| Author | Affiliation |
|---|---|
| Sheryl M. Strasser, PhD, MPH | Georgia State University, School of Public Health, Atlanta, Georgia |
| Megan Smith, MPH | Georgia State University, School of Public Health, Atlanta, Georgia |
| Scott Weaver, PhD | Georgia State University, School of Public Health, Atlanta, Georgia |
| Shimin Zheng, PhD | East Tennessee State University, College of Public Health, Johnson City, Tennessee |
| Yan Cao, PhD, MS | East Tennessee State University, College of Public Health, Johnson City, Tennessee |
Introduction Methods Results Discussion Conclusion
ABSTRACT
Introduction: The aging population is a rapidly growing demographic in the United States. Isolation, limited autonomy, and declining physical and mental health render many older adults vulnerable to elder mistreatment (EM). The purpose of this study was to assess the prevalence and correlates of EM among a sample of older adults using legal assistance services in Atlanta, Georgia.
Methods: Researchers administered surveys to consenting older adults (aged 60+) in 5 metro Atlanta community centers that hosted legal assistance information sessions as part of the Elderly Legal Assistance Program. The surveys screened for risk factors and prevalence of EM risk using valid and reliable measures and included additional questions regarding demographics characteristics and healthcare use behaviors.
Results: Surveys were completed by 112 participants. Findings reveal that 32 (28.6%) respondents met the criteria for elder abuse / neglect risk; 17 (15.2%) respondents met criteria for depression; and 105 (93.7%) had visited a healthcare provider during the past 6 months.
Conclusion: The rates of EM risk in this sample were higher than those previously reported in research. Findings support continued examination of unique risks that may be present among older adults who may be possibly facing legal issues. Additionally, the reported frequency of healthcare visits among participants reveals a promising opportunity to examine development of a more widespread EM screening approach to be conducted in non-emergency settings. Interdisciplinary collaboration is required to inform screening approaches that account for complexities that EM cases present.
INTRODUCTION
The aging population in America is rapidly increasing. In 2010, an estimated 40 million Americans, or 13%, were age 65 and older.1 Projections indicate that by year 2050, the aged population will more than double to 88.5 million people, or approximately 20% of the population.1 This growth can be attributed to the aging of the large “baby-boomer” generation and improvements in medical technology that have contributed to extending the average lifespan.2,3 As the elderly population increases, so too will the number of people living with chronic illnesses and other risk factors for preventable injury.
One form of preventable injury is elder mistreatment (EM). Estimates of the prevalence of EM range from 4% to 10% in the United States (U.S.), although it is widely accepted that the number of cases reported to Adult Protective Services (APS) is representative of only a small proportion of elders suffering various forms of mistreatment.4 A recent survey of a national sample of community-dwelling, cognitively intact adults aged 60 and older estimates the 1-year prevalence of physical, sexual, and emotional abuse, financial mistreatment, and neglect to be 11.4%.5 Importantly, research has also demonstrated an association between EM and emergency department visits, hospitalization, nursing home placement, and premature mortality.6–8
The spectrum of EM (identified as physical, sexual and psychological abuse, as well as neglect and financial exploitation) has been defined by the National Research Council as “intentional actions that cause harm or create a serious risk of harm (whether or not harm is intended) to a vulnerable elder by a caregiver or other person who stands in a trusting relationship to the elder; or failure of a caregiver to satisfy the elder’s basic needs or protect the elder from harm.”9 Researchers have dedicated numerous studies to the examination of risk factors associated with EM. The risks for EM have been classified as demographic, physical and mental health, social relationships, as well as having a history of abuse. Risk factors for elder abuse have been identified as older age, co-habitation, cognitive impairment/illness, depression and social isolation.10–15
Depression is an especially important risk factor for EM. Symptoms of depression likely will not be overtly disclosed by older adults without direct assessment, as there is a strong stigma associated with mental health issues.14 Further exacerbating this issue is the widespread social norm of ageism, which upholds that depression is natural at the end of life, among the younger adult generations.16 Often older people themselves think depression is a natural part of aging and is due to other common physical and social hardships that often accompany aging.17 Depression is not a normal symptom of aging, and studies show that depression that initially appears later in life is linked to a more chronic course of illness.18,19
Although screening for depression typically takes place in a clinical setting, research has demonstrated that community screenings are also feasible and appropriate. In a study conducted by Schonfeld et al20a community-based screening and brief intervention among older adult substance users demonstrated that non-clinical research staff were able to administer a range of screens, including measures of mental health and suicidal risk. Additionally, the Harvard National Depression Screening Day Scale (HANDS) instrument used in this EM study was previously found to be effective in assessing depression among people using a community pharmacy.21
The purpose of this pilot study was to use valid and reliable screens to estimate the prevalence of EM and depression among older adults using legal assistance services provided by an urban Elder Legal Assistance Program (ELAP) and to identify risk factors associated with EM among this population. The ELAP program is required by federal law, funded primarily by the Older Americans Act and provides adults aged 60 and over with legal representation, information and education in civil legal matters. The program does not base eligibility on a person’s income or resources; however, federal law requires that the program direct services to those persons 60 years of age and older who are in the greatest social and/or economic need, limited English-speaking persons, rural or low income minorities.22
According to data from FY 2009, the majority of persons served by the ELAP program in the metropolitan Atlanta area (n=698) were black or African American (n=497) or white (n=168). Less than 1% of program participants identified as being Hispanic/Latino or belonging to another race. Of those served, 540 persons were categorized by the program as having an economic need and 203 were categorized as frail or having social need.23
Given the vulnerability of the population served by ELAP, there is reason to suspect that the prevalence of EM may be higher among this population. Further, older adults seeking legal assistance may have a higher prevalence of EM, given that EM may be a reason for seeking legal assistance among this population. Depression among those seeking legal advice may also be higher due to stressors and possibly perceived hopelessness faced by those seeking assistance.
We based the conceptual model for exploring risk factors related to EM involved in this study on the Rose and Killien’s Risk and Vulnerability Model24 as applied to elder abuse by Frost and Willette.25Vulnerability relates to characteristics of the elder. Items related to vulnerability include age, gender, and the depression scale. Risk refers to hazards or stressors external to the older adult—which is measured by co-habitation. This approach encompasses the major defining theories for causation for elder violence.
METHODS
The pilot study used a cross-sectional survey design. Study subjects were recruited from 5 community centers offering legal assistance information presentations to older adults by representatives of the State of Georgia’s Elderly Legal Assistance Program (ELAP) within metro Atlanta over the course of 9 weeks. To enroll the maximum number of participants, eligibility requirements were broad. Study subjects had to be English speaking and at least 60 years of age. This study was reviewed and approved by the university institutional review board of the principal investigator. No incentives were offered for participation.
The questionnaire consisted of measures for depression and EM. We selected HANDS, a 13-item validated screening tool, for its brevity, ease of administration, and sensitivity for major depression and suicide.26
Research has also demonstrated that the HANDS instrument is reliable in a community setting.21 We used the Hwalek-Sengstock Elder Abuse Screening Test (HS-EAST) to identify indications of EM. The HS-EAST is a 15-item instrument containing questions that indicate 3 distinct domains: violation of personal rights or direct abuse, characteristics of vulnerability and potentially abusive situations.27Scores of 3 or higher on the HS-EAST have been shown to be indicative of abuse, neglect and exploitation risk when compared to the non-abused comparison group.27 The HS-EAST is recognized among EM researchers as a valid screening instrument.28,29
Demographic data collected included race, ethnicity, age, gender, marital status, educational attainment, occupational status and living arrangements (living alone vs. cohabitation). Additional information was collected regarding the number of medical and mental health visits in the past 6 months. Study participants were given the option of completing a paper-based or computer-based survey.
We ran descriptive statistics to obtain study sample characteristics. For the purpose of analysis, we recoded the following variables as dichotomous, categorical variables: marital status (married or living with partner v. single), race (white v. another race), employment status (works outside the home v. does not work outside the home), EM (yes v. no) and depression (yes v. no).
We categorized study participants who scored 3 or above on the HS-EAST scale as having a positive screen for EM, while respondents that scored a 9 or above on the HANDS scale were categorized as being depressed. We created the following age categories using continuous data: 60–69, 70–79, 80–89, and 90 or above. Imputation was used to replace missing observations.
We performed chi-square and both univariate and multivariate regression analyses to estimate and test the association between EM and the following covariates: gender, age, race, ethnicity, employment status, cohabitation, depression, number of visits to a healthcare provider in the past 6 months and number of visits to a mental health care provider in the past 6 months.
RESULTS
One hundred and twelve individuals 60 years of age or older, English speaking and attending elderly legal assistance information presentations at metro-Atlanta community centers provided written, signed consent and enrolled in the study. Seventy respondents (62.5%) completed computer-based surveys. The majority of respondents, (n=76, 67.9%) were female, white (n=81, 72.3%), and between the ages of 60 and 79 (n=83, 74.1%). Slightly over half of the sample (n=61, 54.5%) had a high school education or less. Ninety-three respondents (83%) were not employed. More respondents were single (n=60, 60.7%) and reported living with someone else (n=69, 61.2%). Over 16 % (n=17) of the study sample met criteria for depression and 32 (31.1%) met criteria for EM. Table 1 presents the complete demographic profile of the sample.

The majority of participants reported seeing a healthcare provider between 1 and 3 times within the past 6 months (60.7 %). Nearly 22% reported visiting a healthcare provider 4 to 6 times, 11.2%reported visiting a healthcare provider more than 6 times, while 6.5% of participants reported never having visited a healthcare provider within the past 6 months. The large majority of participants reported never having visited a mental health provider within the past 6 months (93.4%), while 6.6% reported having visited a mental health provider between 1 and 3 times within the past 6 months.
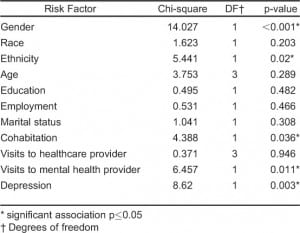
We analyzed the following demographic and risk variables using chi-square to test the association between EM and each of the following variables: sex, race, ethnicity, education, age, employment status, marital status, cohabitation, depression, number of visits to a healthcare provider (physician or nurse practitioner) in the past 6 months and number of visits to a mental healthcare provider (psychiatrist, psychologist or therapist) in the past 6 months. We detected no significant associations between EM and age, marital status, race, employment status, education, or visits to a healthcare provider in the past 6 months.
However, results indicated a significant association between EM and sex, ethnicity, cohabitation and number of visits to a mental health provider (Table 2). A higher proportion of men (56.3% or 18 of 32) met the criteria for EM as compared to women (19.1% or 13 of 68), X2 (1, 100)=14.027, p< 0.001, and of the 5 respondents identifying as Hispanic/Latino, 4 (80%) met the criteria for EM, as compared to 24 of 81 (29.6%) of non-Hispanic/Latino subjects [X2 (1, 86)=5.441, p=0.020]. Nearly half (48.3% or 14 of 29) of those who met EM criteria reported living with another person [X2 (1, 97)=4.388, p=0.036]. Additionally, among the 29 respondents who had a positive screen for EM, 5 (17.2%), reported having had 1–3 visits to a mental health provider within the past 6 months, as compared to 2.9% (2 of 70) of respondents who did not meet criteria for abuse [X2 (1, 99)=6.457, p=0.011].
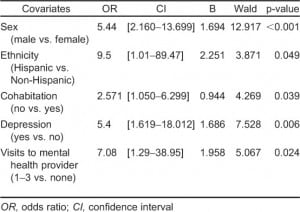
We performed univariate logistic regression for those variables that demonstrated statistically significant associations (p ≤ 0.05) with the independent variable, EM. Results (Table 3) indicate that men in this population were 5 times as likely as women to suffer from or be at risk for EM. Respondents who lived with another person, whether he/she were a spouse, other family member or non-relative were more than twice as likely to suffer or be at risk for abuse/neglect. Depression and number of visits to a mental health provider also increased one’s risk of EM.
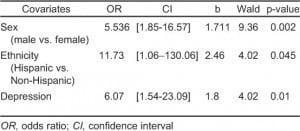
Lastly, we performed multiple logistic regression analysis, which included those variables that remained significant in the univariate regression analyses: sex, ethnicity, cohabitation, depression and visits to a mental health provider. Using this regression model, cohabitation and visits to a mental health provider were not found to be significant predictors of EM. The final multiple logistic regression model included 3 predictors—sex, ethnicity and depression. Males were 5.5 times more likely to meet have a positive screen for EM than females (odds ratio [OR]: 5.54, confidence interval [CI]: 1.85–16.57, p=0.002), and Hispanic respondents were 11.7 times more likely to have a positive EM screen than their non-Hispanic counterparts (OR: 11.73, CI: 1.06–130.06, p=0.045). Depressed respondents were 6 times more likely to have a positive EM screen than their non-depressed peers (OR: 6.07, CI: 1.54–23.09, p=0.01). Results are presented in Table 4.
DISCUSSION
In this cross-sectional survey of older adults attending legal assistance presentations, we found that nearly one-third of our sample met criteria for EM, which is higher than more modest estimates in the general U.S. population ranging from 4–11%.4,5 However, this result serves to confirm our hypothesis that older adults seeking legal services may have a higher prevalence of EM either because EM has led them to seek legal advice or their legal situation has contributed to their vulnerability and put them at greater risk for EM.
Study findings were also different from EM literature concerning demographic risk factors. While other studies indicate that older elderly people are at a greater risk of or abuse and neglect than the younger old, no differentiation of EM by age was found in this sample.10,33 Further, men in this study sample were over 5 times more likely to meet EM criteria than females. While other studies have indicated women are at a greater risk of abuse than men,8,34 Pillemer and Finkelhor13 found that men in their random survey study were more likely to be victims of EM.
Other research has indicated that poorer physical and mental health may put elderly at risk;33 however, our findings indicated that mental health and not physical health was a predictor of EM/EM risk. Depression, and other mental health issues, as implied by the number of visits to a mental health provider in the past 6 months in this study, as well as cohabitation have all been identified as risk factors in the literature. While depression was a significant predictor of EM/EM risk in this study, neither visits to a mental health provider or cohabitation were found to predict EM/EM risk in the multivariate analyses.
We also found that Hispanics/Latinos in this study were substantially more likely than non-Hispanics to meet EM criteria. Examination of EM within Hispanic/Latino communities in the U.S. is gaining attention. In a recent study by DeLiema et al35 in a randomized community sample of 200 Latinos in Los Angeles, 2 out of 5 older adult Latinos reported abuse in the last year, and among those, 22% of the abuse was categorized as “severe,” While the number of Hispanics/Latinos respondents included in this study was very small, this finding highlights the need to further investigate unique interpersonal dynamics and risk factors for EM that may exist in this subpopulation. Because Hispanic/Latino older adults have historically been underrepresented in EM research, explanations for this significant disparity are not readily available.
The differences in our study findings may be due to several factors. First, this study used the HS-EAST instrument, which is not widely used in EM-prevalence studies. Because the instrument was developed for administration by non-clinical professionals, the domains and items may not reflect highly specific measures of EM and thus, there is a potential for overestimation of EM risk. The high prevalence among this sample may also be attributed to the unique circumstances of the study setting. Older adults attending legal presentations may be different than the general older adult population. For these individuals, there may be underlying legal stressors that may lead to strained personal situations, mental distress, depression, and ultimately, violent relationships. The cumulative burden of these stressors may likely place this vulnerable population segment at risk for being the target of abuse by someone who perceives the pending legal matters as “hopeless,” Older adults who are receiving legal services may be in a help-seeking mode; therefore, they are reaching out for services that potentially could assist in address legal problems they face.
Overall, our study findings highlight the need for more robust, sophisticated research that can examine issues related to EM among community-dwelling older adults who may be facing legal issues. The legal circumstances in which clients seek ELAP services may offer an explanation for our high rates of EM/EM risk and depression. Since the prevalence of those who were depressed was much higher than those visiting mental health providers, it is likely that many in the study population needed but were not receiving treatment for depression and therefore at a greater risk for EM.
LIMITATIONS
This study was based on a small and homogenous sample and was further limited by the voluntary nature of the survey; therefore, the answers provided by the respondents may not be indicative of the non-respondents. The results from this study are not generalizable to other older adults who may be seeking legal advice or assistance as a convenience sampling methodology was employed. Additionally, while findings indicate a number of statistically significant associations, temporal ordering is not possible due to the cross-sectional nature of data collected. Additionally, this study used proxy measures for physical and mental health status, number of visits to a healthcare provider and number of visits to a mental health provider. While it stands to reason that high healthcare utilization would be associated with poorer health among older adults, and there is research to support this,36 using healthcare visits as proxy measures does not take into account older adults who may be in need of, but not receiving healthcare for physical or mental health issues. Finally, this study captured respondents’ self-reported answers, not actual behaviors or occurrences of EM. Nonetheless, these findings provide insight into avenues for future research that probes EM risks more profoundly.
CONCLUSION
Elder mistreatment is complex and continued research that advances our understanding of risk factors is essential for prevention efforts. More collaboration among professionals from diverse disciplines who play a role in EM identification and resolution is needed. Professionals trained in law, criminal justice, social services, and mental health may potentially be involved in EM case detection, management, and resolution.36–42 Traditionally the responsibility for recognizing, identifying, and responding to EM has been assumed primarily by healthcare professionals. Jones et al43 determined that the majority of cases are detected by clinicians during urgent care visits. However, through effective screening, EM may be detected before it escalates to a need for emergency medical attention.
The early detection of EM relies heavily on professionals who may interact with older adults earlier than those in urgent healthcare settings, such as primary care physicians, social workers, bankers, lawyers, mental health professionals, and law enforcement. Professionals on the frontline of initial case reporting must receive adequate training to improve identification of signs and symptoms of EM. Enhanced screening and professional collaborations can flourish when EM policies are responsive to scientific evidence that reveal individual-level vulnerabilities and external risk factors for violence.
Given the exponentially growing older adult segment of the United States, the number of adults who may become victims of violence will likely increase until more sensitive, widespread screening is developed and implemented. Progressive national policies responsive to these trends can foster guidelines and screening practices that proactively prepare professionals to identify older adults most at risk for EM. Professionals practicing in the community, such as law enforcement, social services, law, and banking among others, may provide important early screening for EM risks that are frequently associated with victimization. Enhancing the recognition and collaborative partnerships among professionals provide a promising structure (opportunity) for resolving increasingly difficult situations for older adults.
Footnotes
Supervising Section Editor: Monica H. Swahn, PhD, MPH
Submission history: Submitted December 12, 2012; Revision received February 18, 2013; Accepted February 26, 2013
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2013.2.15640
Address for Correspondence: Sheryl M. Strasser, PhD, MPH, MSW, MCHES, School of Public Health, Georgia State University, 140 Decatur Street, Room 847, Atlanta, GA 30303. E-mail: sstrasser@gsu.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Vincent GK, Velkoff V. The next four decades: the older population in the United States 2010 to 2050. Available at: http://www.census.gov/prod/2010pubs/p25-1138.pdf. Accessed January 11, 2010.
2. Daichman LS, Aguas S, Spencer C. Elder abuse. In: Heggenhougen K, Quah S, editors. International Encyclopedia of Public Health. Vol 2. San Diego: Academic Press; 2008. pp. 310–315.
3. Dauenhauer JA, Mayer KC, Mason A. Evaluation of adult protective services: perspectives of community professionals. J Elder Abuse Negl. 2007;19:41–57. [PubMed]
4. Taylor DK, Bachuwa G, Evans J, Jackson-Johnson V. Assessing barriers to the identification of elder abuse and neglect: a communitywide survey of primary care physicians. J Natl Med Assoc.2006;98(3):403–4. [PMC free article] [PubMed]
5. Acierno R, Hernandez MA, Amstadter AB, Resnick HS, Steve K, Muzzy W, Kilpatrick DG. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the national elder mistreatment study. Am J Public Health. 2010;100(2):292–297.[PMC free article] [PubMed]
6. Cooper C, Selwood A, Livingston G. The prevalence of elder abuse and neglect: a systematic review.Age Ageing. 2008;37(2):151–160. [PubMed]
7. Bonnie RJ, Wallace RB. Elder Mistreatment: Abuse, Neglect, and Exploitation in an Aging America. National Research Council (US) Panel to Review Risk and Prevalence of Elder Abuse and Neglect.Washington (DC): National Academies Press (US); 2003. [PubMed]
8. Dunlop BD, Rothman MB, Condon KM. et al. Elder abuse: risk factors and use of case data to improve policy and practice. J Elder Abuse Negl. 2001;12(3):95.
9. Pillemer K, Finkelhor D. The prevalence of elder abuse: a random sample survey. Gerontologist.1988;28(1):51–57. [PubMed]
10. Dyer CB, Pavlik VN, Murphy KP, Hyman DJ. The high prevalence of depression and dementia in elder abuse or neglect. J Am Geriatr Soc. 2000;48(2):205–208. [PubMed]
11. Pillemer K, Finkelhor D. Causes of elder abuse: caregiver stress versus problem relatives. Am J Orthopsychiatry. 1989;59(2):179–187. [PubMed]
12. Alexopoulos GS, Bruce ML, Hull J. et al. Clinical determinants of suicidal ideation and behavior in geriatric depression. Arch. Gen. Psychiatry. 1999;56(11):1048–1053. [PubMed]
13. Lachs MS, Williams C, O’Brien S, Hurst L, Horwitz R. Risk factors for reported elder abuse and neglect: a nine-year observational cohort study. Gerontologist. 1997;37(4):469–474. [PubMed]
14. Choi NG, Jun J. Life regrets and pride among low-income older adults: relationships with depressive symptoms, current life stressors and coping resources. Aging Ment Health. 2009;13:213–225. [PubMed]
15. Centers for Disease Control and Prevention. Healthy aging: depression is not a normal part of growing older. Available at: http://www.cdc.gov/aging/mentalhealth/depression.htm. Accessed January11, 2010.
16. Feldman EL, Jaffe A, Galambos N. et al. Clinical practice guidelines on depression: awareness, attitudes, and content knowledge among family physicians in New York. Arch Fam Med. 1998;7(1):58–62. [PubMed]
17. Lebowitz BD. Diagnosis and treatment of depression in late life. Consensus statement update. J Amer Med Assoc. 1997;278(14):1186–1190. [PubMed]
18. Schonfeld L, King-Kallimanis BL, Duchene DM. et al. Screening and brief intervention for substance misuse among older adults: the Florida BRITE project. Am J Public Health. 2010;100(1):108–114.[PMC free article] [PubMed]
19. Rose MH, Killien M. Risk and vulnerability: a case for differentiation. Adv Nurs Sci. 1983;5(3):60–73. [PubMed]
20. Frost MH, Willette K. Risk for abuse/neglect: documentation of assessment data and diagnoses. J Gerontol Nurs. 1994;20(8):37–45. [PubMed]
21. Baer L, Jacobs DG, Meszler-Reizes J. et al. Development of a brief screening instrument: the HANDS. Psychother Psychosom. 2000;69(1):35–41. [PubMed]
22. Neale AV, Hwalek MA, Scott RO. et al. Validation of the Hwalek-Sengstock elder abuse screening test. J Appl Gerontol. 1991;10(4):406–418.
23. Daly JM, Jogerst GJ. Readability and content of elder abuse instruments. J Elder Abuse Negl.2005;17(4):31–52. [PubMed]
24. Fulmer T, Guadagno L, Bitondo Dyer C. et al. Progress in elder abuse screening and assessment instruments. J Am Geriatr Soc. 2004;52(2):297–304. [PubMed]
25. Comijs HC, Pot AM, Smit JH. et al. Elder abuse in the community: prevalence and consequences. J Am Geriatr Soc. 1998;46:885–888. [PubMed]
26. Ogg J, Bennett G. Elder abuse in Britain. BMJ. 1992;305:988–989.
27. Podnieks E. National survey on abuse of the elderly in Canada. J Elder Abuse Negl. 1992;4:5–58.
28. Gorbien MJ, Eisenstein AR. Elder abuse and neglect: an overview. Geriatr Med. 2005;21:279–292.[PubMed]
29. Comijs HC, Smit JH, Pot AM. et al. Risk indicators of elder mistreatment in the community. J Elder Abuse Negl. 1998;9:67–76.
30. World Health Organization. Abuse of the elderly. Available at:http://www.who.int/violence_injury_prevention/violence/global_campaign/en/elderabusefacts.pdf. Accessed December 11, 2012.
31. DeLiema M, Gassoumis ZD, Homeier DC. et al. Determining Prevalence and correlates of elder abuse using promotores: low-income immigrant Latinos report high rates of abuse and neglect. J Amer Geriatr Soc. 2012;60(7):1333–1339. [PMC free article] [PubMed]
32. Ciccarello MJ. Recent legal trends affecting your older patients. Clin Obstet Gynecol. 2007;50:790–799. [PubMed]
33. Choi NG, Mayer J. Elder abuse, neglect, and exploitation. J Gerontol Soc Work. 2000;33:5–25.
34. Lachs MS, Pillemer K. Elder abuse. Lancet. 2004;364:1263–1272. [PubMed]
35. Payne BK. Crime and elder abuse: an integrated perspective. Springfield, IL: Charles C Thomas; 2005.
36. Strasser SM, Kerr J, King P. et al. A survey of Georgia adult protective service staff: implications for older adult injury prevention and policy. West J Emerg Med. 2011;12(3):357–364. [PMC free article][PubMed]
37. Strasser S, O’Quin K, Price T. et al. Older adults with intellectual disabilities: targets for increasing victimization, a call for a preemptive screening policy. J Ment Health Res Intellect Disabil.2012;5(2):157–167.
38. Jones J, Dougherty JD, Schelbie D. et al. Emergency department protocol for the diagnosis and evaluation of geriatric abuse. Ann Emerg Med. 1998;17:1006–1015. [PubMed]


