-minute didactic and participated in 2 20-minute hands-on skills portions that reviewed procedural issues in bariatric patients, including airway procedures, peripheral venous and intraosseous access, and cardiopulmonary resuscitation. Study participants took part in one of two simulated patient encounters. Paramedics were challenged with treating emergent traumatic and/or medical conditions, as well as extricating and transporting bariatric patients. Each group underwent a debriefing of the scenario immediately following their case. We measured confidence using a 5-point Likert-type response scale ranging from 1 (strongly disagree) to 5 (strongly agree) on a 7-item questionnaire. We assessed knowledge with 12 multiple choice questions. Paired-sample t-tests were used to compare pre- and post-simulation confidence and knowledge with a significance level of p≤0.05. We used analysis of covariance to examine the effect of previous experiences on pre-and post-educational activity confidence and knowledge with a significance level of p ≤0.05. Proportions and 95% confidence intervals are presented as appropriate. We determined the magnitude of significant pre-post differences with Cohen’s d. We assessed scale reliability using Cronbach’s alpha and was found to be reliable with scores of 0.83 and 0.88 across pre- and post-test responses, respectively.
Results
Participants exhibited a significant increase in confidence in performing procedures (p<0.01) and knowledge of bariatric patient management (p<0.001) after the simulation. The current study also found an increase in knowledge of transport, vascular access/circulation and airway management (p<0.001). Participant background showed no effects on these changes.
Conclusion
This study suggests that simulation paired with a didactic is an effective method of education for paramedics caring for and transporting bariatric patients. The data show a significant increase in knowledge and confidence with a 3-hour training session, irrespective of previous training or experience with bariatric patients. This is the first study of its kind to apply simulation training for the pre-hospital care of bariatric patients.
INTRODUCTION
Obesity is prevalent in the United States (U.S.). According to the National Center for Health Statistics, more than a third of adults in the U.S. are obese.1 Obesity is associated with several chronic medical conditions, including hypertension, diabetes,2 obstructive sleep apnea (OSA),3,4 and obesity hypoventilation syndrome.5,6 Obese patients have a greater likelihood of requiring medical intervention than those who are not overweight.7 Due to the increased probability of needing medical support, pre-hospital providers need to be current and competent regarding bariatric treatment and transport needs.
Obese patients have physiologic differences from non-obese individuals. These include increased chest wall resistance, increased abdominal pressure, decreased lung capacity, increased airway resistance, increased subcutaneous tissue, and anatomical distortion.8–10 As a result, assessment and treatment of these patients requires specialized knowledge and skill. In addition to the medical challenges posed by bariatric patients, there are also issues regarding transportation and handling of these patients.11–13 Not only does transport and maintenance of these patients require use of specialized equipment, but it also requires a distinct skill set and knowledge base regarding specific maneuvers. Thus, adequate treatment of bariatric patients requires specific training regarding these issues.
To address the distinct needs of bariatric patients, pre-hospital providers must be trained to care for overweight and obese patients. Traditional training often involves didactic presentations and lectures. However, simulation may be an ideal adjunct to the traditional bariatric training approach. Simulation can provide a dynamic hands-on educational model for instructing first responders on the unique challenges of caring for bariatric patients. Simulation has demonstrated a 4 times greater retention of information versus traditional lecture-based education.14 Simulation is also an ideal means to incorporate the learning theory of “deliberate practice,” which is essential for the development of clinical expertise.15 Thus, simulation may be a well-suited alternative or adjunct to traditional training approaches for this special population.
To date, there is no literature investigating simulation as a model for educating pre-hospital providers in the care of bariatric patients. Examining the use of new instructional methodologies within bariatric transport can help identify the efficacy of these approaches and expand understanding of how to best train pre-hospital providers. This study sought to determine if a 3-hour training session could improve paramedics’ knowledge of bariatric transport and confidence to perform bariatric procedures. Additionally, we examined how participant experiences (number of bariatric patients transported in past year and previous training) impacted the efficacy of this training. The current study assessed paramedics with a pre- and post-training survey.
METHODS
Setting
This study was performed at a fire department in a rural Midwestern township. This publicly operated, combined fire and emergency medical services (EMS) department serves a suburban population of 40,373.16 Sixty-nine full-time and 35 part-time paramedics respond to approximately 4,000 calls per year.
Study Participants
All fire department paramedics who were present on one of 3 scheduled continuing medical education sessions participated. We excluded paramedics who were not available for the entire training session due to clinical duty. Dates of the sessions were August 7th, 8th, and 9th, 2012.
Study Design
Study participants were given identical pre- and post-training surveys that focused on confidence in bariatric care, as well as knowledge of bariatric clinical issues. (See Measures below and Appendix) All surveys were de-identified but included a unique number to link pre- and post-questionnaires. Bariatric training consisted of a didactic portion, a skills portion, and a simulated patient encounter. (See Table 1 for curriculum outline). An EMS physician and a practicing paramedic who were not part of the research team reviewed the survey to ensure proper language appropriate for the study participants, to ensure there was no bias and to ensure the questions matched the demographics and experience of the study participants.
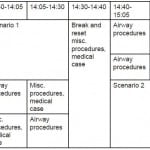
Table 1. Design of 1-day 3-hour training session for paramedics transporting bariatric patients.
The didactic portion included a 30-minute lecture that defined obesity, discussed associated health risks, presented unique EMS care issues, reviewed transfer and mobility concerns, addressed scene and personal safety, and promoted sensitivity and professionalism with regards to bariatric patients.
The 2 20-minute hands-on skills portions reviewed procedural issues in bariatric patients, including airway procedures (Bag-valve-mask, intubation, laryngeal mask airways), peripheral venous and intraosseous access (Vidacare® EZ-IO; Shavano Park, TX), and cardiopulmonary resuscitation (Nasco Life/form® Fat Old Fred Manikin; Fort Atkinson, WI). These task trainers were chosen to demonstrate these skills, as they have the anatomic and physiologic changes present in bariatric patients. In addition, homemade task trainers were used to further practice these skills. Such task trainers included bariatric arms made of ballistics gel and fluid tubing for peripheral venous access, and ballistics gel added to IO mannequins to simulate the greater amount of subcutaneous tissue present in bariatric patients. During the peripheral access/intraosseous access and CPR station, learners were given a case of a bariatric patient needing resuscitation and were to perform venous access and cardiopulmonary resuscitation on the above task trainers.
Study participants took part in one of two simulated patient encounters. The encounters used a water-filled bariatric suit (Simulaids, Inc. Bariatric Rescue Suit; Saugerties, NY), which was placed over a mannequin (Rescue Randy; Saugerties NY) (Figure) and a tarp-style transportation device (Graham Megamover® 1500; Green Bay, WI). The mannequin with bariatric suit, when filled with water, weighed approximately 350 pounds. The first case involved an elderly, morbidly obese male taking dabigatran who fell down a flight of stairs and was unable to get up. The second case described a middle-aged male who used prescription narcotic pills and fell from the toilet and became hypoxic. Although paramedics were challenged with treating emergent traumatic and/or medical conditions, the focus of the simulated patient encounters was on extricating and transporting the bariatric patients. Each group underwent a debriefing of the scenario immediately following their case.
Figure. Mannequin in a water-filled bariatric suit on top of a tarp-style transportation device.
Following the completion of skills stations and the simulation scenario all paramedics were given a post-training survey. After all surveys were collected, the participants discussed the particular case they were presented with during their simulation scenario. The aim of this large-group discussion was to facilitate open dialogue of the difficulties presented during the scenarios and the resultant strategies used to overcome the obstacles. Lastly, the paramedics were given a brief didactic presentation to summarize the medical and transport issues presented by bariatric patients.
Our Institutional Review Board determined that the study was exempt from review due to our de-identifying the data set.
Measures
As part of the pre-survey we collected information on previous training and experience, including number of years of experience, previous bariatric transport participation and the number of bariatric patients transported in the previous year. This information sought to examine if training effects differ among experience levels. For all measures, participants used a Likert-type response scale ranging from 1 (strongly disagree) to 5 (strongly agree).
The current study also assessed confidence in bariatric transport as part of the pre- and post-surveys with a 7-item questionnaire. Example items included “I feel confident that I can properly assess a bariatric patient” and “Can identify local resources to help in emergency management of bariatric patients” (Appendix). For each item subjects used the Likert-type response previously described. We assessed study participants’ knowledge on the treatment and transportation of bariatric patients with 12 multiple-choice items. We developed the multiple choice questions based on the learning objectives for the educational session. These questions evaluated knowledge of bariatric airway management, vascular access/circulation, and transport (Appendix).
Statistical Analysis
We performed all statistical analysis with SPSS (version 18.0; Chicago, IL). Paired-sample t-tests were used to compare pre- and post-simulation confidence and knowledge with a significance level of p≤0.05. We used analysis of covariance (ANCOVA) to examination the effect of previous experiences on pre-and post-educational activity confidence and knowledge with a significance level of p≤0.05. Proportions and 95% confidence intervals are presented as appropriate. Scale reliability was assessed using Cronbach’s alpha. Additionally, we determined magnitude of significant pre-post differences with Cohen’s d.
RESULTS
Pre- and post-training responses from 36 paramedics were available for evaluation. We excluded responses from 5 paramedics who did not complete either a pre-test or a post-test due to being called away from the training session to respond to an emergency call. Of the final sample, 22% (8/36) had participated in bariatric transport training previously (none of which included simulation) and 42% (15/36) had transported at least 5 bariatric patients in the past year. Paramedic experience ranged from 1 to 35 years, with an average of 19.5 years.
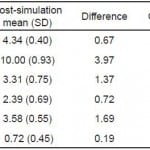
Participants exhibited a significant increase in confidence in performing procedures (p<0.01) assessed by comparing the overall mean confidence for the 7 statements on the pre-test to the post-test (Table 2). Participants also significantly increased their knowledge of bariatric patient management (p<0.001) assessed by comparing the mean number of answers correct on the pre-test to the post-test (Table 2). The data also show an increase in knowledge of transport, vascular access/circulation and airway management (p<0.001) (Table 2).
Table 2. Comparison of bariatric confidence and knowledge scores before and after simulation.
Finally, we examined the magnitude of these effects using Cohen’s d. Conventionally, the size of an effect is determined to be small if greater than 0.20, medium if greater than 0.50, and large if greater than 0.80 (Cohen, 1992). As indicated in Table 2, changes in bariatric confidence and knowledge exhibited large effects. Participant background (number of bariatric patients transported in past year and previous training) showed no effects on these changes (p=0.43; p=0.65, respectively).
The bariatric transport knowledge scale exhibited good reliability, with a Cronbach’s alpha at 0.83 and 0.88 across pre- and post-simulation responses, respectively.
DISCUSSION
The effectiveness of simulation-based training has been confirmed in a number of healthcare realms.17–26 However, researchers have yet to investigate the efficacy of this approach within bariatric transport. One of the strengths of this study is its novelty, as this is the first study to examine the use of simulation in the training of pre-hospital personnel for treating bariatric patients.
These results reveal that a 30-minute didactic lecture combined with simulation training can have a valuable impact on paramedic bariatric transport and medical knowledge. Specifically, paramedics exhibited increases in understanding of the unique airway, vascular access, and transport needs of bariatric patients. Despite 22% of the trainees having had previous formal training in bariatric transport and over 40% having transported at least 5 patients in the last year, the improvement in knowledge and confidence among both previously trained/experienced providers and novices was similar. Although a large portion of paramedics had previously been educated on bariatric transport and treatment, having an opportunity to learn in a hands-on format may have allowed participants to gain a deeper understanding of bariatric patient issues. Simulation is a unique educational technique. Simulation in combination with traditional teaching methods may prove with future randomized studies to be superior for learning certain skills than traditional teaching alone.
Study participants also reported an increase in confidence to perform procedures on bariatric patients after the training. This enhanced confidence can manifest itself in a number of ways for paramedics. Paramedics who are more confident caring for bariatric patients may also be more likely to exhibit guidance to other paramedics not similarly trained, speak up to team members performing tasks incorrectly, and execute procedures with controlled emotions. This outcome, combined with the observed knowledge improvement, is especially noteworthy. These findings fall in line with previous simulation-based studies that indicate leadership and teamwork training provided in simulated environments demonstrates both increased confidence to perform new procedures and decreased apprehension to try new techniques clinically.27–30 This is particularly important as many bariatric patients will require a multidisciplinary team effort to safely manage and transport them to definitive care.
The current study demonstrates favorable trainee outcomes after participating in a 30-minute lecture, a 50-minute simulation, a 25-minute case-based scenario, and a 25-minute task training skill station. Although the didactic portion of this training may have contributed to some of the knowledge acquisition, we believe that it was not the sole contributing factor. The initial didactic discussion was included to provide an overview of bariatric patient concerns, provide understanding of why the training was necessary, and to assure participant safety during the scenarios. Further, as trainees had varying degrees of experience previously caring for bariatric patients, the lecture ensured that all trainees would enter the simulation sessions with an adequate baseline knowledge level to participate in the simulation scenarios. For example, in the initial lecture, participants were told that they may not be able to use traditional cervical spine and long board immobilization and that alternative means may be necessary. During the simulation, trainees had to troubleshoot immobilization techniques to identify effective and ineffective strategies. This understanding, as well as its long-term retention, is unlikely to be demonstrated without interactive hands-on training provided in simulated environments.14 According to Kirkpatrick26 training should be evaluated at 4 levels: reactions, learning, behavior, and results. Whereas many simulation studies investigate solely trainee attitudes, our investigation went an additional step and examined if trainees learned the knowledge relevant to managing bariatric patients.
During the large-group discussion we sought the feedback of the learners. The most common critique was that the scenarios they encountered could have been more challenging. The extrication and transportation took place in a firehouse, which is a local storm and disaster shelter and contains widened staircases and handicap -accessible bathrooms. Future training sites could include more difficult extrication sites or modification of existing sites to simulate the inside of a home or apartment building.
Obese patients present unique challenges to healthcare providers. As this population continues to grow, the healthcare system can expect to encounter such patients with increasing frequency and must prepare accordingly. Knowing how to deliver appropriate care in a safe and effective manner, while maintaining the patient’s dignity, is of the utmost importance.
LIMITATIONS
This small pilot study evaluated learners immediately before and after a simulation-based curriculum that incorporates a didactic session, skill stations, and simulated scenarios. Further investigation into the long-term retention of the knowledge learned from this education session is needed. Additionally, the results reflect the educational session as a whole, and further studies would be needed to determine the effect that simulation or the didactic session has on knowledge acquisition. Future studies should include an assessment of skills as well.
Additionally, the data were obtained from a single EMS service and may not be generalizable to all levels of pre-hospital providers. Future studies should examine if such learning is successfully transferred to the work environment and how such knowledge impacts patient outcomes.
CONCLUSION
The current study suggests that a simulation-based curriculum that incorporates a didactic session, skill stations, and simulated scenarios is an effective method of education for paramedics caring for and transporting bariatric patients. This study shows a significant increase in knowledge and confidence with a 3-hour training session, irrespective of previous training or experience with bariatric patients. This is the first study of its kind to apply simulation training for the pre-hospital care of bariatric patients.
Appendix
Footnotes
Address for Correspondence: Mary Colleen Bhalla, Summa Akron City Hospital, Department of Emergency Medicine, 525 East Market Street, PO Box 2090, Akron, OH 44304. Email: bhallam@summahealth.org. 3 / 2014; 15:199 – 204
Submission history: Revision received July 2, 2013; Submitted November 15, 2013; Accepted December 3, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors alone are responsible for the content and writing of the paper. No funding or financial support was obtained for this research.
REFERENCES
1. Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity in the United States, 2009–2010. NCHS Data Brief. 2012;(82):1-8.
2. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—The evidence report. Obes Res. 1998;6:51S-209S.
3. Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230-1235.
4. Duran J, Esnaola S, Rubio R, et al. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med. 2001; 163:685-689.
5. Leech JA, Onal E, Baer P, et al. Determinants of hypercapnia in occlusive sleep apnea syndrome. Chest. 1987; 92:807-813.
6. Mokhlesi B, Tulaimat A, Faibussowitsch I, et al. Obesity hypoventilation syndrome: prevalence and predictors in patients with obstructive sleep apnea. Sleep Breath. 2007; 11:117-124.
7. Cui R, Iso H, Toyoshima E, et al. Body mass index and mortality from cardiovascular disease among Japanese men and women: the JACC study. Stroke. 2005; 36:1377-1382.
8. Rabec C, de Lucas RP, Veale D. Respiratory complications of obesity. Arch Bronconeumol. 2011;47:252-261.
9. BaHammam A. Acute ventilatory failure complicating obesity hypoventilation: update on a critical care syndrome. Curr Opin Pulm Med. 2010;16:543-551.
10. Sabbane M, Claret P, Lefebvre S, et al. Predicting peripheral venous access difficulty in the emergency department using body mass index and a clinical evaluation of venous accessibility. J Emerg Med. 2013;44:299-305.
11. Hignett S, Griffiths P. Manual handling risks in the bariatric (obese) patient pathway in acute sector, community and ambulance care and treatment. Work. 2009; 33:175-180.
12. Grant P, Newcombe M. Emergency management of the morbidly obese. Emerg Med Aus. 2004; 16:309-317.
13. Hignett S, Griffiths P. Risk Factors for moving and handling bariatric paitents. Nursing Standard. 2009; 24:40-48.
14. Dale E. Audio-Visual Methods in Teaching.3rd Ed. New York: Holt, Rinehart, & Winston; 1969:108
15. Ericsson K. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79:S70-81.
16 . Unknown. (2010) OH – Jackson Township. [online] Available at: http://www.census.gov/popfinder/?fl=39:3915138094 [Accessed: November 16, 2012].
17. Seymour N, Gallagher A, Roman SA, et al. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg. 2002; 236:458-464.
18. Sroka G, Feldman L, Vassiliou MC, et al. Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room- a randomized control trial. Am J Surg. 2010;199:115-120.
19. Britt R, Novosel T, Britt LD, et al. The impact of central line simulation before the ICU experience. Am J Surg. 2009;197:533-536.
20. Barsuk J, McGaghie W, Cohen ER, et al. Use of Simulation-based mastery learning to improve the quality of central venous catheter placement in a medical intensive care unit. J Hosp Med. 2009; 4:397-403.
21. Barsuk J, McGaghie W, Cohen ER, et al. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med. 2009; 37:2697-2701.
22. Holcomb JB, Dumire RD, Crommett JW, et al. Evaluation of trauma team performance using and advanced human patient simulator for resuscitation training. J Trauma. 2002; 52:1078-1086.
23. Wayne DB, Didwania A, Feinglass J, et al. Simulation-based education improves the quality of care during cardiac arrest team responses at an academic teaching hospital: a case-control study. Chest. 2008; 133:56-61.
24. Chopra V, Gesink B, de Jong J, et al. Does training on the anesthesia simulator lead to improvement in performance?. Br J Anaesth. 1994;73:293-297.
25. Wayne D, Siddall V, Butter J, et al. A longitudinal study of internal medicine residents’ retention of advanced cardiac life support skills. Acad Med. 2006; 81:S9-S12.
26. Kirkpatrick DL. Evaluation of training. In: Craig RL., ed. Training and Development Handbook: A Guide to Human Resource Development. 2nd ed. New York: McGraw-Hill; 1976:1-26.
27. Capella J, Smith S. Teamwork training improves the clinical care of trauma patients. J Surg Educ. 2010;67:439-443.
28. Ten Eyck R, Tews M. Improved fourth-year medical student clinical decision-making performance as a resuscitation team leader after a simulation-based curriculum. Simul Healthc. 2010;5:139-145.
29. Evans L, Dodge K. Simulation training in central venous catheter insertion: improved performance in clinical practice. Acad Med. 2010; 85:1462-1469.
30. Barsuk J, McGaghie W. Use of simulation-based mastery learning to improve the quality of central venous catheter placement in a medical intensive care unit. J Hosp Med. 2009; 4:397-403.