| Author | Affiliation |
|---|---|
| William M. Suh, MD | University of California, Irvine Medical Center, Department of Medicine, Division of Cardiology, Orange CA |
| Subramaniam C. Krishnan, MD | University of California, Irvine Medical Center, Department of Medicine, Division of Cardiology, Orange CA |
ABSTRACT
A hiccup, or singultus, results from a sudden, simultaneous, vigorous contraction of the diaphragm and inspiratory muscles, accompanied by closure of the glottis. Hiccups can be associated with bradyarrhythmias. The mechanism of this phenomenon is likely hiccup-induced Valsalva maneuver and increased parasympathetic tone. We present a case of a patient with violent hiccups producing a bradyarrhythmia.
CASE
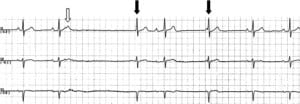
A 76-year-old male with no prior cardiac history was hospitalized after chest wall and pelvic trauma following a fall from a ladder. On the third hospital day, a pause lasting 2.6 seconds was seen on telemetry while the patient was awake (Figure 1). Progressive PR prolongation is visible in the first two cardiac cycles. The T wave of the second cycle is deformed suggesting a superimposed premature atrial contraction with atrioventricular block. A junctional beat is visible 2.6 seconds after the preceding QRS, followed by a sinus beat with a prolonged PR interval and another junctional beat. There was no associated lightheadedness, presyncope, or syncope. Interestingly, the patient reported having a violent bout of hiccups (which he described as being the worst of his life) during the time the bradyarrhythmia was recorded on telemetry.
The patient was normotensive and his pulse rate was noted to be in the sixties. The cardiac examination was normal. Patient’s medications included metoprolol 50 mg orally twice daily (started during this hospitalization for episodes of atrial tachycardia) and morphine sulfate intravenously as needed for pain control. Laboratory data demonstrated no electrolytes disturbances and a normal thyroid stimulating hormone level. Transthoracic echocardiogram was performed, which showed normal left ventricular function, no significant valvular abnormality, normal aortic root, and no evidence of cardiac contusion. Based on these findings, the etiology of the atrial tachycardia was likely from an increased catecholamine state from his recent trauma. Of note, the patient last received metoprolol 12 hours prior to the pause and morphine sulfate three hours prior.
Increased vagal tone/parasympathetic activity can be associated with hiccups, and hiccups have been reported to cause bradyarrhythmias. Due to the transient nature of the patient’s hiccups and the absence of bradycardic symptoms a permanent pacemaker was not indicated or offered to the patient. The metoprolol dose was continued at the same dose and the patient experienced no further bradyarrhythmias or hiccups for the remainder of the hospitalization. An outpatient Holter monitor did not reveal any recurrence of the bradyarrhythmias and the patient remains asymptomatic.
DISCUSSION
Bradyarrhythmias in hospitalized patients can occur from a multitude of causes, including intrinsic conduction system disease, medications, and maneuvers that increase parasympathetic activity (e.g. tracheal suctioning, bowel movements, cough). A comprehensive history is essential in the evaluation of a patient with a bradyarrhythmia.
Our patient initially presented with chest and pelvic trauma. There was no evidence of blunt myocardial injury (BMI) by transthoracic echocardiogram. Ventricular arrhythmias are common with BMI while atrial arrhythmias and bradyarrhythmias are less frequent. The patient was given two medications (metoprolol and morphine) that can contribute to bradyarrhythmias. However, both of these medications were continued after the bradycardic event, and no recurrences of bradyarrhythmia were seen. The simultaneous occurrence of violent hiccups during the bradyarrhythmia makes the hiccups the likely cause of the pause.
A hiccup, or singultus, results from a complex motor event consisting of a sudden, simultaneous, vigorous contraction of the diaphragm and inspiratory muscles, accompanied by closure of the glottis. The rush of air colliding with the closed glottis produces the hiccup sound. Hiccups are often rhythmic in nature, and synchronous with cardiac (mid-systole) and respiratory cycles (mid-inspiration).1 They are usually benign; however, they rarely can be associated with pathology or have serious consequences.
Hiccup-induced heart block was first described by Harrington in 1969, and others have confirmed the association between hiccups and bradyarrhythmias.2–4 Transient bradyarrhythmias have been described following vagal stimulation (deep breathing, Valsalva maneuver, carotid massage, coughing, and nausea/vomiting), and increased vagal tone/parasympathetic activity is the most likely mechanism of how hiccups induce bradyarrhythmias. Hiccups can increase parasympathetic activity in several ways. Increased activity from atrial mechanoreceptors and respiratory stretch receptors can modulate parasympathetic tone. The fact that hiccups are synchronous with cardiac and respiratory cycles suggests that neural mechanisms exist between the heart, lungs, and the hiccup generator.1 In addition, hiccups mimic the Valsalva maneuver, and this is likely the mechanism that has the most influence on cardiac rhythm.4
Hiccups are usually transient in nature. Since our patient had no further bradyarrhythmias once his hiccups resolved a permanent pacemaker was not required. A careful history in this case made the diagnosis, and the patient was spared an unnecessary procedure.
CONCLUSION
Hiccups are an infrequent cause of bradyarrhythmias. Hiccup-induced Valsalva maneuver and increased parasympathetic tone is the most likely explanation for this phenomenon and the likely cause of bradyarrhythmia in this patient. When evaluating a patient with bradyarrhythmias in the hospital, the physician should be aware of this clinical entity and be diligent in evaluating for all causes of bradyarrhythmias.
Footnotes
Supervising Section Editor: David E. Slattery, MD
Submission history: Submitted October 04, 2008; Revision Received February 19, 2009; Accepted March 08, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: William M. Suh, MD, Division of Cardiology, University of California, Irvine Medical Center, 101 The City Drive, Building 53, Mail Route 81, Room 100, Orange, CA 92868-4080
Email: willsuh@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Chen BY, Vasilakos K, Boisteanu D, Garma L, Derenne JP, Whitelaw WA. Linkage of hiccup with heartbeat. J Appl Physiol. 2000;88:2159–65. [PubMed]
2. Harrington TJT, Sanctis RWD. Hiccup-induced atrioventricular block. Ann Intern Med.1969;70:105–106. [PubMed]
3. Malhotra S, Schwartz MJ. Atrioventricular asystole as a manifestation of hiccups. J Electrocardiol. 1995;28:59–61. [PubMed]
4. Agarwal SK, Das D. Possible termination of ventricular bigeminy by hiccups. Postgrad Med. 1980;67:165–168. [PubMed]


