| Author | Affiliation |
|---|---|
| Tina Wu, MD | Keck School of Medicine of the University of Southern California, Department of Emergency Medicine, Los Angeles, CA |
| Mark R. Bell, MD | Emergent Medical Associates, Manhattan Beach, CA |
| James R. Blakeman | Emergency Groups’ Office, Arcadia, CA |
| Irv Edwards, MD | Emergent Medical Associates, Manhattan Beach, CA |
| William K. Mallon, MD | Keck School of Medicine of the University of Southern California, Department of Emergency Medicine, Los Angeles, CA |
ABSTRACT
Introduction:
Physician reimbursement laws for diagnostic interpretive services require that only those services provided contemporaneously and /or contribute directly to patient care can be billed for. Despite these regulations, cardiologists and radiologists in many hospitals continue to bill for ECG and plain film diagnostic services performed in the emergency department (ED). The reimbursement value of this care, which is disconnected in time and place from the ED patient encounter, is unknown. In a California community ED with a 32,000 annual census, the emergency physicians (EPs) alone, by contract, bill for all ECG readings and plain film interpretations when the radiologists are not available to provide contemporaneous readings. To determine the impact of this billing practice on actual EP reimbursement we undertook an analysis that allows calculation of physician reimbursement from billing data.
Methods:
An IRB-approved analysis of 12 months of billing data cleansed of all patient identifiers was undertaken for 2003. From the data we created a descriptive study with itemized breakdown of reimbursement for radiograph and ECG interpretive services (procedures) and the gross resultant physician income.
Results:
In 2003 EPs at this hospital treated patients during 32,690 ED visits. Total group income in 2003 for radiographs was $173,555 and $91,025 for ECGs, or $19/EP hour and $6/EP hour respectively. For the average full-time EP, the combined total is $2537/month or $30,444 per annum, per EP. This is $8/ED visit (averaged across all patients).
Conclusion:
As EP-reimbursement is challenged by rising malpractice premiums, uninsured patients, HMO contracts, unfunded government mandates and state budgetary shortfalls, EPs are seeking to preserve their patient services and resultant income. They should also be reimbursed for those services and the liability that they incur. The reimbursement value of ECGs and plain film interpretations to the practicing EP is substantial. In the ED studied, it represents $30,444 gross income per full-time EP annually. Plain film interpretation services produce three times the hourly revenue of ECG reading at the hospital studied.
INTRODUCTION
ECGs and radiographs are fundamental diagnostic tools in the emergency department (ED); however, reimbursement for emergency physicians’ (EP) interpretations of these studies has long been a controversial issue. Most of the healthcare dollars for interpretative services went to cardiology and radiology specialists because they respectively interpreted and subsequently billed for ECG and radiograph interpretations performed in EDs, regardless of its immediate relevance to the patient care in question.1,2The Health Care Financing Administration’s policy (HCFA), now known as Centers for Medicare and Medicaid Services (CMS), assumed that the cardiology and radiology overread constituted patient care and has traditionally paid the first claim submitted. Previously, Medicare would consider the EP’s interpretation to be part of the attending physician’s overall workup and treatment of the patient in the ED, and this service would not be considered under a separate charge.3
The current study attempts to determine the financial impact of misdirected revenue from EPs for diagnostic studies, such as radiographs and ECG interpretations in the ED.4–6We examined the billing records of a 32,000 annual census community ED located in Chino Valley, California, and were able to extrapolate this data to the National Hospital Ambulatory Medical Care Survey (NHAMCS) data from 2005, which estimated 115 million ED visits in the country. We performed calculations, estimating the average annual revenue for EPs, based on billing and reimbursement data at this community hospital.
METHODS
We conducted a retrospective, descriptive study of consecutive ED visits for one year. The hospital’s Institutional Review Board approved the study to analyze 12 months of the ED’s billing data, cleansed of all confidential patient identifiers. The study was exempt from obtaining a written informed consent form due to the noninvasive, nonclinical nature of the analysis. This particular billing company has successfully withstood multiple outside audits to verify the validity of these billing and coding practices. Additionally, in a 2005 audit performed by National Health Information Center (NHIC), the Medicare carrier for California conducted a statewide audit of coding and documentation practices of EPs. The billing company successfully defended coding in all reviewed charts and confirmed that their approach to coding and billing for plain film and ECG interpretation met industry standards.
RESULTS
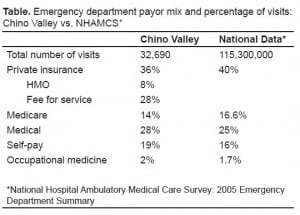
To generate an average reimbursement fee per interpretation we compiled and summated itemized lists of reimbursement fees for both the radiograph and ECG interpretations for the 12-month period. The payor mix, as shown in Table 1 – Medicare, 14%; MediCal, 28%; fee for service, 28%; contracted HMO, 8%; occupational medicine, 2%; and self-pay, 19% – is similar to national data from the NHAMCS 2005 survey. We recorded plain film radiograph billing only during ED hours without immediately available radiology interpretative services. There were 40 hours per day of EP coverage, with double coverage 16 hours daily. Radiology’s schedule of plain film coverage in 2003 left 9,048 hours “uncovered,” during which time the EPs billed for plain film interpretive services. This schedule included 15.5 hours each weekday, and 20 hours on Saturdays, and all day Sunday. Advanced studies, such as CT scans, angiograms, and formal ultrasounds, continued to be interpreted by radiologists off site. Since EPs read all ECGs, we recorded ECG billing for a total of 40 hours per day of EP coverage (due to 16-hours daily double coverage). This totaled 14,600 hours annually.
Actual revenue amounts in 2003 for ECGs and radiograph were $91,025 and $173,555 respectively. Using physician coverage data, these figures resulted in revenue of $19 per hour for radiograph interpretation and $6 for ECG interpretation per hour for each physician. For the average full-time EP, the combined total is $2,537 per month and $30,444 per annum for each individual physician.
DISCUSSION
With the growth of the specialty of emergency medicine, the first-line physician treating patients in the ED is usually a residency-trained EP. The interpretation of diagnostic tests is considered a critical skill in the armamentarium of their competencies, and in fact is part of the core content of the specialty.7 Furthermore, the credentialing process at many hospitals specifically includes these interpretive services for EPs. Ultimately, the EPs use these ancillary test interpretations to direct immediate patient management and treatment decisions. ECG and radiograph interpretations generally occur at the same time as patient care. Because of frequent unavailability, cardiologists and radiologists often interpret radiographs and ECGs hours to days after the patients’ departure from the ED; therefore, their interpretations often do not directly affect the patients’ ED visit and real-time medical decisions. Many hospitals that contract with teleradiology groups after hours often limit interpretation services to CT scan and MRI images.
Specialists have challenged EP billing for these services, arguing that because they have greater qualifications to interpret these studies patient care would suffer without their involvement. Several studies, however, report strong concordance rates of ECG interpretation between cardiologists and EPs and even challenge the concept that the “specialist” interpretation is the “gold standard.”8 The largest study, conducted with 400 patients by the University of California, Los Angeles Department of Medicine, concluded that a cardiologist’s review of ED ECGs interpreted by the EP in fact contributed little additional clinically relevant information.9. Twenty-five of 289 tracings, or 8.6%, had potentially significant ECG abnormalities for which the ED physician and cardiologists reads differed. In 2.7% of these cases, it was the ED physician who detected an abnormality that the cardiologist missed. In a review of the 2.7% of cases that differed, no cases were found to have been inappropriately managed. In conclusion, ECG interpretation by a cardiologist did not alter patient care. Other studies have found that using cardiologist interpretation as “the gold standard” is problematic as they have found that interpretations even between cardiologists reading the same ECG often vary substantially.10
The accuracy of EPs’ interpretations of plain radiography studies is also well documented in the literature. Concordance rates of radiographic readings between EPs and radiologists were generally quite high. Rates of disagreement between EPs and radiologists in the interpretation of radiographs have traditionally ranged from 8–11% with an alteration in treatment required in 0.1–3% of these patients.11–17 The significance of these numbers must be interpreted in light of other studies that have found inter-radiologist disagreement rates between 4–8%.18 A review of over 15,000 films in a community teaching hospital revealed 99% were correctly interpreted. Of the remaining 1% of EP “misreads,” less than half were deemed clinically significant.19 A George Washington University Medical Center study that reviewed 23,500 radiographs over a one- year period and evaluated patient care outcomes in those instances where post-discharge radiology interpretations differed from the EPs’ interpretation found an overall error rate of 1.8%. However, no adverse patient care outcomes resulted. Undesirable outcomes included permanent loss of function, suboptimal restoration, or prolonged recovery identified by delayed radiological diagnosis.20
Interdisciplinary concordance and interpretive skill discussions, while relevant, fail to address the central issue that only interpretation contemporaneous to care represents a service to patients in the ED. These studies and their interpretations result in real-time patient care decisions and management. Interpretation occurring at a later time can only serve a medical-legal or quality assurance purpose and should not be billed by specialists as a service to the patient.
Perhaps the most relevant and important study to date was conducted by the Office of Inspector General (OIG), a branch of the Department of Health and Human Service that detects fraud, waste, abuse and mismanagement. The study, which examined 356 medical records and telephone interviews with ED and radiology department directors at 18 hospitals in nine states, found that 44 percent of radiology interpretations were performed at least one day after the patient was discharged from the ED.21 Only 6.2% were interpreted and made immediately available to the treating EP prior to patient discharge. The remainder had no documentation of the time of interpretation or whether it was available to the treating EP. In no cases, did the radiologists’ reinterpretation require alterations in the initial treatment plan. As a result of this study, OIG findings concluded that a radiologist’s reinterpretations: 1) did not constitute patient care, 2) did not result in recall of patients, and 3) did not affect initial treatment. Consequently, OIG recommended to HCFA, “Pay for reinterpretations of radiographs only when attending physicians specifically request a second physician’s interpretation in order to render appropriate medical care before the patient is discharged. Any other reinterpretation of the attending physician’s original interpretation should be treated and reimbursed as part of the hospital’s quality assurance program. HCFA should implement this recommendation through either regulation or by seeking legislation as appropriate.” OIG projected that a minimum of $20.4 million was paid for these reinterpretations in 1990.5,6,21
Prior to 1996, reimbursement and billing occurred sporadically for the EP interpreting ECGs and plain radiographs with potentially thousands to millions of dollars of lost revenue. Per HCFA guidelines at that time interpretation of a radiograph or ECG given to an ED patient by a radiologist or cardiologist generally constituted an element of Part B service covered by the carrier. Often this meant that the cardiologist and radiologist submitted claims first and were reimbursed, even if their interpretation was performed subsequent to the EP’s interpretation, which ultimately dictated the patients’ disposition and management.
The 1996 Medicare rulings favored the reimbursement of ECG and radiograph for EPs. HCFA ruled in the Federal Register that reimbursement would occur only for the radiograph and ECG interpretation that directly and immediately contributes to the diagnosis or treatment of the patient.22 Only one radiograph and/or ECG interpretation will be reimbursed, except under unusual circumstances. Exceptions to this rule include a provision for a second read when the physician performing the initial interpretation believes that another physician’s expertise is required to examine a questionable finding. The second interpretation would be considered a quality assurance measure, unless the second interpretation changes the diagnosis. If a new diagnosis is reached, then CMS policy dictates that payment be provided for the second interpretation. Furthermore, any interpretation (per current Medicare policy) that is not performed contemporaneously is not medically necessary. A non-contemporaneous read can be made as a quality assurance function, but must not be billed to Medicare Part B. A 1995 Medicare Final Rule states: “Advise hospitals that the Medicare carrier may determine that the hospital’s official interpretation is for quality control and liability purposes only and is a service to the hospital rather than to an individual beneficiary.”22
For ECG and plain radiograph interpretations to be considered as a separate payment, specific conditions must be met. A distinction between an interpretation and a review of the findings must be made. A review of diagnostic tests is already included in the ED visit payment.22 Proper documentation of an ECG and radiograph interpretation as a billable procedure includes providing a complete written interpretation within the ED treatment records.2,6 A separate document of the EP’s interpretation is not necessary for billing purposes.
For radiograph interpretations, simply stating “normal” or “no acute disease” are inadequate. Comment must be made as to who provided the initial interpretation, the type of views/projection, specific description of anatomic location, pertinent positives, and a conclusion.2 For ECGs, the interpretation must include three of the following six elements: 1). Rhythm or rate, 2) axis, 3) intervals, 4) segments, 5) notation of a comparison with a prior ECG if one was available, and 6) summary of clinical condition.
While overreads performed by radiologists are a valuable resource to the hospital for quality assurance, they rarely alter a patient’s treatment plan.4 Billing for non-contemporaneous interpretations, which is often the practice of radiologists and cardiologists, is not considered patient care and would constitute fraud and abuse of the Medicare program,1 subject to penalties and False Claims laws.
Despite the clarity of these laws for EP reimbursements, many third parties still do not reimburse for these interpretations. Many argue that since hospital bylaws and the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) regulations require an “official interpretation,” it is the radiologists and cardiologists who are responsible for all radiographs and ECGs respectively performed in the hospital. They contend that these specialists have had more extensive training specific to these diagnostic studies and should ultimately be compensated for their expertise. In many hospitals the contractual arrangement for cardiology and radiology services specifically directs billing activities to the specialists and away from the EPs. These hospital arrangements should be considered fraudulent given the clarity of the language surrounding interpretive services. In effect, directing ECG and plain film interpretive fees to specialists who do not provide contemporaneous care is a form of fee splitting.
Two of the most important types of malpractice claims against EPs derive from “missed myocardial infarctions” and “missed fractures” where failure to diagnose is the tort. “Missed myocardial infarction” represents the most expensive claims while “missed fracture” represents one of the most frequent claims. These two diagnoses rely primarily on the accurate real-time interpretation of ECGs and radiographs. Since litigation of these in medical malpractice suits is so heavily reliant on EP interpretations, logic would dictate that it is the EPs who should be reimbursed for the interpretations since they assume the greatest liability for the interpretation.
The American College of Emergency Physicians (ACEP) has issued a policy statement regarding this topic, originally issued in 1996, reaffirmed in 2000, and revised and approved in 2006:
-
Interpretation of diagnostic studies ordered for the immediate evaluation and management of an ED patient should be done contemporaneously with the ED visit. A contemporaneous interpretation may be done by the emergency physician or by another specialist within the limits of training, experience and competence of that physician
-
The interpretation of the diagnostic studies, both preliminary reading and final reports, must be documented in writing, available contemporaneously with the patient’s evaluation, and filed in the patient’s medical record.
-
The emergency physician providing contemporaneous interpretation of a diagnostic study is entitled to reimbursement for such interpretation even if the study is reviewed subsequently as part of the quality control process of the institution in which the physician practices.23
As noted above, the OIG projected that $20.4 million was paid for ECG and plain film interpretations. The current study data suggests this is may be a substantial underestimate. In 2005 The CDC National Hospital Ambulatory Medical Care Survey (NAAMC), which measures ED utilization across the country, found that an estimated 115.3 million visits were made to hospital EDs, or about 39.6 visits per 100 persons.24Diagnostic and screening services were provided at 71% of visits, including 40.7 million visits (35%) receiving radiographs and 18.9 million visits receiving ECGs (16%). Extrapolating these figures from ED utilization data from this study and the estimated revenue generated at our community hospital, U.S. ED visits would generate approximately $779 million dollars for radiographs and $114 million for ECGs, for a grand total of $890 million dollars of revenue. The payor mix at the study site closely mimics the NHAMC national database. Even if the ECGs are deleted, using the assumption that many EPs do in fact bill for this service, the radiograph component is still $779 million, or 39-fold greater than the OIG estimate.
LIMITATIONS
Although continuous quality improvement data and management of patient callbacks are maintained at this hospital site for discrepancies between radiologists and EPs, as well as cardiologists and EPs, we did not report this data in the current study; therefore, the discrepancy data is not available. Additionally as mentioned above, although our hospital payor demographics reflect the majority of all hospitals in the U.S., based on the NHAMC national database, we caution the generalization of the study results to individual hospitals. In addition, in extrapolating the NHAMC data for ED visits, we are assuming that the vast majority of providers for those visits are EPs qualified in radiograph and ECG interpretation. This may vary widely again based on geographic location.
CONCLUSION
The potential revenue derived annually from the interpretation of radiograph and ECG interpretive services is substantial. At this community hospital, the average full-time EP receives $30,444 for these services each year. Depending on yearly income and geographic location, this could mean up to 10–20% of their annual income. If we assume these funds are largely untapped, or are misdirected to those who are billing for these studies (that are not interpreted contemporaneously to patient care) in other hospitals, then EPs currently are losing a large portion of their revenue. The payor mix represented by the study-site hospital reflects the demographics of many EDs in the country. However, because reimbursement rates vary widely in different regions, caution should be used in generalizing this data to other hospitals.
Non-contemporaneous interpretation of radiographs and ECGs are not medically necessary, do not contribute to patient care, and consequently should be considered a submission of a false claim and carry severe consequences. Attempts by hospitals and specialists to circumvent Medicare rules should be deemed as fraudulent activity. EPs are entitled to be reimbursed for their interpretive services that affect the patients’ emergency treatment and disposition.
Value is provided both to the patient and the EP when ECG and radiograph interpretations are delivered in a timely manner that is cost effective and supported by quality assurance measures. The additional time needed to document an appropriate radiograph and ECG interpretation is well worth the reimbursement value for the EPs’ practice, as the results of this study indicate. Patients also benefit from these immediate findings and appropriate management based on these interpretations in a timely and meaningful fashion, thus maximizing the quality of ED care.
Footnotes
Supervising Section Editor: Jeffrey Druck, MD
Submission history: Submitted June 19, 2008; Revision Received December 04, 2008; Accepted January 23, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Tina Wu, MD. Emergent Medical Associates, 111 North Sepulveda Blvd, Suite 210, Manhattan Beach, CA 90266
Email: tinawumd2@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Levin DC, Rao VM. Turf wars in radiology: emergency department ultrasound and radiography. J Am Coll Rad. 2005;2:271–3.
2. Blakeman J. Diagnostic Interpretive Services: Coding and documentation issues. Course lecture presented at: EM Seminars: Beyond basics: Providing expert training in emergency medicine reimbursement and coding; May 12, 2007; Honolulu, HI.
3. Centers for Medicare and Medicaid Services, Department of Health and Human Services. Medicare Carriers Manual Section 2020G.
4. Preston CA, Marr JJ, III, Amaraneni KK, et al. Reduction of “callbacks” to the ED due to discrepancies in plain radiograph interpretation. Am J Emerg Med. 1998;16:160–2.[PubMed]
5. Blakeman JR. HCFA final rule: ED physicians can be paid for reading X-rays, ECGs. ED Manag. 1996;8:21–4. [PubMed]
6. Blakeman JR. Diagnostic interpretations: improving chances for being paid. ED Manag.1995;7:9–11. [PubMed]
7. 2005 EM Model Review Task Force. Thomas HA, Binder LS, Chapman DM, et al. The 2003 model of the clinical practice of emergency medicine: the 2005 update. Ann of Emerg Med. 2006;48:e1–17. [PubMed]
8. Eken C, Goksu E, Eray O, et al. The consistency of emergency physicians’ and cardiologists’ ECG interpretation and likelihood classification of chest pain patients. Inter J of Clin Prac. 2006;60:1194–7.
9. Kuhn M, Morgan MT, Hoffman JR. Quality assurance in the emergency department: evaluation of the ECG review process. Ann Emerg Med. 1992;21:10–5. [PubMed]
10. Salerno SM, Alguire PC, Waxman HS. Competency in interpretation of 12-lead electrocardiograms: A summary and appraisal of published evidence. Ann Int Med.2003;138:751–61. [PubMed]
11. Espinosa JA, Nolan TW. Reducing errors by emergency physicians in interpreting radiographs: longitudinal study. Brit Med J. 2000;320:737–40. [PMC free article][PubMed]
12. Robinson PJ, Wilson D, Coral A, et al. Variation between experienced observers in the interpretation of accident and emergency radiographs. Brit J Rad. 1999;72:323–330.
13. Lufkin KC, Smith SW, Matticks CA, et al. Radiologists’ review of radiographs interpreted confidently by emergency physicians infrequently lead to changes in patient management. Ann Emerg Med. 1998;31:202–7. [PubMed]
14. Scott WW, Jr, Bluemke DA, Mysko WK, Weller GE, Kelen GD, Reichle RL, et al. Interpretation of emergency department radiographs by radiologists and emergency medicine physicians: teleradiology workstation versus radiograph readings. Rad.1995;195:223–229.
15. Fleischer G, Ludwig S, McSorley M. Interpretation of pediatric x-ray films by emergency department pediatricians. Ann Emerg Med. 1983;12:153–8. [PubMed]
16. Rhea JT, Potsaid MS, DeLuca SA. Errors of interpretation as elicited by a quality audit of an emergency department facility. Rad. 1979;132:277–80.
17. Benger JR, Lyburn ID. What is the effect of reporting all emergency department radiographs? Emerg Med J. 2003;20:40–3. [PMC free article] [PubMed]
18. Siegle RL, Baram EM, Reuter SR, et al. Rates of disagreement in imaging interpretation in a group of community hospitals. Acad Rad. 1998;5:148–54.
19. Brunswick JE, Ilkhanipour K, Seaberg DC, et al. Radiographic interpretation in the emergency department. Am J Emerg Med. 1996;14:346–8. [PubMed]
20. O’Leary MR, Smith MS, O’Leary DS, et al. Application of clinical indicators in the emergency department. JAMA. 1989;262:3444–7. [PubMed]
21. Office of Inspector General, Department of Health and Human Services. Medicare’s reimbursement for interpretations of hospital emergency room radiographs. Document no. OEI-02-89-01490, July 30, 1993.
22. Federal Register, December 8 1995; Volume 60, No. 236: 63123–63357.63357.[PubMed]
23. ACEP Policy statement: Interpretation of Imaging diagnostic studies. Ann Emerg Med.2006;48:645.
24. Nawar EW, Niska RW, Xu J. National hospital ambulatory medical care survey: 2005 emergency department summaryAdvanced Data From Vital and Health Statistics US Department of Health and Human Services.2007. 386.


