| Author | Affiliation |
|---|---|
| Raymond J. Roberge, MD, MPH | National Personal Protective Technology Laboratory/National Institute for Occupational Safety and Health/Centers for Disease Control and Prevention, Pittsburgh, PA |
| Marc R. Roberge | Washington and Jefferson College, Washington, PA |
ABSTRACT
Introduction:
Osteopathic Manipulation Techniques (OMT) have been shown to be effective therapeutic modalities in various clinical settings, but appear to be underutilized in the emergency department (ED) setting. To examine barriers to the use of OMT in the ED and provide suggestions to ameliorate these barriers.
Methods:
Literature review
Results:
While the medical literature cites numerous obstacles to the use of OMT in the ED setting, most can be positively addressed through education, careful planning, and ongoing research into use of these techniques. Recent prospective clinical trials of OMT have demonstrated the utility of these modalities.
Conclusion:
Osteopathic Manipulation Techniques are useful therapeutic modalities that could be utilized to a greater degree in the ED. As the number of osteopathic emergency physicians increases, the opportunity to employ these techniques should increase.
INTRODUCTION
Osteopathic Manipulation Techniques (OMT) are therapeutic maneuvers (Table 1) employed by osteopathic physicians to treat somatic dysfunction (defined as impaired or altered function of related components of the somatic system, including skeletal, arthrodial, and myofascial structures, as well as related vascular, lymphatic and neural elements).1–3 Recent prospective studies have demonstrated statistically significant improvement in outcomes for the treatment of neck pain and ankle sprains with the use of OMT in the emergency department (ED).4,5 Further, the Agency for Health Care Policy and Research of the U.S. Public Health Service has previously suggested that the use of spinal manipulation is one of the safest methods for relief of spinal discomfort in adults presenting with acute low back pain6 and often meets with positive results.7

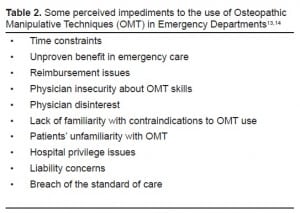
In 1999, 2,559 osteopathic physicians were practicing emergency medicine, accounting for 8% of the emergency physician workforce.8 Increases in class sizes and the opening of seven more osteopathic medical schools in the interim (two new osteopathic medical schools and five new campuses of existing osteopathic medical schools) suggest that the number of osteopathic emergency physicians (OEP) will increase, as will, ostensibly, the opportunity to employ OMT in the ED. The increased use is also potentially enhanced by the finding that a significant proportion of ED patients is open to, and utilizes, alternative medical therapies.9 With greater than 110 million ED patient visits annually in the U.S., this amounts to potentially nine million patients cared for by OEP each year.10 Despite the wider opportunities for use of OMT in the emergency setting, recent data indicate that perhaps only 55% of OEP utilize OMT in their practice and a minority (28%) report daily or weekly usage.11 A number of impediments to OMT use have been cited in the literature (Table 2). This article will review some cited obstacles to OMT utilization in the ED and explore amelioration strategies.11,12
Time Constraints
OEPs utilize OMT significantly less than family practice osteopathic physicians.13 Lack of time has been cited as the primary reason.11,12 Because the number of EDs in the U.S. has decreased 14% since 1993, greater average patient numbers at remaining sites without concomitant increases in staff means less time per patient.14 In addition, fewer procedures are being performed in the ED, in part because of increased documentation requirements.15 The average estimated time needed for the actual performance of OMT in the ED ranges from as little as 2 – 6 minutes to 10 – 20 minutes, depending on the procedure and the practitioner’s skills.4,12 If one accepts both the suggested guidelines that the optimal number of patients seen by EPs should not exceed 2.5 patients/hour16and the stated performance time estimates for OMT, it is possible that in select cases OMT could be utilized in a timely fashion in most ED settings. While performance times could be enhanced by the development of teaching programs in osteopathic medical schools that focus on OMT use in the ED clinical setting to maximize efficiency and time management, such programs are in short supply.11 OMT that can be performed efficiently and offer the most immediately-apparent results (i.e., soft tissue treatment, high-velocity/low amplitude treatment, muscle energy treatment) should be employed.11 Triage protocols could be established to identify patients who would potentially agree to its use and who could benefit most from OMT (e.g., torticollis, low back pain, etc.), and an ED room could be designated specifically for OMT.11
Unproven Benefit in Emergency Care
Recent data has shown that 13.8% of patients coming to an ED in the U.S. have complaints referable to the musculoskeletal system.10 Despite the commonplace use of OMT in the medical community (it is estimated that there are hundreds of millions of such treatments per year in the U.S.)17 and the great numbers and variety of patient encounters amenable to use of OMT,11,12 only two randomized, controlled studies from EDs attest to their efficacy in the treatment of musculoskeletal dysfunction.18–21 Both demonstrated benefit from OMT use for acute musculoskeletal disorders.4,5 One ED study found that the use of OMT for the treatment of acute ankle sprains was associated with a statistically significant improvement in edema and pain and a trend toward increased range-of-motion immediately following intervention.4 In the second ED study, which compared OMT to intramuscular ketorolac for the treatment of acute neck pain, OMT proved just as efficacious in providing pain relief, but was significantly better in reducing pain intensity. Possible reasons for the dearth of evidence-based studies in osteopathic medicine include concentration on clinic services and obtaining practice rights, and improving the profession’s standing.22 However, with the ever-increasing emphasis on evidence-based medicine, it is incumbent upon OEPs to institute well-designed, randomized ED studies that will address the utility of OMT in terms of safety, efficacy, and cost-effectiveness.23 If such studies continue to corroborate their efficacy, OMT use should increase in the ED. Currently six prospective, randomized studies are being carried out under the auspices of osteopathic medical schools and the American Osteopathic Association, but none are ED trials.24 A recent editorial22 highlighted this issue of evidence-based osteopathic medicine by calling for the osteopathic medical profession to make a dedicated effort to develop research that can test OMT mechanisms and define their effectiveness. Thus, the ultimate role of OMT in the ED therapeutic armamentarium can only fully be defined through well-conducted, prospective clinical trials that will weigh its efficacy, or lack thereof, for specific disorders.
Physician Insecurity with OMT Skills
Proficiency in OMT requires constant practice and application, and insecurity may reflect limitations in training and/or clinical experience. Classroom instruction is carried out during four years of osteopathic medical school, and competence must be demonstrated on the Certification of Osteopathic Medicine Licensure Examination (COMLEX) required for medical licensure in the U.S. OMT training continues in osteopathic internship and osteopathic residency training, and studies have shown that the use of OMT correlates closely with OMT interest and training during internship and residency.13,25 Osteopathic physicians who undertake osteopathic residency training use OMT significantly more than those osteopaths who pursue training in allopathic residencies.26 However, more than 50% of osteopaths currently enter allopathic residency training programs each year where they are generally not exposed to OMT.27 This lack of supplementary OMT training, coupled with the lack of OMT role models in allopathic programs, inhibits OMT skills development of osteopathic resident physicians.28 Therefore, it seems that the key to overcoming physician insecurity of OMT skills is ensuring that appropriate skills learned in osteopathic medical school will continue to be honed during the postdoctoral clinical training period. An increase in the number of osteopathic residency programs has been suggested as one measure to ensure that adequate numbers of osteopathic physicians continue to learn OMT skills.28 The incorporation of OMT training for osteopathic physicians in allopathic residencies also continues the learning process, and such programs have shown the added benefit of spurring interest in OMT by allopathic physicians.27,29 One survey reported that 90% of allopathic family medicine resident physicians believe that OMT is effective for treating somatic dysfunction.27 For physicians who have been in private practice for a number of years with limited OMT exposure, refresher courses are available.30
Reimbursement
Third-party payers [e.g., governmental (Medicare, Medicaid, etc.), and private insurers (insurance companies, health management organizations, preferred provider organizations, etc.)] are the primary sources of income for healthcare institutions and providers. The types of procedures that can be billed for by OEPs include any service listed in the American Medical Association’s Current Procedural Terminology (CPT) codes.31Five CPT codes (98925, 98926, 98927, 98928, 98929), referring to different body regions [i.e., head region, cervical region, thoracic region, lumbar region, sacral region, pelvic region, lower extremities, upper extremities, rib cage region, abdomen, and viscera region] are identified for OMT. Although procedures such as OMT are legitimately billable and reimbursable, some third-party payer practices may result in non-payment or decreased payment. Specifically, insurers may attempt to “bundle” services (i.e., combining the payment of one service into another to reduce payment) or utilize capitation of services, as occurs frequently within the framework of managed care contracts.32,33 Use of a modifier will allow OMT to be billed separately, in some situations, if it is designated as a separate and distinct service rendered during an ED visit. The most commonly-employed modifier is modifier-25 that indicates a significant, separately identifiable evaluation and management service by the same physician on the same day of the procedure or other service provided.32 The combination of EP inexperience with billing and recent data have demonstrated that a significant number of EPs are naïve regarding OMT billing in their practices and that only a small minority of hospital EDs (16.8%) bill for OMT.11 Therefore, it is imperative that OEPs be familiar with the types of service arrangements they have with insurers and they should work closely with their billing providers to remain current regarding reimbursement issues to ensure appropriate reimbursements for OMT. In these days of declining healthcare institution revenues, the additional revenue generated from OMT performed in the ED can be substantial for the practitioner and the institution.12
Physician Disinterest
The reported lack of interest in using OMT by osteopathic physicians may be related to a number of issues.12 It has been suggested that unsuccessful applicants to medical schools who subsequently are accepted to osteopathic medical school may place limited importance on OMT and thus be less likely to utilize this modality.34 Also, as more osteopathic physicians compete for residency training in non-primary care specialties, the emphasis on OMT diminishes.35 Similarly, the growth in the number of osteopathic physicians who graduate each year has increased the number of these individuals who enroll in allopathic training programs where there is no exposure to OMT. Interestingly, there appears to be increasing interest in OMT among allopathic physicians.28 One study noted that approximately two-thirds of allopathic physicians in family practice residencies expressed interest in learning OMT and supported the concept of certification by the American Osteopathic Association (AOA) of allopathic physicians who demonstrate proficiency in OMT.27 Other allopathic programs (i.e., physical medicine and rehabilitation medicine) are increasingly recognizing the need for OMT.36 Since it has been shown that interest in OMT correlates with the emphasis placed on it during postgraduate training, an increase in the number of osteopathic residency programs, or an emphasis on combining elements of osteopathic medicine into allopathic programs, might serve to spur increased interest and usage of OMT.28,29 CME programs in OMT increase interest and expertise among osteopathic physicians, as well as allopathic physicians. The greater the number of allopathic physicians who use OMT, the greater likelihood of continued interest by osteopathic physicians. Disinterest is usually overcome as the benefits of OMT are consistently realized by the practitioner.12
Lack of Knowledge of Contraindications to OMT Use
Practicing physicians must be aware of the contraindications to any procedure, and OMT is no exception. Development of formal guidelines their use in the ED have been proposed that would serve to diminish inappropriate use.11 Thrust techniques have the greatest number of absolute contraindications, including: malignancy, osteoporosis, severe rheumatoid arthritis, carotid or vertebrobasilar vascular disease, fracture, history of a pathological fracture, connective tissue disease, aneurysm, and anticoagulant therapy.1,36 The appropriateness of the use of thrust techniques for lumbar radiculopathy is unresolved.37 Soft tissue, muscle energy, and myofascial release techniques have few contraindications.37 A checklist of contraindications can be placed in the ED chart of patients being considered for OMT to reinforce precautions against inappropriate use.12
Patient Unfamiliarity with OMT
A significant proportion of Americans are not familiar with osteopathic medicine. However, the 44 million ambulatory care visits made annually to osteopathic physicians suggest that familiarity with osteopathic medicine and (by extension) OMT is increasing.1In addition, a sizable proportion of ED patients utilize alternative therapies, including OMT.3,9 One survey noted that 23% of ED patients had previously utilized manipulation-type therapy (chiropractic).38 This suggests that many ED patients would be amenable to considering the use of OMT. As with any medical procedure, a thorough explanation of the procedure beforehand will ensure patient understanding and cooperation. This should include a discussion of alternatives, risks/benefits, and assessment of the patient’s understanding and preference.39
Hospital Privilege Issues
Physician credentialing is the process of gathering information regarding a physician’s qualifications for appointment to the medical staff, whereas delineation of clinical privileges denotes approval to provide specific services or perform specific procedures by a physician.40 The specific process for physician credentialing and delineation of clinical privileges must be defined by medical staff and department bylaws, policy, rules, or regulations. Hospital privileges are not owned by any specific department and are granted by the hospital board on the basis of the practitioner’s documented training, experience and current clinical practice.41 OEPs wishing to use OMT in the ED must include OMT in their request for clinical privileges, as do physicians from other specialties who wish to use these techniques in hospital-based settings (e.g., family medicine practitioners, internists), and need to be able to document appropriate training and experience. Since competence in OMT is part of the COMLEX examination for medical licensure in osteopathic medicine, passage indicates appropriate knowledge and experience in OMT. Graduates of an allopathic family medicine residency program that offers a one-month course in OMT have obtained hospital privileges for OMT with receipt of a letter from their program documenting completion of such study.42
Liability Concerns
While liability concerns are ever present given the current surge in malpractice litigation in the U.S., few therapeutic modalities possess as safe a track record as OMT. A review encompassing six decades of use in the U.S. (several hundred million treatments performed annually) noted only 185 reports of injury, although there are concerns about underreporting.17 Similarly, no treatment-related complications were noted in a study of 346 pediatric patients undergoing OMT.43 Some reported injuries following manipulation techniques (including OMT) have included stroke secondary to vertebral artery or vertebrobasilar artery injury, Wallenberg syndrome, visual defects, hearing loss, balance defects, phrenic nerve injury, cauda equine syndrome, disc herniations, fractures, dislocations, but few of these were attributable to osteopathic physicians.44–46The key to good outcomes in OMT, as with most therapeutic procedures, is appropriate training and a thorough patient history and physical examination prior to manipulation.17 Thorough knowledge of contraindications to OMT is also requisite.12Documentation of informed consent before a medical procedure is a prudent undertaking and may be more important in the ED because EPs are less likely to have an ongoing relationship with their patients than other physicians.47
Breach of the Standard of Care
In legal terms, the standard of care is the level at which the average, prudent provider in a given community would practice. It is how similarly qualified practitioners would have managed the patient’s care under the same or similar circumstances. The standard of care is established in liability cases through the use of expert witnesses, and the medical malpractice plaintiff must establish that it has been breached. Osteopathic physicians are trained in OMT and must demonstrate their competence in OMT on their medical licensure examination (COMLEX). Numerous well-designed studies have demonstrated that OMT is comparable to other therapeutic modalities with respect to numerous disorders (e.g., neck pain, back pain, ankle sprain, etc.),4,23–25 thereby validating OMT as an acceptable therapeutic modality. The estimated use of OMT hundreds of millions of times per year in the this country with few reports of complications attests to its safety, an issue that is paramount in defining the standard of care.17
CONCLUSION
While OMT are safe, effective therapeutic modalities that have practical application in the ED evaluation and treatment of musculoskeletal disorders, these techniques are currently underused. Cited impediments to its use in the ED by OMT-credentialed physicians can be overcome by guidelines-directed use, and education of ED staff, hospital administration and patients as to its potential benefits. More randomized ED clinical trials of OMT are needed to delineate positive or negative aspects of these therapies as they relate to specific disorders. Studies that show benefit in the ED setting will enhance its application.
Footnotes
Supervising Section Editor: Laleh Gharahbaghian, MD
Submission history: Submitted April 16, 2008; Revision Received September 22, 2008; Accepted October 20, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Raymond J. Roberge, MD, MPH, National Personal Protective Technology Laboratory, P.O. Box 18070, 626 Cochrans Mill Road, Pittsburgh, PA 15236
Email: dtn0@cdc.gov
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. This work reflects Dr. Roberge’s personal views and was not carried out as part of his official duties with the National Personal Protective Technology Laboratory/National Institute for Occupational Safety and Health/Centers for Disease Control and Prevention
REFERENCES
1. Lesho EP. An overview of osteopathic medicine. Arch Fam Med. 1999;8:477–484.[PubMed]
2. Osteopathic manipulative techniques. American Academy of Osteopathy website. Available at: http://drtortu.com/Osteopathic%20Manipulative%20Techniques.htmAccessed August 3, 2007.
3. Licciardone J, Gamber R, Cardarelli K. Patient satisfaction and clinical outcomes associated with osteopathic manipulative treatment. J Am Osteopath Assoc.2002;102:13–20. [PubMed]
4. Eisenhart AW, Gaeta TJ, Yens DP. Osteopathic manipulative treatment in the emergency department for patients with acute ankle injuries. J Am Osteopath Assoc.2003;103:417–421. [PubMed]
5. McReynolds TM, Sheridan BJ. Intramuscular ketorolac versus osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. J Am Osteopath Assoc. 2005;105:57–68.[PubMed]
6. Biggs SJ, Bowyer OR, Braen GR, Brown K, Deyo R, et al. Acute low back problems in adultsClinical practice guideline No. 14, Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services; Rockville, MD: 1994[AHCPR Publication No. 95-0642].
7. Dillard JN, Knapp S. Complementary and alternative pain therapy in the emergency department. Emer Med Clin No Amer. 2005;23:529–549.
8. Pollard JA, Leveque EA, Lewin MR. Osteopathic physicians in emergency medicine.Ann Emer Med. 2003;42:261–265.
9. McCubbin TR, MacCormack LM, Adams HR, Glassey MS, Sarche S, Feldhaus K. Alternative medicine use among emergency department patients. Acad Emer Med.1999;6:553.
10. McCraig LF, Nawar EW.National hospital ambulatory medical care survey: 2004 emergency department summary. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics website. Available at:http://0www.cdc.gov.mill1.sjlibrary.org/nchs/about/major/nhcs/nhcs_reports.htmAccessed August 3, 2007.
11. Ray AM, Cohen JE, Buser BR. Osteopathic emergency physician training and use of osteopathic manipulative therapy. J Am Osteopath Assoc. 2004;104:15–21. [PubMed]
12. Paul FA, Buser BR. Osteopathic manipulative treatment application for the emergency department patient. J Am Osteopath Assoc. 1996;96:403–409. [PubMed]
13. Spaeth DG, Pheley AM. Use of osteopathic manipulative treatment by Ohio osteopathic physicians in various specialties. J Am Osteopath Assoc. 2003;103:16–26.[PubMed]
14. Anonymous: U.S. Emergency care system overcrowded and understaffed, American College of Emergency Physicians Says. MedicalNews website. Available at:http://www.medicalnewstoday.com/medicalnews.php?newsid=35991 Accessed August 3, 2007.
15. Swoboda TK, Munyak J. Use of a sedation-analgesia datasheet in closed shoulder reductions. J Emer Med. 2005;29:129–135.
16. American Academy of Emergency Medicine. Position Statement. Emergency Physician-to-Patient Staffing Ratios. Available at:http://www.aaem.org/positionstatements/statements201.php Accessed on September 22, 2008.
17. Vick DA, McKay C, Zengerle CR. The safety of manipulative treatment: review of the literature from 1925 to 1993. J Am Osteopath Assoc. 1996;96:113–115. [PubMed]
18. Andersson GBJ, Lucent T, Davis AM, Kappler RE, Lipton JA, Leurgans S. A comparison of osteopathic spinal manipulation with standard care for patients with low back pain.New Engl J Med. 1999;31:1426–1431. [PubMed]
19. Hoehler FK, Tobis JS, Buerger AA. Spinal manipulation for low back pain. J Am Med Assoc. 1981;245:1835–1838.
20. Burton AK, Tillotson KM, Cleary J. Single-blind randomized controlled trial of chemonucleolysis and manipulation in the treatment of symptomatic lumbar disc herniation. Eur Spine J. 2000;9:202–207. [PubMed]
21. Williams NH, Wilkinson C, Russell I, Edwards RT, Hibbs R, Linck P, Muntz R. Randomized osteopathic manipulation study (ROMANS): pragmatic trial for spinal pain in primary care. Fam Prac. 2003;20:662–669.
22. Rogers FJ. A call for evidence-based medicine: evolving standards and practices for JAOA readers and authors alike. J Am Osteopath Assoc. 2007;107:293–294.
23. Licciardone JC. Osteopath research: elephants, enigmas, and evidence. Osteopath Med & Primary Care. 2007;1:7. [PMC free article] [PubMed]
24. Osteopathic Manipulation Techniques U.S. National Institutes of Health website. Available at: www.ClinicalTrials.gov Accessed on November 11, 2007.
25. Fry LJ. Preliminary findings on the use of osteopathic manipulative treatment by osteopathic physicians. J Am Osteopath Assoc. 1996;96:91–96. [PubMed]
26. Johnson SM, Kurtz ME. Diminished use of osteopathic manipulative treatment and its impact on the uniqueness of the osteopathic profession. Acad Med. 2001;76:821–828.[PubMed]
27. Allee BA, Pollak MH, Malnar KF. Survey of osteopathic and allopathic residents’ attitudes toward osteopathic manipulative treatment. J Am Osteopath Assoc.2005;105:551–561. [PubMed]
28. Shubrook JH. The current state of osteopathic manipulative treatment in the hospital setting. Osteopath Fam Phy News. 2006;6:1, 12–13.
29. Przekop PR, Tulgan H, Przekop A, DeMarco WJ, Campbell N, Kisiel S. Implementation of an osteopathic manipulative medicine clinic in an allopathic teaching hospital: a research-based experience. J Am Osteopath Assoc. 2003;103:543–549. [PubMed]
30. Harvard Medical School, Department of Continuing Education. Introduction to Osteopathic Manipulative Medicine. Harvard Medical School website. Available at:http://www.cme.hms.harvard.edu/index.asp?SECTION=Classes&ID=00271286&SO=NAccessed on July 14, 2007.
31. Edelberg C. Emergency department coding and billing. Emer Med Clin No Amer.2004;22:131–151.
32. Brunetti S.Payers playing games. Medical Economics. Pennsylvania Chapter American College of Emergency Physicians website. Available at:http://www.paacep.org/MedicalEconomics.htm Accessed on: Accessed on July 14, 2007.
33. Halaja-Henriques A.Coding case study – OMT codes for use by DOs and MDs. PA Academy of Family Physicians website. Available at:http://www.pafp.com/MMS/coding/omt.htm Accessed on July 14, 2007.
34. Aguwa MI, Koop Liechty D. Professional identification and affiliation of the 1992 graduate class of the colleges of osteopathic medicine. J Am Osteopath Assoc.1999;99:408–420. [PubMed]
35. Meyer CT, Price A. The crisis in osteopathic medicine. Acad Med. 1992;67:810–816.[PubMed]
36. Atchison JW, Newman RL, Kim GV. Interest in manual medicine among residents in physical medicine and rehabilitation. The need for increased instruction. Am J Phys Med Rehabil. 1995;74:439–443. [PubMed]
37. Stoll ST, Russo D. The physiologic basis of manipulation. In: Wainapel SF, Fast A, editors. Alternative Medicine and Rehabilitation: A Guide for Practitioners. New York, NY: Demos Medical Publishing; 2002. pp. 1–30.
38. Kim S, Munoz KN, Braun JE, Doshi A, Wayland KT, Hohrmann JL, Clark S, Radeos MS, Camargo CA., Jr Use of complementary/alternative medicine among emergency department patients: a prospective multicenter study. Acad Emer Med. 2003;10:549.
39. Braddock CH, III, Fihn SD, Levinson W, Jonsen AR, Pearlman RA. How doctors and patients discuss routine clinical decisions: informed decision making in the outpatient setting. J Gen Intern Med. 1997;12:339–345. [PMC free article] [PubMed]
40. Anonymous American College of Emergency Physicians Policy Statement: Physician credentialing and delineation of clinical privileges in emergency medicine. Ann Emer Med. 2006;48:511.
41. Hirsch EA. Fighting for hospital privileges. Fam Pract Manag. 2004;11:69–74.[PubMed]
42. Leiber JD. Allopathic family medicine residents can learn osteopathic manipulation techniques in a 1-month elective. Fam Med. 2005;37:693–5. [PubMed]
43. Hayes NM, Bezilla TA. Incidence of iatrogenesis associated with osteopathic manipulative treatment of pediatric patients. J Am Osteopath Assoc. 2006;106:605–608. [PubMed]
44. Manipulation of the cervical spine: risks and benefits. Phys Therapy. 1999;79:50–65.
45. Stevinson C, Ernst E. Risks associated with spinal manipulation. Am J Med.2002;112:566–571. [PubMed]
46. Lesho EP. An overview of osteopathic medicine. Arch Fam Med. 1999;8:477–484.[PubMed]
47. Moskop JC. Informed consent in the emergency department. Emer Med Clin No Amer.1999;17:327–339.


