| Author | Affiliation |
|---|---|
| Calvin A. Brown, MD | Brigham and Women’s Hospital, Harvard Medical School, Department of Emergency Medicine, Boston, Massachusetts |
| Kelly Cox, MD | University of Illinois-Peoria, Department of Emergency Medicine, Peoria, Illinois |
| Shelley Hurwitz, PhD | Brigham and Women’s Hospital, Harvard Medical School, Department of Medicine, Boston, Massachusetts |
| Ron M. Walls, MD | Brigham and Women’s Hospital, Harvard Medical School, Department of Emergency Medicine, Boston, Massachusetts |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Pre-hospital airway management is a key component of resuscitation although the benefit of pre-hospital intubation has been widely debated. We report a large series of pre-hospital emergency airway encounters performed by air-transport providers in a large, multi-state system.
Methods
We retrospectively reviewed electronic intubation flight records from an 89 rotorcraft air medical system from January 01, 2007, through December 31, 2009. We report patient characteristics, intubation methods, success rates, and rescue techniques with descriptive statistics. We report proportions with 95% confidence intervals and binary comparisons using chi square test with p-values <0.05 considered significant.
Results
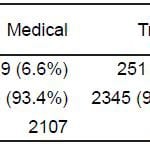
4,871 patients had active airway management, including 2,186 (44.9%) medical and 2,685 (55.1%) trauma cases. There were 4,390 (90.1%) adult and 256 (5.3%) pediatric (age ≤ 14) intubations; 225 (4.6%) did not have an age recorded. 4,703 (96.6%) had at least one intubation attempt. Intubation was successful on first attempt in 3,710 (78.9%) and was ultimately successful in 4,313 (91.7%). Intubation success was higher for medical than trauma patients (93.4% versus 90.3%, p=0.0001 JT test). 168 encounters were managed primarily with an extraglottic device (EGD). Cricothyrotomy was performed 35 times (0.7%) and was successful in 33. Patients were successfully oxygenated and ventilated with an endotracheal tube, EGD, or surgical airway in 4809 (98.7%) encounters. There were no reported deaths from a failed airway.
Conclusion
Airway management, predominantly using rapid sequence intubation protocols, is successful within this high-volume, multi-state air-transport system.
INTRODUCTION
Out-of-hospital tracheal intubation is an accepted but controversial practice. Prior research on patient outcomes after pre-hospital intubation has yielded mixed results with several studies suggesting that, in select groups of trauma patients, it may increase mortality.1–5 Training, protocols, oversight, and frequency of individual provider intubation all might influence success rates and clinical outcome, and previous reports may not represent success rates possible from highly skilled clinicians working in high volume systems.6,7 Previous small studies of air transport intubations have found success rates from 66% to 97%, with higher success seen after the institution of rapid sequence intubation (RSI) protocols.8–13 We report a large consecutive series of intubations performed within an 89 rotorcraft, multi-state transport system in order to characterize methods, success rates and rescue techniques when intubation is performed by flight paramedics and nurses using standardized rapid-sequence intubation protocols.
METHODS
Study Design
This is a retrospective analysis of consecutive intubations performed by paramedics and flight nurses. Institutional review board approval was obtained at both Brigham and Women’s Hospital and the University of Illinois –Peoria.
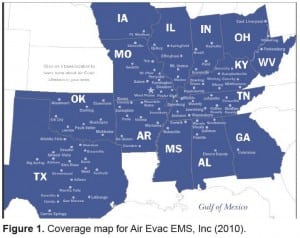
Setting
Intubations were performed by flight personnel within a large air medical company based in the central part of the United States. The company operates 89 206L Long Ranger helicopters flying from 85 bases. The system services more than 1,000 hospitals and records an average of 26,000 flights per year with a combination of inter-facility transfers (60.2%) and on-scene calls (39.8%). Most flight bases are rural, stand-alone structures and are not associated with urban or academic medical centers. Intubations were performed by paramedics and nurses with advanced airway management training. All providers underwent robust quarterly training sessions consisting of seminars on airway assessment, difficult airway management and rapid sequence intubation under the tutelage of regional medical directors. Lectures focused on difficult airway detection, RSI pharmacology and airway management in specific clinical scenarios, such as head injury and shock. Additionally, case-based skills sessions, utilizing METI ECS simulators of differing ages (neonatal, pediatric and adult), were mandatory with special attention placed on straight and curved blade direct laryngoscopic technique, augmentation maneuvers (optimal external laryngeal manipulation) and the use of rescue airways for difficult intubations. Each paramedic and flight nurse had to perform 4 intubations under the supervision of the regional medical director. Airway scenarios were pulled from actual flight logs during which particular airway challenges or hazards were encountered. These scenarios ranged from facial and airway trauma to airway obstruction to airway management in the morbidly obese. During the simulator sessions, providers were tested not only on intubation technique and tube placement but also on correct dosing, timing and application or RSI medications. Extraglottic device and cricothyrotomy (both percutaneous and surgical) techniques were also practiced every 3 months. Paramedics and flight nurses had an average of 12 years of prehospital experience and logged annually more than 25 airway procedures through a combination of field intubations and simulated airway scenarios. Two-thirds of these airway procedures are performed in simulation. Airway management was guided by standard intubation protocols, reviewed and approved annually by the senior medical director. Indications for airway management include failure of oxygenation and ventilation, inadequate airway protection, or airway deterioration during transport. Protocols outlined the indication for pretreatment agents (i.e. lidocaine and fentanyl for head injury with presumed elevated intracranial pressure), use of induction agents and neuromuscular blockers for rapid sequence intubation, and algorithms for crash and failed airway management. Induction agents included etomidate, midazolam and ketamine. Paralytics included succinylcholine, rocuronium and vecuronium. Standard drug doses were used for airway management and are listed in Table 1.
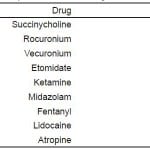
Table 1. Rapid sequence intubation drugs and intravenous doses.
Selection of Participants
We included all adult and pediatric patients who underwent either an intubation attempt or placement of an extraglottic device by any system flight personnel over a 36-month period from 1/1/07 to 12/31/09 in our analysis. Patients intubated by flight crew personnel but not flown (ongoing cardiopulmonary arrests in the field who were taken by ground to the closest local hospital or patients who never ultimately left the original facility) were not included in the database and therefore not analyzed. No significant changes were made to protocols or training during this time.
Methods of Measurement
We categorized each intubated patient as either a medical or trauma intubation based on information provided to dispatchers or gathered on scene. A difficult airway assessment was done, whenever possible, by each operator prior to administration of medication and, if appropriate for neuromuscular blockers, rapid sequence intubation was performed. The operator evaluated mouth opening, cervical spine mobility, mandible and tongue size and location of the thyroid cartilage prior to airway intervention. This approach has been used successfully to predict difficult direct laryngoscopy in emergency department patients14,15 In the absence of significant predicted difficulty, the intubator performed orotracheal rapid sequence intubation by direct laryngoscopy. An extraglottic device (combitube, laryngeal mask airway or King laryngeal tube) was used as the initial airway maneuver if the patient was deemed to be too difficult to safely receive neuromuscular blockade. Extraglottic devices placed as the first planned method of airway control occurred with sedation only. In-flight cardiopulmonary arrests with a crash airway were managed with immediate direct laryngoscopy, without RSI meds, followed by extraglottic device placement if laryngoscopy failed. A failed airway was defined as either a failed intubation attempt in concert with an oxygen saturation below 90% despite maximal supplemental oxygen and assisted ventilations or 3 failed attempts by an experienced operator.14 Failed airways were managed, per protocol, with either a rescue device (combitube, laryngeal mask airway or laryngeal tube), continued bag mask ventilation, or cricothyrotomy. Malleable stylets were used in the endotracheal tubes during intubation and all blunt trauma patients were placed in cervical collars on-scene. Helicopters were not equipped with video larygoscopes. Each patient transport generated a flight record as well as a standardized intubation report that was completed in real time by the operator. Whether an intubation took place is a demand function on the electronic flight record and cannot be bypassed. Recorded variables included the patient age, sex, estimated weight, flight classification, protocol and drugs used, initial airway management maneuver, number of intubation attempts, intubation success, and use of rescue devices. During the registry period, an intubation attempt was defined as insertion of any laryngoscope blade with passage of an endotracheal tube beyond the patient’s lips. Confirmation of endotracheal tube placement was done by auscultation and colorimetric end-tidal CO2 detection. Capnography was used during transport. Successful endotracheal intubation was defined by tube passage resulting in chest rise, and color change on a colorimetric end-tidal CO2 detector. Vitals signs were noted to be “stable” or “unstable” both before and after intubation but specific values were not contained in the database. Intubation reports were monitored for completeness by regional medical directors with a reporting compliance of 100%.
Data Collection and Processing
After each flight, operators recorded flight and intubation data onto a structured data form. Data were reviewed for completeness and entered by the medical director and nurse educator into the company’s main database (SQL database, Microsoft AccessTM, Redmond, WA). We then imported the data into a spreadsheet (Microsoft Excel™, Redmond, WA) for analysis. Structured queries were performed to retrieve data relevant to primary and secondary endpoints.
Primary Data Analysis
We present descriptive data with 95% confidence intervals (95% CI) where appropriate and binary comparisons using chi square test. Analysis was completed using SAS 9.13 (SAS Institute, Cary, NC).
RESULTS
During the review period, 4,916 intubations were recorded into the database. Forty-five intubations were not performed by prehospital personnel and were excluded, resulting in 4,871 intubations available for analysis, including 2,186 (44.9%) medical and 2,685 (55.1%) trauma cases. Given the total flight volume, approximately 6% of annual flights required crew members to perform advanced airway procedures during transport. There were 4,390 (90.1%) adult and 256 (5.3%) pediatric (age ≤ 14) intubations with a mean age of 46.1 years. 225 (4.6%) encounters did not have an age recorded. Of these, 3,155 patients (64.8%) were male and 1,716 (35.2%) were female.
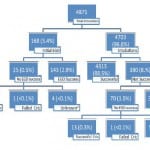
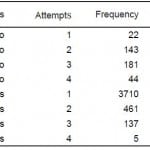
Of 4,871 encounters, 4,703 (96.6%) underwent an orotracheal intubation attempt as the first airway maneuver (Figure 2). First attempt intubation success was 78.9% (n=3710, 95% CI 77.7, 80.0) and ultimate intubation success was 91.7% (n=4313, 95% CI 90.9, 92.5). Of successful intubations, 96.7% (n=4171) were intubated in 2 or fewer attempts and 99.9% (n=4308) in 3 attempts or less. Five patients received a fourth attempt. Overall, the intubation success rate was higher for medical patients than for trauma patients (93.4% versus 90.3%; p=.0001 JT test, Table 2, Table 3).
Figure 2. Breakdown of airway management encounters. CRIC, cricothyrotomy; EGD, extraglottic device.
Table 2. Attempts for successful versus unsuccessful intubations.
For unsuccessful intubations (n=390), 22 (5.6%) had 1 attempt, 143 (36.7%) had 2 attempts, 181 (46.4%) had 3 attempts, and 44 (11.3%) patients had 4 attempts before another management method was performed. Of these patients, 350 (90%) had an attempt at extraglottic device (EGD) placement as the first rescue maneuver which was successful in 320 cases. The King LT was successful 91.6% of the time (207/226 attempts), the combitube was successful 90.1% (100/111 attempts) and the laryngeal mask airway, although used rarely, was successful 100% of the time (13/13). Fourteen patients underwent cricothyrotomy, six as the first rescue method (all of which were successful) and eight after a failed attempt at EGD use, with one failure from the latter group. For the remaining 56 (14.4%) patients, no additional details were recorded although, per protocol, they would have been managed with prolonged bag and mask ventilation.
One hundred sixty-eight (3.4%) of all patients were initially managed with an extraglottic device without an antecedent attempt at endotracheal tube placement. In this group, successful oxygenation with an EGD occurred in 143 (85.1%) and was unsuccessful in 25 (14.9%). Rescue cricothyrotomy was attempted in 21 of the 25 (80%) patients for whom EGD management was unsuccessful, with only one failure. Four cases had no additional details available, although per protocol they would have been mask ventilated until transport was complete. Operators reported no deaths during transport due to a failed airway. Overall, successful oxygenation and ventilation (successful intubation, EGD use or surgical airway) was 98.7% (n=4809, 95%, CI 98.4, 99.0).
DISCUSSION
Air-medical teams often take care of the most severely compromised patients for whom early and decisive airway management may have a direct impact on patient outcome.6, 7 Tracheal intubation, however, is a complex procedure requiring extensive knowledge of airway anatomy, human physiology, pharmacology and various rescue strategies should intubation fail. Even in the simplest of scenarios, intubation represents a high-stakes situation for every patient. Reporting quality care and procedural competency is paramount in this select group of critical-care providers. In this system, which involves specialized training and a skills maintenance program, complemented by protocol-driven practice, airway management with tracheal intubation and selected use of extraglottic devices is performed with high levels of success. Our finding of a 91.7% intubation success rate and a 98.7% oxygenation and ventilation success rate confirms results from smaller studies and suggests these findings may be typical of other air-medical programs. 8–13,15 Additionally, this contributes to our understanding of air-transport airway management competency by evaluating intubation procedures and success, on a large scale, within a private, non-academic program and suggests that high-level airway management is likely ubiquitous with these specialized providers.
Surgical airways were performed at a similar rate and with similar success to prior published reports of pre-hospital cricothyrotomy.16,17 Extraglottic devices were used early and often in our study population, with the King laryngeal tube used most frequently. All EGDs had high rates of placement and successful use suggesting these tools continue to be a helpful adjunct for pre-hospital airway management. The baseline skill set of our operators was high. This particular air transport company provides an extensive airway training program for new employees and maintains skills through quarterly training sessions, all with strict oversight by regional medical directors. It is difficult to gauge the exact impact of this educational regimen on intubation success, although augmenting real-life experience with extensive simulation is unlikely to make their performance worse. We do know that intubation volume (or lack thereof) is linked to performance. Early investigations of out-of-hospital intubation success by ground providers have shown varying results, but as many as 16% of pre-hospital intubations may be unsuccessful.18 Minimal airway management requirements for paramedic certification and skill degradation because of infrequent field intubations have been blamed for these inconsistent results.19,20 Procedural performance is associated with frequent repetition, and paramedics in high volume settings have shown higher rates of intubation success; however, most EMS systems cannot provide high volume procedural exposure.21 One review from Pennsylvania found that endotracheal intubation took place in only 0.7 percent of all patient encounters in 2003. Two-thirds of providers performed 2 or fewer intubations and nearly 40% did not perform any.19 Although a causal relationship cannot be made given the study design, our findings suggest that this group of pre-hospital providers who receive elaborate initial training and ongoing assessments to maintain intubation skill, practicing within a protocol-driven system for uniformity, perform advanced airway management with a high degree of success. While we await equal performance from ground personnel, a trend has developed that shows specially trained air-transport providers have the skills required for safe and effective emergency airway management. Going forward, intubation trends seen in hospital settings should be investigated further in the pre-hospital arena. This includes the integration of video laryngoscopes and optical devices, the refinement of difficult airway protocols and development of pre-intubation checklists. Air transport personnel should continue to be on the vanguard of airway management research.
LIMITATIONS
Our study has some important limitations. First, these intubations were performed by highly skilled paramedics and flight nurses within a high volume air-transport company, predominantly during inter-facility transfers; therefore our results represent what operators with a similar skill set and exposure would likely achieve and may not be generalizable to all pre-hospital providers. Second, self-reported data have intrinsic limitations, and under-reporting of poorly performed intubations including those with multiple failed attempts and adverse events is possible. Close compliance monitoring by regional medical directors and mandatory reporting fields for intubation in the electronic flight record, and a reporting compliance of 100% limits the possibility of selective reporting. Additionally, the structured data form was designed for internal, administrative purposes and was not originally created with a developed research protocol. This has resulted in some non-standard definitions and variables in our data pool. Looking ahead, operational definitions can be clarified during a prospective collection phase. First, the definition used for tracheal intubation attempt required actual attempted insertion of an endotracheal tube, while the most widely accepted definition of intubation attempt simply requires insertion of the laryngoscope blade beyond the teeth. Therefore, our finding that 3.4% of all patients had an EGD device placed as the first airway maneuver may not be exact if some of those patients underwent direct laryngoscopy (without an attempt at tracheal tube placement) first. This may also result in an overestimation of the first attempt success rate found in our sample. However, even if every patient who had an EGD placed was categorized as a first attempt failure, the first attempt success rate remains high. Second, many data points that would have been helpful in refining our results were not collected. Vital signs surrounding intubation were noted to be “stable” or “not stable,” although specific values were not recorded. In addition, it was not specified when, exactly, the intubation took place whether before lift off or in-flight. The latter group would pose unique challenges because of the physical constraints of a small rotorcraft. We are unable to make detailed statements about intubations that took place while in the air.
Drugs used during intubation were documented in the registry as classifications of medications instead of specific agents. In other words when RSI was performed, etomidate or midazolam could have been used in standard doses if the patient was hemodynamically stable. Either drug would have qualified as the “induction” agent for the electronic record; however, the specific drug was not documented. This makes intubation comparisons stratified by particular drugs impossible. Finally, destination tube confirmation was not recorded, and therefore an overestimation of intubation success within our sample is possible.22–25 All tubes, however, were verified with auscultation, chest rise, and colorimetric ETC02 detection. In addition, waveform capnography was a recommended part of the post-intubation care during transport, making the chance of an unrecognized misplaced tube very low. We did not include patients intubated by Air Evac EMS personnel but not flown because of critical instability, ongoing CPR or death in the field included in our analysis since a transport flight record was not generated for these encounters. Certainly, this population had high morbidity and mortality and perhaps some may have died as a result of failed airway management. Not knowing or including this group in our analysis biases our findings towards better performance and may have left out serious airway complications that escaped our surveillance. Approximately 1% of our study population (60 patients) had no recorded successful airway maneuver. It is impossible to know how these encounters ended. Since there were no operator reports of patient death due to a failed airway, one interpretation is that these patients were successfully bag-and-mask ventilated until transport was complete. Another reasonable conclusion is that the lack of information on these encounters means we may be under-reporting deaths due to failed airway management.
This group of advanced-level providers underwent advanced simulation airway training multiple times per year as part of routine competency checks. Although simulation used to augment real-life experience is generally considered beneficial, the effect this extra training has on final performance is difficult to gauge.
Finally, our primary outcome was successful intubation rather than neurologic function or mortality. How these performance characteristics translate to patient survival and function requires further study.
CONCLUSION
In this high volume air transport agency, skilled pre-hospital providers, using rapid sequence intubation protocols, are successful with airway management techniques including tracheal intubation and ventilation with an extraglottic device. Surgical airways are rarely required but likely to be successful when performed. These data may be used to better define attainable performance and training standards for pre-hospital air transport providers responsible for emergency airway management.
Figure. Coverage map for AIR Evac EMS, Inc (2010).
Footnotes
Women’s Hospital, Department of Emergency Medicine, 75 Francis Street, Boston, MA 02115. Email: cabrown@partners.org. 3 / 2014; 15:188 – 193
Submission history: Revision received June 13, 2013; Submitted October 3, 2013; Accepted November 11, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. Dr. Cox is the medical director for Air Evac EMS, Inc.
REFERENCES
1. Davis DP, Hoyt DB, Ochs M, et al. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. J Trauma. 2003;54:444-453.
2. Winchell RJ, Hoyt DB. Endotracheal intubation in the field improves survival in patients with severe head injury. Trauma Research and Education Foundation of San Diego. Arch Surg. 1997;132:592-597.
3. Sloane C, Vilke GM, Chan TC, et al. Rapid sequence intubation in the field versus hospital in trauma patients. J Emerg Med. 2000;19:259-264.
4. Murray JA, Demetriades D, Berne TV, et al. Prehospital intubation in patients with severe head injury. J Trauma. 2000;49:1065-1070.
5. Davis DP, Peay J, Sise MJ, et al. The impact of prehospital endotracheal intubation on outcome in moderate to severe traumatic brain injury. J Trauma. 2005; 58:933-939.
6. Poste JC, Davis DP, Ochs M, et al. Air medical transport of severely head-injured patients undergoing paramedic rapid sequence intubation. Air Med J. 2004; 23:36-40
7. Davis DP, Stern J, Sise MJ, et al. A follow-up analysis of factors associated with head-injury mortality after paramedic rapid sequence intubation. J Trauma. 2005;59:486-490.
8. Lowe L, Sagehorn K, Madsen R. The effect of a rapid sequence induction protocol on intubation success rate in an air medical program. Air Med J. 1998;17:101-104.
9. Germann CA, Baumann MR, Kendall KM, et al. Performance of endotracheal intubation and rescue techniques by emergency services personnel in an air medical service. Prehosp Emerg Care. 2009; 13:44-49.
10. Rose WD, Anderson LD, Edmond SA. Analysis of intubations. Before and after establishment of a rapid sequence intubation protocol for air medical use. Air Med J. 1994;13:475-478.
11. Sing RF, Rotondo MF, Zonies DH, et al. Rapid sequence induction for intubation by an aeromedical transport team: a critical analysis. Am J Emerg Med. 1998; 16:598-602.
12. Murphy-Macabobby M, Marshall WJ, Schneider C, et al. Neuromuscular blockade in aeromedical airway management. Ann Emerg Med. 1992;21:664-668.
13. Ma OJ, Atchley RB, Hatley T, et al. Intubation success rates improve for an air medical program after implementing the use of neuromuscular blocking agents. Am J Emerg Med. 1998; 16:125-127.
14. Walls RM, Murphy MF. Identification of the difficult and failed airway. In: Walls RM and Murphy MF (eds): Manual of Emergency Airway Management, 3rd edition. Philadelphia, Lippincott Williams and Wilkins, 2008;81-93.
15. Reed MJ, Dunn MJG, McKeown DW, et al. Can an airway assessment score predict difficulty at intubation in the emergency department?. Emerg Med J. 2005;22:99-102
16. Thomas S, Judge T, Lowell MJ, et al. Airway management success and hypoxemia rates in air and ground critical care transport: a prospective multicenter study. Prehosp Emerg Care. 2010;14:283.
17 McIntosh SE, Swanson ER, Barton ED. Cricothyrotomy in air medical transport. J Trauma. 2008;64:1543-1547.
18. Robinson KJ, Katz R, Jacobs LM. A 12-year experience with prehospital cricothyrotomies. Air Med J. 2001;20:27-30.
19. Wang HE, Kupas DF, Paris PM, et al. Preliminary experience with a prospective, multi-centered evaluation of out-of-hospital endotracheal intubation. Resuscitation. 2003;58:49-58.
20. Wang HE, Kupas DF, Hostler D, et al. Procedural experience with out-of-hospital endotracheal intubation. Crit Care Med. 2005; 33:1718-1721.
21. Burton JH, Baumann MR, Maoz T, et al. Endotracheal intubation in a rural EMS state: procedure utilization and impact of skills maintenance guidelines. Prehosp Emerg Care. 2003;7:352-356.
22. Warner KJ, Carlbom D, Cooke CR, et al. Paramedic Training for Proficient Prehospital Endotracheal Intubation. Prehosp Emerg Care. 2010;14:103-108.
23. Jones JH, Murphy MP, Dickson RL, et al. Emergency physician-verified out-of-hospital intubation: miss rates by paramedics. Acad Emerg Med. 2004; 11:707-709.
24. Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37:32-37.
25. Jemmett ME, Kendal KM, Fourre MW, et al. Unrecognized misplacement of endotracheal tubes in a mixed urban to rural emergency medical services setting. Acad Emerg Med. 2003; 10:961-965.
26. Colwell CB, McVaney KE, Haukoos JS, et al. An evaluation of out-of-hospital advanced airway management in an urban setting. Acad Emerg Med. 2005;12:417-422.