| Author | Affiliation |
|---|---|
| Daniel J. Pallin, MD, MPH | Department of Emergency Medicine, Brigham and Women’s Hospital, Boston, Massachusetts |
| Carlos A. Camargo, MD, DrPH | Department of Emergency Medicine, Brigham and Women’s Hospital, Boston, Massachusetts |
| Jeremiah D. Schuur, MD, MHS | Department of Emergency Medicine, Brigham and Women’s Hospital, Boston, Massachusetts |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction: National guidelines suggest that most skin abscesses do not require antibiotics, and that cellulitis antibiotics should target streptococci, not community-associated MRSA (CA-MRSA). The objective of this study is to describe antimicrobial treatment of skin infections in U.S. emergency departments (EDs) and analyze potential quality measures.
Methods: The National Hospital Ambulatory Medical Care Survey (NHAMCS) is a 4-stage probability sample of all non-federal U.S. ED visits. In 2007 NHAMCS started recording whether incision and drainage was performed at ED visits. We conducted a retrospective analysis, pooling 2007–2010 data, identified skin infections using diagnostic codes, and identified abscesses by performance of incision and drainage. We generated national estimates and 95% confidence intervals using weighted analyses; quantified frequencies and proportions; and evaluated antibiotic prescribing practices. We evaluated 4 parameters that might serve as quality measures of antibiotic stewardship, and present 2 of them as potentially robust enough for implementation.
Results: Of all ED visits, 3.2% (95% confidence interval 3.1–3.4%) were for skin infection, and 2.7% (2.6–2.9%) were first visits for skin infection, with no increase over time (p=0.80). However, anti-CA-MRSA antibiotic use increased, from 61% (56–66%) to 74% (71–78%) of antibiotic regimens (p<0.001). Twenty-two percent of visits were for abscess, with a non-significant increase (p=0.06). Potential quality measures: Among discharged abscess patients, 87% were prescribed antibiotics (84–90%, overuse). Among antibiotic regimens for abscess patients, 84% included anti-CA-MRSA agents (81–89%, underuse).
Conclusion: From 2007–2010, use of anti-CA-MRSA agents for skin infections increased significantly, despite stable visit frequencies. Antibiotics were over-used for discharged abscess cases, and CA-MRSA-active antibiotics were underused among regimens when antibiotics were used for abscess. [West J Emerg Med. 2014;15(3):282–289.]
INTRODUCTION
Skin infections are among the most common reasons for seeking medical care. Community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) was first described in the mid-1990s. An epidemic of skin infections followed, and emergency department (ED) visits for skin infection nearly tripled from 1993 to 2005. In 2005, skin infections were diagnosed at 3.4 million ED visits and 7.7 million physician office visits in the United States (U.S.).1,2 CA-MRSA became the most common pathogen isolated from purulent skin infections.3
Surveillance has been limited by the absence of large studies capable of differentiating abscess from cellulitis. Most epidemiological studies have relied on diagnostic codes from the International Classification of Diseases, Clinical Modification, 9th Edition (ICD9), which unfortunately groups these 2 conditions within a single category labeled “Cellulitis and Abscess.”1,2 For example, ICD9 code 681 indicates “Cellulitis and abscess of finger, toe, or digit.” In 2007, the National Hospital Ambulatory Medical Care Survey (NHAMCS) started tracking whether incision and drainage (I&D) was performed during an ED visit, allowing us to analyze nationwide antibiotic prescribing practices for abscess and cellulitis separately.
Distinguishing abscess from cellulitis is clinically important because they are treated differently. Evidence-based guidelines recommend that most abscesses be treated with I&D, without antibiotics, and that most cases of cellulitis be treated with antibiotics targeting streptococci, not CA-MRSA.4 The implication is that only a minority of skin infection patients treated as outpatients require coverage for CA-MRSA. Despite this, use of such antibiotics in this group has increased, reaching 38% of all antibiotic regimens among ED patients with skin infection by 2005.1 Overuse of antibiotics is an important public health and quality issue because it causes antimicrobial resistance, and adverse events such as Clostridium difficile colitis.5
We analyzed NHAMCS data from 2007–2010, in order to describe antibiotic use at U.S. ED visits for abscess and cellulitis. We analyze 4 potential measures of quality of care regarding antibiotic use in skin infection cases.
METHODS
We conducted a retrospective analysis of NHAMCS data. NHAMCS is a 4-stage probability-weighted sample of ED visits in all 50 states and the District of Columbia, excluding federal, military, and Veterans Administration hospitals. Its methods have been detailed previously.6 In brief, trained abstractors collect data on structured data entry forms. Data are subsequently validated and cleaned by staff at the Centers for Disease Control (CDC) and by outside consultants. Further details are available in CDC publications.6 Since 2007, a specific data field indicates performance of I&D. Another field indicates whether the visit was the first visit for the complaint or a repeat visit. For this analysis, we pooled ED data from 2007–2010. We included all observations in the database, without exclusions based on age, demographic characteristics or other characteristics.
Skin infection visits were identified by the same ICD9 diagnostic codes used in prior investigations, i.e. cellulitis and abscess of finger (681.00); cellulitis and abscess of toe (681.10); other cellulitis and abscess (682.00–682.99, which includes head, neck, trunk, limbs, and buttocks); cellulitis digit NOS (681.90); felon (681.01); impetigo (684); hidradenitis (705.83); other specified diseases of the hair and hair follicle (i.e. folliculitis, 704.8); neonatal infective mastitis (771.5); nonpurulent mastitis (675.2); breast abscess (675.1); or carbuncle and furuncle (680.00–680.99). We did not include: onychia, dental abscess, Bartholin’s abscess, and pilonidal abscess, following prior investigations.1 If the ED visit was not the first one for the index condition (i.e. was a follow-up visit), we excluded it from analysis. If I&D was performed, we classified the skin infection as an abscess. We classified antibiotics according to whether they were agents typically active against CA-MRSA (trimethoprim-sulfamethoxazole, clindamycin, tetracyclines, rifampin, linezolid, or vancomycin).3 We classified ED disposition as discharged or admitted (to intensive care unit, floor, operating room, observation unit, or to another hospital in transfer), and excluded patients who died in the ED or left before being seen or against medical advice. For individual years, 2007–2010, we report descriptive information on the frequency of visits and antibiotic prescribing practices. We also report the results for all years, stratified by region.
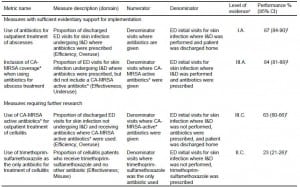
We evaluated 4 potential quality measures: 1) Use of any antibiotic for discharged abscess patients, a measure of overuse.4 2) Non-inclusion of agents with activity against CA-MRSA in antibiotic regimens for abscess patients, a measure of underuse.4 We tested whether this measure would be affected by inclusion of fluoroquinolones in the definition of agents typically active against CA-MRSA, since they often do have such activity and might be chosen due to allergy to other agents, tolerability, desire for co-coverage of Gram-negative bacteria, or for other reasons. 3) Use of CA-MRSA-active agents for discharged cellulitis patients, a measure of overuse. Guidelines suggest that non-purulent cellulitis be treated with agents effective against streptococci, not CA-MRSA, and purulent cellulitis is uncommon.3,4 4) Use of trimethoprim-sulfamethoxazole monotherapy for cellulitis patients, a measure of misuse. This is relevant because there is doubt about this antibiotic’s effectiveness for streptococcal infections.4 We conducted stratified analyses to determine whether any of the following factors were associated with adherence to these measures: age, sex, or geographic region.
We used SAS 9.2 (SAS Institute, Cary, NC) for all analyses, analyzing data using recommended NHAMCS procedures.6 For comparisons of proportions, we report relative risks and their 95% confidence intervals, and χ2 testing. To assess trends over time and adjust for independent variables of interest, we used logistic regression, and report odds ratios and their 95% CIs. This study was exempted from review by our IRB.
RESULTS
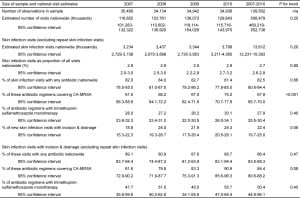
Of all U.S. ED visits during 2007–2010, 3.2% included a diagnosis of skin infection (95% CI 3.1–3.4%). After exclusion of repeat skin infection visits, skin infection was diagnosed at 2.7% of all visits (Table 1). Repeat skin infection visits are excluded from further analyses.
Table 1. Skin infection visits, incision and drainage procedures, and antibiotic use, in United States emergency departments, by year, 2007–2010.
The frequency of skin infection visits relative to all other diagnoses did not change year to year (p=0.80). Among skin infection visits, I&D was noted at 22%, with a non-significant year-to-year increase (p=0.06). Antibiotics were prescribed at 83% of skin infection visits, without year-to-year change (p=0.66). An agent typically active against CA-MRSA was included in 68% of regimens when antibiotics were prescribed. From 2007 to 2010, there was a 13% increase in use of regimens active against CA-MRSA (61% in 2007 versus 74% in 2010, p for trend <0.001). Such an agent was used at 56% (95% confidence interval [CI] 54–58%) of all skin infection visits (as distinct from 68% of antibiotic regimens when antibiotics were prescribed).
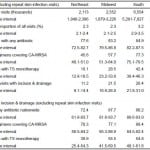
Table 2 shows results by region. All of the nationwide findings described above were accentuated in the South. Skin infections were more common, at 3.2% of all visits, versus 2.3–2.7 in the other regions. I&D was performed at a higher proportion of skin infection visits (26% versus 11–22%), and antibiotics and anti-CA-MRSA antibiotics were used more often. (See Table 2).
Table 2. Skin infection visits, incision and drainage procedures, and antibiotic use, in emergency departments, by United States region, 2007–2010.
CA-MRSA; community-associated methicillin-resistant Staphylococcus aureus; TS, trimethoprim-sulfamethoxazole
*p-values are from chi-squared testing, and assess heterogeneity among the four geographic regions.
Our first quality analysis considered the use of antibiotics among visits with outpatient surgical treatment of abscess. Measure adherence was 13%, because antibiotics were used at 87% of these visits (Table 3). Among the covariates analyzed, this practice varied only by region, with the lowest adherence (i.e. most overuse) in the South, as detailed in Table 2.
Table 3. Proposed quality measures of antibiotic use for skin infections, and performance in United States emergency departments (ED), 2007–2010.
CA-MRSA; community-associated methicillin-resistant Staphylococcus aureus; I&D, incision and drainage
*Antibiotics with CA-MRSA activity are defined here as: trimethoprim-sulfamethoxazole, clindamycin, tetracyclines, rifampin, linezolid, or vancomycin. However, fluoroquinolones often have such activity.
†As measures of overuse or misuse, lower performance is better.
‡As a measure of underuse, a higher proportion is better.
xEvidence grading classification detailed in reference [4]. Letter grades indicate strength of recommendation, with A indicating strong evidence, B indicating moderate evidence, and C indicating poor evidence. Roman numerals indicate quality of evidence, with I indicating ≥1 properly randomized trial, II indicating high-quality controlled observational studies or non-randomized trials, and III indicating expert opinion and case series.
Our second analysis explored the underuse of agents effective against CA-MRSA among antibiotic regimens for abscess visits. As expected, among visits at which at least one antibiotic was prescribed, the probability of an antibiotic regimen containing an agent typically active against CA-MRSA was higher among abscess versus non-abscess visits (relative risk 2.39, 95% CI 1.85–3.08). However, among abscess patients, only 84% of antibiotic regimens included an agent typically active against CA-MRSA (95% CI 81–88%); i.e. nearly 16% of regimens were guideline-non-concordant. When quinolones were included as CA-MRSA-active agents, this percentage was similar, at 86% (95% CI 82–89%). Among the potential covariates, only geographic region demonstrated heterogeneity, with the highest adherence in the South (i.e. least underuse), as detailed in Table 2.
Our third analysis examined the use of CA-MRSA-active regimens among discharged patients with cellulitis, a measure of overuse. Among cellulitis visits, 63% of antibiotic regimens included an agent typically active against CA-MRSA (95% CI 60–65%). This increased from 56% (95% CI 50–61%) in 2007 to 68% (95% CI 63–73%) in 2010 (p=0.008). Among discharged cellulitis cases, 63% of regimens included such an agent (95% CI 60–66%). This was similar among admitted cases (62%, 95% CI 56–68%). Among the potential covariates, only geographic region demonstrated heterogeneity, with the most overuse in the South (Table 2).
In our fourth analysis, we studied monotherapy with trimethoprim-sulfamethoxazole among cellulitis patients. Trimethoprim-sulfamethoxazole was used as the sole antibiotic at 23% of cellulitis visits (95% CI 21–26%), versus 44% of abscess visits (95% CI 39–49%), and in 29% of antibiotic regimens for cellulitis (95% CI 26–31%), versus 50% (95% CI 45–56%) of regimens for abscess. There was no association with patient age. The use of trimethoprim-sulfamethoxazole monotherapy also varied regionally, with the most frequent misuse in the South, as detailed in Table 2.
DISCUSSION
Skin infection was diagnosed at 3.2% of U.S. ED visits during 2007–2010, with no increase during the period. A prior report found that 3.0% of ED visits were for skin infection in 2005.1 This echoes prior findings suggesting that the epidemic may have reached a plateau.7
When we excluded repeat visits from the analysis, we found that skin infection was diagnosed at 2.7% of visits during 2007–2010, without an increase over time. We observed that 22% of new skin infection visits were for abscess (i.e. were treated with I&D). This is consistent with the results of a single-center study which also found that I&D was performed at 22% of skin infection visits.8 Our analysis reveals substantial regional variation in the frequency of skin infection relative to other diagnoses, in the frequency of abscess among skin infection, and the likelihood of use of anti-CA-MRSA antibiotics, with the effects of the CA-MRSA epidemic most apparent in the South (Table 2).
We have presented 4 potential metrics for assessment of quality of care, which we derived from evidence-based guidelines (Table 3).4 We believe that 2 of them, one focusing on overuse and another on underuse, might be appropriate measures for implementation in national quality programs, such as Medicare’s Physician Quality Reporting System.9
Our first proposed measure calculates the proportion of abscess visits ending in discharge at which an antibiotic is used. Multiple studies have shown that routine use of antibiotics for uncomplicated abscesses is not beneficial.4 We suggest implementing this measure by designating as “overuse” any use of antibiotics for abscess treated with I&D and discharged from the ED or clinic, while providing an exception that allows the clinician to specify a reason for antibiotic use (such as immunosuppression, large area of surrounding cellulitis, or area difficult to drain).4 We emphasize that it would never be correct to consider all antibiotic use inappropriate among discharged abscess patients, since there are accepted indications, as listed above. We suggest that this measure of overuse might be valuable as a relative measure, rather than an absolute measure. We found that 87% of discharged abscess patients were treated with antibiotics, suggesting widespread overuse of antibiotics for this common problem. This was most pronounced in the South, at 90%.
Our second potential quality measure assesses failure to use agents active against CA-MRSA when using antibiotics to treat abscess patients. Although antibiotics are usually not indicated in the outpatient treatment of skin abscesses, when antibiotics are used, they should cover CA-MRSA.3,4 We found that nearly 16% of antibiotic regimens prescribed at abscess visits did not include an agent typically active against CA-MRSA. This problem was least common in the South, at 12%. As discussed below, all aspects of performance in the South seem to be directed toward more CA-MRSA coverage, leading to more overuse and less underuse. This is interesting, given our observation that the epidemic appears to be affecting the South disproportionately.
Our third analysis examined use of CA-MRSA-active antibiotics for outpatient treatment of cellulitis. We found that 63% of antibiotic regimens for cellulitis treated on the outpatient basis included an agent typically active against CA-MRSA (Table 3). This is not consistent with current IDSA guidelines, which suggest that non-purulent cellulitis be treated with antibiotics targeting streptococci, not CA-MRSA.4 Purulent cellulitis is uncommon, accounting for only 8% of purulent skin infections.3 Here again, the proper implementation of the quality measure would probably be to view use of anti-CA-MRSA antibiotics as overuse while allowing exceptions (such as failure of prior therapy or presence of purulence).4
This and prior studies reveal that antibiotics targeting CA-MRSA are being used much more frequently, despite lack of evidence and guidelines that recommend otherwise.1,4 Specifically, most cases of abscess do not require antibiotics at all, and most cases of cellulitis should be treated with agents targeting streptococci, not CA-MRSA. We suspect that as clinicians have seen a dramatic rise in the cases of CA-MRSA skin infections (i.e. abscesses), they have assumed that the same organism was responsible for other skin infections (i.e. cellulitis). Additionally, the presence of screening for MRSA carriage and computerized ED dashboards that display a patient’s MRSA status, may lead clinicians to prescribe these antibiotics. However, while this national trend indicates an inappropriate response to the epidemic, there is a problem with applying this criterion to the practice of an individual clinician: clindamycin is a good first-line agent for CA-MRSA-associated infections, and is also a good first-line agent for non-purulent cellulitis, given its coverage of streptococci.4 While many might view a beta lactam as a preferred first-line agent for non-purulent cellulitis, use of clindamycin would not rise to the level of “poor quality” care. Therefore, we consider monitoring of the use of anti-CA-MRSA agents for cellulitis to be a topic of epidemiological interest, but not sufficiently robust for evaluation of the quality of healthcare on a case-by-case basis. It also bears mentioning that providers may be skeptical of the IDSA guidelines’ recommendations for treatment of cellulitis, since they are not based on evidence from clinical trials and since microbiological proof of the etiology of cellulitis is usually impossible to obtain.4,10
Lastly, we analyzed trimethoprim-sulfamethoxazole monotherapy among cellulitis patients as a potential quality measure. The inappropriateness of this practice would lie in the widely held belief that this antibiotic is not effective for streptococcal infections, leading to recommendations that all non-purulent skin infections be covered with beta lactams or other anti-streptococcal agents.4 However, the evidence that this antibiotic is not effective for streptococcal infections is from small clinical trials that were done many years ago, and from in vitro studies that may have been influenced by inappropriately high concentrations of thymidine in culture media.11 One clinical trial that uses trimethoprim-sulfamethoxazole monotherapy for cellulitis is under way, and should shed light on this question (NCT00730028). Pending its publication, it remains prudent to recommend against trimethoprim-sulfamethoxazole monotherapy for streptococcal infections, but we believe that deeming such a practice “poor quality” would be inaccurate, and do not propose this as a quality measure at this time.
In summary, we identified 2 reasonable measures for quality assessment: overuse of antibiotics among abscess patients treated as outpatients with I&D, and use of antibiotic regimens that fail to cover CA-MRSA when using antibiotics for treatment of abscesses. We present the last 2 of our 4 measures as important objects of further study. Evidence for or against the use of anti-CA-MRSA antibiotics in the treatment of cellulitis will come from three ongoing clinical trials (NCT00676130, NCT00729937, NCT00730028).
Our regional analyses reveal interesting patterns of disease occurrence and medical practice. CA-MRSA appears to be causing more abscesses in the South, and prescribers in that region are responding by using more anti-CA-MRSA agents. This includes both more overuse, and less underuse. This may be viewed as a well-intentioned but exaggerated response to the CA-MRSA epidemic. These findings mirror prior analyses of regional variation in appropriateness of antibiotic use in Medicare data, which found evidence of inappropriate use in the South.12
Overall, these results provide clear evidence that the emergence of CA-MRSA continues to have a major impact on prescribing practices for skin infection patients in US EDs, while at the same time providing evidence that the epidemic may have reached a plateau. Before 2001, emergency clinicians almost never used anti-CA-MRSA regimens when treating skin infection patients.1 But by 2005, 38% of antibiotic regimens for these patients included an agent typically active against CA-MRSA, and the current data show that by 2010, 74% of antibiotic regimens for skin infection patients targeted this organism. This dramatic increase is not justified by current evidence or national guidelines.
LIMITATIONS
The main limitations of our study are those common to all NHAMCS investigations.13 Prior research has revealed that when analysis of NHAMCS data provides evidence of errors of omission in medical practice, such evidence should be viewed skeptically, because the data collectors sometimes miss data.14 A case in point is our observation that only 81% of cellulitis patients received antibiotics. We are skeptical about this, and we assume that the true proportions were higher. We can only assume that many of the discharged patients got prescriptions that the NHAMCS data collectors did not see, or sought care after already receiving antibiotics from another provider. With regard to admitted patients, some of them may have received their antibiotics after they were sent from the ED to the ward. On the other hand, NHAMCS data are probably valid when they reveal errors of commission; there is no known mechanism by which errors of commission could erroneously appear.14 All retrospective uncontrolled studies are vulnerable to information bias and other unknown threats to validity.
A limitation particular to our study is use of I&D as a proxy for the diagnosis of abscess. Some procedures may not have been captured, and in some cases patients with cellulitis may have had I&D without identification of pus. Our prior research has suggested that billing data are specific but not sensitive for positive identification of abscesses among all skin infections.8
Our first measure, overuse of antibiotics for discharged abscess patients, is caveated by the fact that in the present investigation we were unable to account for chronic co-morbidities such as diabetes and immunosuppression. While there is no evidence that patients with these conditions benefit from antibiotics for uncomplicated skin abscesses, current guidelines do recommend that they receive antibiotic treatment as an adjunct to I&D.4 Our second measure evaluated failure to include anti-CA-MRSA activity in antibiotic regimens for abscess patients. We found that about 16% of such regimens failed to include such agents. While it is conceivable that some of the 16% were data collection errors, our finding of statistically significant regional diversity, which was consistent with the other regional variations we observed, suggests that the data may be a valid measure of underuse—we can think of no reason that NHAMCS data collectors would be less likely to miss anti-CA-MRSA antibiotics in the South.
CONCLUSION
While ED visit rates for skin infection increased from 1993–2005, this study suggests that the epidemic stabilized during 2007–2010. The CA-MRSA epidemic has prompted major changes in antibiotic choices for these common infections, and use of anti-CA-MRSA agents continues to increase, despite lack of evidence to support their use in this setting. When treating abscesses, clinicians are using antibiotics too much. This is an appropriate target for quality improvement efforts and national quality metrics aimed at antimicrobial stewardship. When they do use antibiotics to treat abscesses, clinicians are often failing to include anti-CA-MRSA antibiotics. This is a reasonable target in efforts to improve care. When treating cellulitis, use of antibiotics effective against CA-MRSA is rising, despite lack of evidence and despite national guidelines. This may be a reasonable target for efforts to promote stewardship, with the caveats given above.
Footnotes
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Supervising Section Editor: Robert Derlet, MD
Address for Correspondence: Daniel Pallin, MD, MPH. Brigham and Women’s Hospital, 75 Francis St. Boston, MA 02215. Email: dpallin@partners.org. 5 / 2014; 15:282 – 289
Submission history: Revision received April 23, 2013; Revision received July 15, 2013; Accepted August 26, 2013
Full text available through open access at http://escholarship.org/uc/uciem_westjem
REFERENCES
1. Pallin DJ, Egan DJ, Pelletier AJ, et al. Increased US emergency department visits for skin and soft tissue infections, and changes in antibiotic choices, during the emergence of community-associated methicillin-resistant Staphylococcus aureus. Ann Emerg Med. 2008;51:291-298.
2. Pallin DJ, Espinola JA, Leung DY, et al. Epidemiology of dermatitis and skin infections in United States physicians’ offices, 1993-2005. Clin Infect Dis. 2009;49:901-907.
3. Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. The N Engl J Med. Aug 17 2006; 355:666-674.
4. Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52:e18-55.
5. Bartlett JG. A call to arms: the imperative for antimicrobial stewardship. Clin Infect Dis. 2011; 53:S4-7.
6. McCaig LF, McLemore T. Plan and operation of the National Hospital Ambulatory Medical Survey. Series 1: programs and collection procedures. Vital Health Stat 1. 1994(34):1-78.
7. Ray GT, Suaya JA, Baxter R. Trends and characteristics of culture-confirmed Staphylococcus aureus infections in a large U.S. integrated health care organization. J Clin Microbiol. 2012; 50(6):1950-1957
8. Qualls ML, Mooney MM, Camargo CA, Jr., et al. Emergency department visit rates for abscess versus other skin infections during the emergence of community-associated methicillin-resistant Staphylococcus aureus, 19972007. Clin Infect Dis. 2012; 55:103-105.
9. Physicain Quality and Reporting System (formely PQRI). Avaliable at: www.outcome.com/pqrs.htm. Accessed December 10, 2012.
10. Swartz MN. Clinical practice. Cellulitis. N Engl J Med. 2004; 350:904-912.
11. Bowen AC, Lilliebridge RA, Tong SY, et al. Is Streptococcus pyogenes Resistant or Susceptible to Trimethoprim-Sulfamethoxazole?. J Clin Microbiol. 2012; 50:4067-4072.
12. Zhang Y, Steinman MA, Kaplan CM. Geographic Variation in Outpatient Antibiotic Prescribing Among Older Adults. Arch Intern Med. 2012;172:1-7.
13. McCaig LF, Burt CW. Understanding and interpreting the national hospital ambulatory medical care survey: key questions and answers. Ann Emerg Med. 2012; 60:716-721
14. Cooper RJ. NHAMCS: Does It Hold Up to Scrutiny?. Ann Emerg Med. 2012;60:722-725