| Author | Affiliation |
|---|---|
| Abigail Hankin, MD, MPH | Emory University, Department of Emergency Medicine, Atlanta, Georgia |
| Brittany Meagley, MD, MPH | Emory University, Rollins School of Public Health, Department of Health Policy and Management, Atlanta, Georgia |
| Stanley C. Wei, MD, MPH | St. Joseph’s Mercy Care Services, Atlanta, Georgia |
| Debra Houry, MD, MPH | Emory University, Department of Emergency Medicine, Atlanta, Georgia |
Introduction Methods Results Discussion Conclusion
ABSTRACT
Introduction: To assess the prevalence of risk factors for violent injury among young adults treated at an urban emergency department (ED).
Methods: This study is a cross-sectional analysis of data collected as part of a longitudinal study. Enrollment took place in an urban ED in a Level 1 trauma center, June through December 2010. All patients aged 18–24 years were eligible. Patients were excluded if they were incarcerated, critically ill, or unable to read English. Study participants completed a 10-minute multiple-choice questionnaire using previously validated scales: a) aggression, b) perceived likelihood of violence, c) recent violent behavior, d) peer behavior, and e) community exposure to violence.
Results: 403 eligible patients were approached, of whom 365 (90.1%) consented to participate. Average age was 21.1 (95% confidence interval: 20.9, 21.3) years, and participants were 57.2% female, 85.7% African American, and 82.2% were educated at the high school level or beyond. Among study participants, rates of high-risk exposure to individual risk factors ranged from 7.4% (recent violent behavior) to 24.5% (exposure to community violence), with 32.3% of patients showing high exposure to at least one risk factor. When comparing participants by ethnicity, no significant differences were found between White, African-American, and Hispanic participants. Males and females differed significantly only on 1 of the scales – community violence, (20.4% of males vs. 30.3% of females, p= 0.03). Self-reported hostile/aggressive feelings were independently associated with initial presentation for injury-associated complaint after controlling for age, sex, and race (odds ratio 3.48 (1.49–8.13).
Conclusion: Over 30% of young adults presenting to an urban ED reported high exposure to risk factors for violent injury. The high prevalence of these risk factors among ED patients highlights the potential benefit of a survey instrument to identify youth who might benefit from a targeted, ED-based violence prevention program.
INTRODUCTION
Injuries account for the majority of childhood injuries and deaths in the United States (U.S.), with homicide and suicide ranked as the second and third leading cause of death, respectively, among adolescents aged 15–19.1 Furthermore, injuries from interpersonal assaults in this age group accounted for 656,000 visits to U.S. emergency departments (EDs) in 2008.2 Non-fatal violent injuries in adolescents often precede fatal violence and homicide, making this a pressing public health concern for research and prevention initiatives.3,4
Previous research has identified risk factors that are associated with risk for violent injury among adolescents and young adults. These risk factors include low academic performance, peer delinquency, and availability of drugs in a neighborhood, as well as witnessing or being the victim of an act of violence, a history of violent injury, and a history of physical fighting.5,6 Among boys, a history of illicit drug use predicted violent injury, whereas among girls, a history of depressive symptoms was predictive.6
As both a societal safety net and a healthcare provider to those with limited resources, many behavioral scientists have highlighted the potential of the ED as a site for screening for health risks and initiating prevention programs.7 The ED has been used as a site for primary and secondary prevention strategies for health-related behavioral risks ranging from intimate partner violence to substance abuse.8,9 With respect to youth violence, prior studies have found that ED-based violence prevention can be an effective method of secondary prevention among previously-injured youth.10
To realize the potential of the ED as a site for primary prevention efforts, it is important to target research and prevention at youth who are at risk, rather focusing on youth who have been the victims of violent injury. Currently, there is a dearth of research assessing the prevalence of risk factors for violent injury among all young adults visiting the ED, or the relationship between these risk factors and risk for future ED visits for injury.
In this study, we sought to identify the prevalence of risk factors for violent injury among young adults presenting to an urban, inner-city ED, as well as the association between risk factor exposure and gender, age, ethnicity, and presentation for injury vs. non-injury complaint. By assessing the prevalence of these risk factors across all youth presenting to the ED, this study can provide a picture of the burden of risk for violent injury among young patients in the ED.
METHODS
Study Design
We conducted a cross-sectional survey of patients aged 18–24, presenting to the ED over a 7-month period. This study was approved by our university institutional review board and the hospital research oversight committee.
Setting
The ED is in an inner-city academic hospital predominantly serving a minority (88% African- American), indigent population. The ED serves over 100,000 patients annually.
Study Protocol
Participants were enrolled by research assistants, including both departmental research assistants (RA) and a dedicated study research assistant. Both the departmental RAs and the study RA were specially trained in recruiting and consenting patients for ED-based research, and had specialized training in ED patient recruitment, study ethics, and informed consent procedures. The RAs were present in the ED for 8-hour shifts, with shift day and time varying to include weekend days, as well as weekdays, and day shifts as well as evening shifts.
Any patient between the ages of 18–24, regardless of presenting complaint, was eligible for participation. We excluded participants if they were critically ill, incarcerated, had a psychiatric emergency, or if they were unable to read English. All eligible patients were approached for participation in the study. Potential participants were asked to participate in a study about health and health behaviors among young adults, and were asked whether they would be willing to complete a written survey requiring approximately 10 minutes of their time. If participants were in the waiting room when approached, they were taken to a private area to complete the survey. If participants were in treatment rooms, RAs endeavored to identify periods during the ED course when the patient would not be interrupted for the duration of survey completion. Visitors were asked to step away during completion of the survey.
Participants in the study were asked to complete an 8-page written survey, consisting of Likert-style questions (details below). Completion of the survey took approximately 10 minutes, and the RA approached patients only during naturally occurring episodes of waiting, such as in the waiting room or while awaiting results. Patients were provided with verbal and written informed consent, and were given a $5 gift card for their time.
Measures
The survey was composed of 6 different instruments; instruments were identified via a Centers for Disease Control and Prevention (CDC) compendium of Youth Violence assessment tools, and were selected based on risk factors evaluated and relevance to the study age group.11 To assess hostile/aggressive behavior, we used the Hostility portion of the Product-Symptom Checklist-90, 6 items scored on a Likert scale and designed to measure symptoms of aggression, and hostility.12 This instrument has been shown to have an internal consistency of 0.73 when tested among adolescent African-American males.13 To assess self-perceived likelihood of violence, we used the Likelihood of Violence and Delinquency Scale of the Sage Baseline Survey. The scale has 9 items, each with a Likert-type scale of multiple-choice options. When studied in a population of adolescent African-American males, it was found to have an internal consistency of 0.84.14 To assess recent history of engagement in violence, we used the Aggressive Behavior Scale of the Sage Baseline Survey, a 12-item survey of Likert-type questions which has been found to have an internal consistency of 0.66 to 0.80 among adolescent African-American males.15 To assess peer-group violence, we used the Friend’s Delinquent Behavior scale from the Denver Youth Survey, an 8-item scale found to have an internal consistency among adolescent African-American males of 0.89.15 Finally, exposure to community violence was measured using the Children’s Exposure to Community Violence survey, a 12-item survey with an internal consistency of 0.84 among adolescent African-American males.16
Although the survey instruments used had been developed and validated in adolescent populations, the majority have not been used to define ‘high-risk’ and “low-risk” youth based on survey results. For the purpose of defining the prevalence of violence risk factor exposure in the ED, we defined a “high risk” exposure to a given risk factor as strong endorsement (greater than the midpoint on the Likert scale) on more than half of items within a given assessment. Two alternative definitions of high risk were also evaluated: 1.) Any endorsement (2 or more on the Likert scale) on more than half of the items and 2.) Any endorsement of any item in the assessment.
Data Analysis
We analyzed data using SAS 9.2 (Cary, NC). We analyzed the survey data using Pearson’s χ2 test or Fisher’s Exact test as appropriate to determine the associations between survey results and demographic factors (gender and ethnicity). T-tests were used for assessing associations with age, which we entered as a continuous variable. We used bivariate and multivariate logistic regression to evaluate the association between demographic and violence risk factors and initial presentation to the ED for injury. Given small cell sizes for non-black races, we used a binary variable for black versus non-black race in the models. Final model selection was by backwards elimination with forced inclusion of key demographic variables. We included all usable data for participants who were unable to finish the survey.
RESULTS
Four hundred three eligible patients were approached, of whom 365(90.1%) consented to participate. Average age was 21.1 years. Participants were 57.2% female, 85.7% African-American, and 82.2% had completed high school.
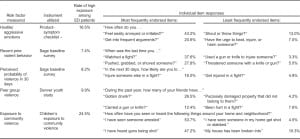
When comparing participants across all categories, we found that 32.3% of patients reported a high exposure to 1 or more risk factors surveyed. Rates of exposure to tested risk factors for violence/violent injury ranged from 7.4% of participants reporting recent violent behavior, to 24.5% reporting exposure to community violence (Table 1).
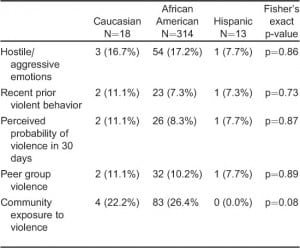
When comparing responses by ethnicity, we found no significant differences between rates of risk factor exposure between black vs. non-black participants. These results are limited by the very small numbers of participants who identified as a race/ethnicity other than African-American. This reflects the patient population served in study ED, as described in other research studies undertaken in this ED (Table 2).17
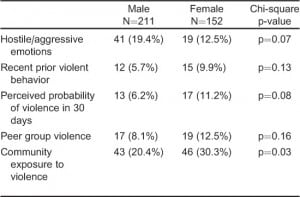
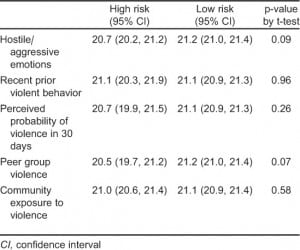
Male vs. female participants also showed notable similarities, with significant variation found only in responses to questions about exposure to community violence (20.4% of females vs. 30.3% of males, p=0.03). Risk exposures showing trends towards significance included hostile/aggressive feelings (19.4% among females vs. 12.5% among males, p=0.08) and self-reported prior violent behavior (6.2% among females vs. 11.2% among males, p=0.09) (Table 3). Differences in age between those identified as high risk versus low risk were small and not statistically significant (Table 4).
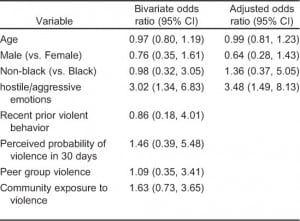
Age, sex, and race were not significantly associated with presentation to the ED for evaluation of an injury-related complaint versus a non-injury complaint. Those who reported high levels of hostile/aggressive impulses were significantly more likely to have presented for an injury-related complaint (odds ratio [OR] 3.02, 95% confidence interval [CI] 1.34, 6.83). This association remained significant after controlling for age, sex, and race (OR 3.48, 95% CI 1.49, 8.13). No statistically significant association was found between injury and other violence risk factors (Table 5).
DISCUSSION
These study findings show high rates of exposure to risk factors for violent injury among young adults presenting to this urban ED, including hostile/aggressive impulses (16.5% of the overall study sample), self-reported probability of future violent behavior (8.2%), prior history of violent/aggressive behavior (7.4%), peer group violent behavior (9.9%), and exposure to community violence (24.5%).
The most notable finding from this cross-sectional study was the strikingly similar rates of risk factor exposure when comparing participants by gender, ethnicity, and based on reason for ED visit, comparing patients seen for an injury compliant vs. those presenting for a non-injury complaint. When comparing participants by gender, we found a trend towards higher rates of hostile/aggressive feelings among females, and significantly higher exposure to community violence among males. These findings correlate with recent ED research, which found that gender was not significantly related with risk of peer violence.18 Reasons for the differences noted in this study might be based on a) gender differences in perceived social norms around reporting emotions (i.e., females might be more willing to report anger/hostility), and b) gender-based differences in time spent outdoors in the community, and different settings chosen for social aggregation, which may impact the likelihood of directly witnessing community violence.
Similarly, when comparing participants who presented to the ED for an injury complaint vs. a non-injury complaint, most categories surveyed did not show a significant difference in risk exposure by presenting complaint. The only risk factor that varied significantly was the proportion of patients with frequent hostile/aggressive feelings, at 37.5% among injured patients vs. 16.6% of non-injury patients. We found the similarities between injured vs. non-injured patients to be as illuminating as the difference; this suggests that targeting violence-prevention interventions toward patients who present after a severe injury may miss a large population of youth presenting for unrelated complaints, but who are nonetheless at very high risk.
Across the board, the findings of this study suggest that traditional expectations about demographic factors that indicate patient is high risk for violent injury may result in interventions that target only a small segment of the at-risk population, and that a targeted, uniform screening process may more effectively identify youth who would benefit from a violence-prevention program.
LIMITATIONS
This study is limited by the use of surveys relying on self-report data; we attempted to minimize bias introduced by self-report by providing patient privacy while completing the written survey and by assuring patient confidentiality and protection of patient data.
An additional challenge was presented by the fact that there is no current standardization for defining “high” levels of exposure to each tested risk factor that could be employed evenly across all of the scales. To operationalize risk factor exposure, and to facilitate future research about health consequences of risk factor exposure, the study authors developed a definition that intentionally defines a rather high threshold for a “positive screen.” Two less stringent definitions of high risk were also evaluated, but these alternative definitions showed no significant association of any of the risk factors with presentation for injury, suggesting they would be less effective for prediction of future injury. Future research into dose-response effects of risk factor exposure would be vital for violence-protection efforts. Association between self-reported risk factors and presentation for injury may be complicated by the fact that presentation for a violent injury may itself impact likelihood to report aggressive emotions, reported probability of future violence, etc.
Finally, this survey was performed at a single site, which was the ED of an inner-city, urban trauma center. Future studies in other clinical settings would help policymakers and health practitioners understand the degree to which these levels of exposures may be generalized to other geographic and clinical settings.
CONCLUSION
Over 30% of young adults presenting to an urban ED self-reported high exposure to risk factors for violent injury, with the most prevalent exposure being high rates of community violence, as reported by 25.8% of participants. When comparing by demographic categories, male and female patients varied only with respect to exposure to community violence, and we found no significant difference by participant ethnicity. We also found remarkable similarity when comparing participants who were initially seen in the ED for an injury complaint as compared with patients initially seen for a non-injury complaint. These findings suggest that a screening for violence risk factors would provide an important tool to identify and provide prevention services for young adults at risk for violent injury.
Acknowledgments
The authors would like to thank the Emory Center for Injury Control, which provided a seed grant through CDC 5 R49 CE001494 that supported this work, as well as guidance and support throughout the process.
Footnotes
Supervising Section Editor: Monica H. Swahn, PhD, MPH
Submission history: Submitted November 7, 2012; Revision received February 20, 2013; Accepted February 26, 2013
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2013.2.14810
Address for Correspondence: Abigail Hankin, MD, MPH. Emory University, Department of Emergency Medicine, 1364 Clifton Road, NE, Atlanta, GA 30322. Email: ahankin@emory.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. This work was funded through CDC Grant 5 R49 CE001494. The authors disclosed no other potential sources of bias.
REFERENCES
1. Anon. CDC – WISQARS (Web-based Injury Statistics Query and Reporting System) Available at:http://www.cdc.gov/injury/wisqars/index.html. Accessed October 31, 2009.
2. Centers for Disease control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQRS) [online]. National Center for Injury Prevention and Control, Centers for Disease Control and Preventino [2010 Jun 14]. Available at: www.cdc.gov/injury.
3. Luckenbill DF. Criminal homicide as a situated transaction. Social Problems. 1977;25(2):176–186.
4. Sege R, Stringham P, Short S. et al. Ten years after: examination of adolescent screening questions that predict future violence-related injury. J Adolesc Health. 1999;24(6):395–402. [PubMed]
5. Herrenkohl TI, Maguin E, Hill KG. et al. Developmental risk factors for youth violence. J Adolesc Health. 2000;26(3):176–186. [PubMed]
6. Borowsky IW, Ireland M. Predictors of future fight-related injury among adolescents. Pediatrics.2004;113(3):530. [PubMed]
7. Walls CA, Rhodes KV, Kennedy JJ. The emergency department as usual source of medical care: estimates from the 1998 National Health Interview Survey. Acad Emerg Med. 2002;9(11):1140–1145.[PubMed]
8. Houry D, Kemball R, Rhodes KV. et al. Intimate partner violence and mental health symptoms in African American female ED patients. Am J Emerg Med. 2006;24(4):444–450. [PMC free article][PubMed]
9. D’Onofrio G, Pantalon MV, Degutis LC. et al. Brief Intervention for Hazardous and Harmful Drinkers in the Emergency Department. Ann Emerg Med. 2008;51(6):742–750.e2. [PMC free article] [PubMed]
10. Zun LS, Downey L, Rosen J. The effectiveness of an ED-based violence prevention program. Am J Emerg Med. 2006;24(1):8–13. [PubMed]
11. Dahlberg LL, Toal SB, Swahn MH. Measuring violence-related attitudes, beliefs, and behaviors among youths: a compendium of assessment tools. Atlanta: Centers for Disease Control; 2005.
12. Derogatis LR, Rickels K, Rock A. “The SCL-90 and the MMPI a step in the validation of a new self-report scale” Br J Psychiatry. 1976;19:1–15. [PubMed]
13. Paschall MJ, Flewelling RL. Measuring intermediate outcomes of violence prevention programs targeting African-American male youth: an exploratory assessment of the psychometric properties of six psychosocial measures. Health Educ Res. 1997;12(1):117. [PubMed]
14. Flewelling RL, Pashcall MJ, Ringwalt CL. SAGE baseline survey. Research Triangle Park, NC: Research Triangle Institute. Flewelling, Paschall and Ringwalt. 1993.
15. Huizinga D, Weiher AW, Espiritu R. et al. Delinquency and crime: Some highlights from the Denver Youth Survey. Taking stock of delinquency: An overview of findings from contemporary longitudinal studies. 2003:47–91.
16. Richters JE, Martinez P. The NIMH community violence project: I. Children as victims of and witnesses to violence. Psychiatry. 1993;56(1):7–21. [PubMed]
17. Houry D, Kaslow NJ, Kemball RS. “Does screening in the Emergency Department Hurt or Help Victims of Intimate Partner Violence?” Ann Emerg Med. 2008;51(4):433–442. et al. [PMC free article][PubMed]
18. Walton MA, Cunningham RM, Goldstein AL. et al. Rates and correlates of violent behaviors among adolescents treated in an urban emergency department. J Adolesc Health. 2009;45(1):77–83.[PMC free article] [PubMed]


