| Author | Affiliation |
|---|---|
| Donald Schreiber, MDCM | Division of Emergency Medicine, Stanford University School of Medicine, Stanford, California |
| Ayesha Sattar, DO | Division of Emergency Medicine, Stanford University School of Medicine, Stanford, California |
| Dorian Drigalla, MD | Department of Emergency Medicine, Texas A&M College of Medicine, Temple, Texas |
| Steven Higgins, MD | Department of Cardiology, Scripps Memorial Hospital, La Jolla, California |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Many emergency department (ED) patients have symptoms that may be attributed to arrhythmias, necessitating outpatient ambulatory cardiac monitoring. Consensus is lacking on the optimal duration of monitoring. We describe the use of a novel device applied at ED discharge that provides continuous prolonged cardiac monitoring.
Methods
We enrolled discharged adult ED patients with symptoms of possible cardiac arrhythmia. A novel, single use continuous recording patch (Zio®Patch) was applied at ED discharge. Patients wore the device for up to 14 days or until they had symptoms to trigger an event. They then returned the device by mail for interpretation. Significant arrhythmias are defined as: ventricular tachycardia (VT) ≥4 beats, supraventricular tachycardia (SVT) ≥4 beats, atrial fibrillation, ≥3 second pause, 2nd degree Mobitz II, 3rd degree AV Block, or symptomatic bradycardia.
Results
There were 174 patients were enrolled and all mailed back their devices. The average age was 52.2 (± 21.0) years, and 55% were female. The most common indications for device placement were palpitations 44.8%, syncope 24.1% and dizziness 6.3%. Eighty-three patients (47.7%) had ≥1 arrhythmias and 17 (9.8%) were symptomatic at the time of their arrhythmia. Median time to first arrhythmia was 1.0 days (IQR 0.2–2.8) and median time to first symptomatic arrhythmia was 1.5 days (IQR 0.4–6.7). 93 (53.4%) of symptomatic patients did not have any arrhythmia during their triggered events. The overall diagnostic yield was 63.2%
Conclusion
The Zio®Patch cardiac monitoring device can efficiently characterize symptomatic patients without significant arrhythmia and has a higher diagnostic yield for arrhythmias than traditional 24–48 hour Holter monitoring. It allows for longer term monitoring up to 14 days.
INTRODUCTION
Symptoms attributed to possible cardiac arrhythmias, such as syncope, palpitations or dizziness, are common presenting complaints to the emergency department (ED) and may account for 3–4% of all ED visits. ED management is driven by risk assessment and current guidelines.1–5 Admission rates, however, remain high and inpatient management is expensive.6 Outpatient management for ED patients has been complicated by logistical barriers to outpatient ambulatory cardiac monitoring such as the need for cardiology consultation, availability of cardiac monitoring devices and patient compliance.
Importance
The gold standard for diagnosing an arrhythmia as the etiology for the patient’s symptoms is electrocardiogram (ECG) documentation of a rhythm disturbance at the time of symptoms.1–5 The optimal device for ambulatory cardiac monitoring is based on the frequency of symptoms. Typically, a 24–48 hour Holter monitor is used.1–3,6,7 However, consensus is lacking in the literature on the optimal duration of cardiac monitoring. The American College of Emergency Physicians’ clinical policy on syncope suggests that Holter monitoring beyond 24 hours is unlikely to increase detection of significant arrhythmias.3 Other authors report that 24-hour Holter monitoring is insufficient, and ambulatory cardiac monitoring for 1–6 weeks may be required.7–10
Goals of this Investigation
In this study, we describe the use of a novel portable ambulatory cardiac monitoring device applied upon discharge from the ED that provides continuous monitoring for up to 14 days. Our goal was to determine the diagnostic yield of such a device and to determine the value of prolonged monitoring of low-risk discharged ED patients with possible cardiac arrhythmia.
METHODS
Study Design and Setting
We completed an observational study at 3 academic EDs in the United States between February 2011 and February 2012.
Selection of Participants
We enrolled a convenience sample of discharged adult ED patients >18 years of age with symptoms suggestive of possible cardiac arrhythmia who were deemed candidates for outpatient ambulatory cardiac monitoring. All diagnostic testing, final disposition and use of the device were at the discretion of the attending emergency physician. The ambulatory cardiac rhythm monitor was a single use long-term, continuous recording patch (Zio®Patch – iRhythm Technologies, Inc. San Francisco, CA) that was applied by trained ED personnel at discharge. The device is a FDA-approved diagnostic adhesive patch that is affixed to the left anterior chest wall. It continuously records the cardiac rhythm for up to 14 days.
Methods and Measurement
Incorporated into the Zio®Patch is an event marker button that patients are instructed to press when symptomatic. Activation of the event marker button is termed a triggered event, and for purposes of this study it is assumed that the triggered event represented symptoms of possible cardiac arrhythmia. The patient was also provided a diary for written entries of symptoms and times. The cardiac rhythm for 45 seconds before and 45 seconds after a triggered event or diary entry was marked for review. Subjects were instructed to wear the device up to 14 days and then simply mail the device in the supplied pre-addressed postage-paid envelope to the company’s facility. They were also instructed to return to the ED for any recurrent or worsening symptoms. The complete set of continuous rhythm data and the file of triggered events (if any) were downloaded from the device and analyzed using a proprietary algorithm. An initial report was prepared and then sent electronically for cardiology review and is then returned to the ordering physician. The cardiologist reviewed the entire record including all triggered events and the patient diary and generated a summary report.
Outcomes
We defined significant arrhythmias as ventricular tachycardia (VT) ≥4 beats, paroxysmal atrial fibrillation (PAF), supraventricular tachycardia (SVT) ≥4 beats, ≥3 sec pause, 2nd degree Mobitz II or 3rd degree AV block, or symptomatic bradycardia. Serious arrhythmias were defined as: VT >120 for 30 seconds, Complete or 3rd degree heart block, symptomatic second degree heart block, type II, pause >6 seconds and symptomatic bradycardia <40 beats per minute for >30 seconds. If any serious arrhythmias were detected on the initial report, the ED or cardiologist was immediately notified; the patient was then contacted and asked to return, all in accordance with existing policies and procedures for reporting critical results. We also defined analyzable time as the percentage of the entire patient ECG data record that had sufficient fidelity to enable a rhythm analysis. Diagnostic yield was defined as the percentage of all patients who had a triggered event without any arrhythmia found or who had a significant symptomatic arrhythmia detected.
Analysis
We described descriptive statistics using parametric and non-parametric techniques where appropriate. All device data were maintained on the company’s encrypted secure database. We de-identified the data and provided the results for analysis without any protected health information. The study was reviewed and approved by each institution’s institutional review board.
RESULTS
Characteristics of Study Subjects
We enrolled a total of 174 patients; the average age was 52.2 (± 21.0) years and 55% were female. Palpitations (78, 44.8%), syncope (42, 24.1%) and dizziness (11, 6.3%) were the most common indications for ambulatory device placement. Other indications included the detection of specific arrhythmias, such as ventricular tachycardia (14, 8.0%), atrial fibrillation (4,2.3%), bradyarrhythmias (5,2.9%) or unspecified arrhythmias (20, 11.5%) All 174 patients (100%) returned their cardiac monitor for review.
Study Results
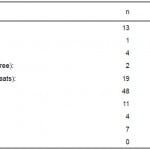
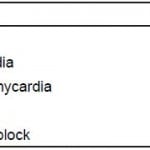
Eighty-three patients (47.7%) had ≥1 significant arrhythmias (excluding chronic atrial fibrillation), and 17 (9.8%) were symptomatic at the time of their arrhythmia. Nine patients (5.2%) had ≥2 arrhythmias. Significant arrhythmias are further detailed in Table 1. There were no significant gender differences identified. Median time to first arrhythmia was 1.0 days (interquartile range [IQR] 0.2–2.8) and median time to first symptomatic arrhythmia was 1.5 days (Mean 3.9, IQR 0.4–6.7). The mean times to first symptomatic event for each arrhythmia are outlined in Table 2. Seven (4.0%) patients required immediate physician notification for serious arrhythmias. There were no patient deaths.
Table 1. Summary of arrhythmias.
In total, 93(53.4%) symptomatic patients did not have any arrhythmia during their triggered events. We calculated the diagnostic yield of 63.2% is calculated to be the number of triggered events without arrhythmias (n=93) and the number of significant symptomatic arrhythmias detected (n=17). Median device wear time was 6.9 days (IQR 5.8–9.2), and the analyzable time was 98.6% of the total recorded data.
DISCUSSION
In this study we describe a novel ambulatory cardiac monitoring device that can easily be applied to patients upon discharge from the ED. It was well tolerated for prolonged monitoring and compliance was excellent. Single channel ECG data quality was also excellent with more than 98% of the total recording time analyzable.
The device had high diagnostic yield for low-risk patients discharged from the ED with primary complaints of palpitations, syncope or dizziness. We observed that the 24–48 duration of traditional Holter monitoring may be inadequate for identifying significant arrhythmias in these patients. For example, the median time to the first triggered arrhythmia in this study for ventricular tachycardia and sinus pauses was 3.1 and 4.2 days respectively, outside the window of traditional Holter monitoring.
The current primary criterion for establishing a cardiac arrhythmia as the cause of syncope, near syncope, palpitations or dizziness rests on the correlation of the arrhythmia with symptoms.1–3,6,7 The clinical challenge in the ED is to identify and admit the high-risk patients and refer the low-risk patients for outpatient evaluation if appropriate.1,6,7 The role of ambulatory cardiac monitoring for ED patients is guided by clinical suspicion for an arrhythmia, the anticipated frequency of recurrent symptoms and whether the patient is low risk and safe for discharge. In practical terms, the logistics of organizing adequate follow up within 14 days of the index ED visit is often problematic for a variety of administrative, financial and system-based reasons. This study demonstrated the ease and utility of initiating ambulatory cardiac monitoring with the Zio®Patch at the time of the index ED visit.
Several devices are currently available to assess cardiac rhythm disturbances in ambulatory patients. The traditional Holter monitor was first introduced to clinical practice in the 1940s.7 The first device was a 75-pound backpack with a reel-reel tape recorder and large batteries. Current technology incorporates flash memory, weighs less than 200 grams and stores 24–48 hours of continuous ECG data but still requires electrodes and wires for patient use.6,7 The major advantages of traditional Holter monitors are the ability to continuously record ECG data and the fact that transmission of data is not patient dependent. However, non-compliance with use of the device or maintaining a log of symptoms limits diagnostic utility.1,7
Event recorders do not record continuous ECG data but require patient activation at the time of symptom onset. These devices may be applied to the chest wall at the time of the event and must be activated by the patient. A brief, typically 90-second, single lead ECG recording is captured and stored on the device. Because of limited data storage capability, these data must be transmitted to a central monitoring center for validation and analysis. Although these devices can be used for cardiac monitoring over longer periods of time, they are limited by the fact that patients must be able to activate the device following symptom onset.7 This may be difficult to achieve, for example, if the patient had syncope or suffered an injury related to the event. Finally, these devices cannot be used to document asymptomatic arrhythmias.2,7
External continuous loop recorders (ELR) are attached to the patient by chest electrodes or a wristband. They continuously record the ECG recording but only save the data if activated by the patient. The continuous looping memory feature allows the device to store a fixed length of pre-activation and post-event ECG data.7
Mobile cardiac telemetry systems (MCOT) provide up to 30 days of real-time continuous cardiac monitoring without the need for patient activation or data transmission. The relative disadvantages of these devices are the higher costs, the need for electrodes and bulky recording devices, as well as the potential burden on the clinician who must be available to review the large amount of data.1,2,6 Implantable loop recorders (ILRs) are surgically implanted subcutaneous devices that continuously record single-lead ECG signal through 2 electrodes. However they are very expensive and necessitate an invasive procedure.1
Traditionally, ambulatory cardiac monitoring is usually initiated with a 24–48 hour Holter monitor. Bass reported a diagnostic yield of 15% with 24-hour Holter monitoring that did not increase even if the device was applied for 72 hours.8 In a prospective study evaluating ELR in syncope, symptom-rhythm correlation was found in 56% with an ELR worn for 1 month versus only 22% for 48 hour Holter monitoring.7,9 In, studies on selected patients with palpitations comparing ELR and 48-hour Holter monitors, the diagnostic yield with Holter monitors was 35%–39%.10 In our study, the overall diagnostic yield was 63.2%, which is considerably higher than traditional 48-hour Holter monitoring and points to the value of up to 14-day ambulatory cardiac monitoring.
The absence of an arrhythmia during syncope, palpitations or a triggered event does not by itself provide a definitive diagnosis but does allow the clinician to exclude an arrhythmia as a potential cause and is thus clinically useful. Over half our patients (53.4%) did not have an arrhythmia despite a triggered event. This allows the clinician to potentially exclude an arrhythmia as an etiology of the patient’s symptoms and potentially avoid further cardiac evaluation.
LIMITATIONS
As an observational convenience study, enrollment was based on clinician discretion alone. Concomitant Holter monitoring could not be provided. There was no randomized comparison to Holter monitor or other traditional management approaches. Demographic data were limited to age and gender, and we did not analyze or compare other clinical characteristics. No long-term follow-up data was obtained. Attributing all triggered events to symptoms may be incorrect without formal patient review. Certain events such as syncope may have occurred during the monitoring period without arrhythmia but the patient may not have been able to activate the event recorder button. While this may have lowered the diagnostic yield, any important arrhythmia would have been detected during the continuous monitoring.
CONCLUSION
This study demonstrated the utility of the Zio®Patch, a novel ambulatory cardiac monitoring device that is applied at discharge for up to 14 days following an ED visit for syncope, palpitations or dizziness. This approach provided relatively prompt diagnoses at both ends of the clinical spectrum, including the documentation of normal sinus rhythm in patients with symptoms, as well as serious asymptomatic arrhythmias in others. Further outcome and economic studies are required to determine if this device will reduce hospital admission rates and improve the diagnostic efficiency for these patients.
Footnotes
Address for Correspondence: Donald Schreiber, MDCM, FRCPC, FACEP, Division of Emergency Medicine, Stanford University School of Medicine, 300 Pasteur Dr., Stanford, CA 94304. Email: donalds@stanford.edu. 3 / 2014; 15:194 – 198
Submission history: Revision received July 12, 2013; Submitted October 30, 2013; Accepted November 11, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. Technical support from iRhyhm Technologies, Inc., San Francisco, CA. iRhyhm Technologies, Inc had no role in the design of the study, the statistical analysis of the data, interpretation of the results or the preparation or review of the manuscript.
REFERENCES
1. Sheldon RS, Morillo CA, Krahn AD, et al. Standardized Approaches to the Investigation of Syncope: Canadian Cardiovascular Society Position Paper. Canadian Journal of Cardiology. 2011; 27:246-253.
2. Moya A, Sutton R, Ammirati F, et al. Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J. 2009; 30:2631-2671.
3. Huff SJ, Decker WW, Quinn JV, et al. Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department with Syncope. Ann Emerg Med. 2007;49:431-444.
4. Zimetbaum P, Josephson ME. Evaluation of Patients with Palpitations. New Engl J Med. 1998; 338:1369-1373.
5. Thavendiranathan P, Bagai A, Khoo C, et al. Does This Patient with Palpitations Have a Cardiac Arrhythmia?. JAMA. 2009; 302:2135-2143.
6. Brignole M, Hamdan MH. New Concepts in the Assessment of Syncope. J Am Coll Cardiol. 2012; 59:1583-1591.
7. Zimetbaum P, Goldman A. Ambulatory Arrhythmia Monitoring: Choosing the right device. Circulation. 2010; 122:1629-1636.
8. Bass EB, Curtiss EI, Arena VC, et al. The duration of Holter monitoring in patients with syncope. Is 24 hours enough?. Arch Intern Med. 1990; 150:1073-1078.
9. Kinlay S, Leitch JW, Neil A, et al. Cardiac event recorders yield more diagnoses and are more cost-effective than 48-hour Holter monitoring in patients with palpitations. A controlled clinical trial. Ann Intern Med. 1996;124:16-20.
10. Gula LJ, Krahn AD, Massel D, et al. External loop recorders: determinants of diagnostic yield in patients with syncope. Am Heart J. 2004; 147:644-648.