| Author | Affiliation |
|---|---|
| Delia L. Lang, PhD, MPH | Emory University, Rollins School of Public Health, Department of Behavioral Sciences and Health Education, Atlanta, GA |
| Jessica M. Sales, PhD | Emory University, Rollins School of Public Health, Department of Behavioral Sciences and Health Education, Atlanta, GA |
| Laura F. Salazar, PhD | Emory University, Rollins School of Public Health, Department of Behavioral Sciences and Health Education, Atlanta, GA |
| James W. Hardin, PhD | Medical University of South Carolina, Department of Epidemiology, Charleston, SC |
| Ralph J. DiClemente, PhD | Emory University, Rollins School of Public Health, Department of Behavioral Sciences and Health Education, Atlanta, GA |
| Gina M. Wingood, ScD, MPH | Emory University, Rollins School of Public Health, Department of Behavioral Sciences and Health Education, Atlanta, GA |
| Eve Rose, MSPH | Emory University, Rollins School of Public Health, Department of Behavioral Sciences and Health Education, Atlanta, GA |
ABSTRACT
Introduction:
African-American women are affected by disproportionately high rates of violence and sexually transmitted infections (STI)/human immunodeficiency virus (HIV) infection. It is imperative to address the intersection of these two urgent public health issues, particularly as these affect African-American adolescent girls. This study assessed the prevalence of rape victimization (RV) among a sample of African-American adolescent females and examined the extent to which participants with a history of RV engage in STI/HIV associated risk behaviors over a 12-month time period.
Methods:
Three hundred sixty-seven African-American adolescent females ages 15–21, seeking sexual health services at three local teenager-oriented community health agencies in an urban area of the Southeastern United States, participated in this study. Participants were asked to complete an audio computer-assisted self-interview (ACASI) at baseline, 6- and 12-month follow-up. We assessed sociodemographics, history of RV and sexual practices. At baseline, participants indicating they had experienced forced sex were classified as having a history of RV.
Results:
Twenty-five percent of participants reported a history of RV at baseline. At 6- and 12-months, victims of RV had significantly lower proportions of condom-protected sex (p=.008), higher frequency of sex while intoxicated (p=.005), more inconsistent condom use (p=.008), less condom use at last sex (p=.017), and more sex partners (p=.0001) than non-RV victims. Over the 12-month follow-up period, of those who did not report RV at baseline, 9.5% reported that they too had experienced RV at some point during the 12-month time frame.
Conclusion:
African-American adolescent females who experience RV are engaging in more risky sexual behaviors over time than non-RV girls, thereby placing themselves at higher risk for contracting STIs. In light of the results from this unique longitudinal study, we discuss considerations for policies and guidelines targeting healthcare, law enforcement and educational and community settings. The complexities of RV screening in healthcare settings are examined as is the need for tighter collaboration between healthcare providers and law enforcement. Finally, we consider the role of prevention and intervention programs in increasing awareness about RV as well as serving as an additional safe environment for screening and referral.
INTRODUCTION
Due to jeopardized health of adult and adolescent women, the intersection of gender-based violence and increased risk for acquiring sexually transmitted infections (STIs), including human immunodeficiency virus (HIV), has received increased attention in public health research.1 The United Nations Declaration on Violence Against Women provides a broad basis for defining gender-based violence, which includes but is not limited to physical, sexual, and psychological violence, sexual abuse of female children, marital rape, non-spousal violence, sexual harassment, trafficking in women and forced prostitution. Globally, girls and women face systematic discrimination, leaving them highly vulnerable to being harmed physically, psychologically and moreover sexually by the men in their families and communities.2
In the United States (U.S.), women experience high rates of sexual violence. According to results from the National Violence Against Women Survey (NVAWS), nearly one in six women surveyed reported having been raped in their lifetime, a prevalence of 17.6%.3 Furthermore, research suggests that in nearly two-thirds of cases, rape victimization (RV) was perpetrated by someone the victim knew (e.g. friends, acquaintances, or intimate partners) with over 50% of victims reporting that the rape occurred before age 18.3,4 While RV rates are alarming, data also indicate that only one in five women reported their rape to authorities, suggesting that available data on RV represent a severe underestimate.3
Retrospective studies in the U.S. examining physical and/or sexual victimization have shown that women’s experiences of victimization during childhood and/or adolescence are associated with high-risk sexual practices in adulthood and the acquisition of STIs, including HIV. 5–13 Among African-American adult women specifically, experiences of SV in childhood and/or adolescence are associated with increased risk for abortion, re-experiencing abuse as an adult, acquiring an STI, earlier sexual debut, a greater number of lifetime sexual partners, and sex trading.7,8,14–16
Among adolescent females, studies examining the association between RV and STI/HIV-associated risk behaviors suggest a similar pattern of associations as those described for adult women. Studies based on representative samples of adolescent females report that approximately one in five girls has experienced some form of victimization.17,18 Among sexually active adolescent girls, this rate increases to approximately one in three girls with African-American adolescent females reporting higher rates of physical or sexual victimization compared to other ethnic groups.19–23 Many adverse psychological and physical health outcomes have been found to be associated with early experiences of RV, including eating disorders, decreased self-esteem and poor health-related quality of life.17,24–27 Adolescent females with a history of RV also report engaging in high risk sexual practices including having multiple sexual partners, earlier sexual debut, not using birth control at last intercourse, substance abuse, and exchanging sex for money or drugs.16,20,28–39 Moreover, studies have reported a link between RV and self-reported STIs, whereas one recent study with female detained adolescents showed that victimization was related both directly and indirectly to biologically-confirmed chlamydia.18,19,32,40 Indirectly, physical or sexual victimization was related to chlamydia through condom failures and having sex while intoxicated.
Among adolescents, African-American females continue to represent a vulnerable group bearing the disproportionate burden of STI/HIV infection.41–44 Specifically, the prevalence of chlamydia and gonorrhea is substantially higher among same-age African-American adolescent females compared to females from other ethnic groups.45,46 Furthermore, previous studies have observed that among African-American females, even after adjusting for diverse behavioral and sociodemographic risk indices, the reinfection rate was threefold that among white peers.42,47–50 This could be due to a combination of factors including lack of adoption of STI/HIV-preventive strategies, such as using condoms consistently or limiting number of sex partners and/or selecting partners from high risk sexual networks.46,51,52
Taken together, these studies suggest that examining the intersection of RV and sexual risk taking among African-American females at high risk for STI/HIV acquisition is not only timely but also necessary given the scarce body of prospective research in this area. For purposes of this study, RV is defined as non-consensual sex during childhood or adolescence. RV is a particularly harmful type of gender-based violence associated with the most enduring health consequences, such as STI/HIV acquisition and associated risk behaviors.5,7,17,33,53,54 The purpose of this study was to describe the prevalence of RV in a population of African-American adolescent females seeking STI services, and to longitudinally assess the extent to which African-American adolescent females with a history of RV engage in STI/HIV associated risk behaviors over a 12-month time period.
METHODS
Participants
Participants in this study were part of a randomized controlled trial evaluating a sexual risk reduction intervention for young African-American females in an urban area of the Southeastern U.S. From March 2002 through August 2004, recruiters screened self-identified young African-American females seeking reproductive and sexual health services at three local teenager-oriented community health agencies. Eligibility criteria included being African-American, female, 15 to 21 years of age, and sexually active (reporting vaginal intercourse in the previous 60 days). The local institutional review board approved the study protocol before implementation.
Of 1,558 screened, 874 females met eligibility criteria. Of those who met eligibility criteria, 82% (n=715) agreed to participate, provided written informed consent, and completed a baseline assessment. Of those who agreed to participate, 348 (48.7%) were randomly assigned to the sexual risk reduction intervention condition while 367 (51.3%) were randomly assigned to a standard-of-care comparison condition. Analyses reported in this study addressed data from participants who were randomized to the standard-of-care comparison condition only to eliminate any effects of the intervention on high risk sexual behaviors. We obtained high retention rates (86%) at both 6- and 12-month follow ups for this sample.
Procedures
Data collection consisted of a 40-minute survey administered via audio computer-assisted self-interviewing (ACASI) technology at baseline, 6-month and 12-month follow-up time periods. Questions assessed sociodemographic information, history of RV, condom use behaviors and other variables describing participants’ sexual history. Participants were compensated $50 for their participation at each assessment time point.
Measures
History of Rape Victimization
History of RV was conceptualized as an index comprising two severe forms of abuse—forced vaginal intercourse or forced anal intercourse—and was assessed by asking two questions: “Has anyone ever forced you to have vaginal sex when you didn’t want to?” and “Has anyone ever forced you to have anal sex when you didn’t want to?” Response choices were yes (1) and no (0). Participants who endorsed either of these two questions were categorized as having a history of rape victimization. Participants who did not endorse either of these two questions were categorized as having no history of rape victimization.
Sociodemographic and Background Measures
We assessed highest grade completed in school by a single question, “What was the last grade that you completed in school?” Participants were also asked if they were currently attending school. Receiving federal assistance for living expenses was assessed by four yes-or-no questions. We summed responses to each question to create an index of family aid. Participants were also asked with whom they were living at the time of assessment (i.e. family members, boyfriend, other friends). We also assessed age at first willing vaginal sex.
Condom Use
We assessed several measures of condom use. First, condom use during the last episode of vaginal intercourse with a sex partner was assessed. Condom use at last intercourse provides an assessment of recent condom use that may be less susceptible to recall bias.55Participants were asked the question “Did you use a condom the last time you had vaginal sex with your boyfriend or steady partner?” Response choices were yes or no. Second, we assessed consistent condom use by asking participants the question “How many times did you have vaginal sex in the past 60 days?” Participants were then asked “How many of these times did you use a condom?” Based on these two questions we computed a continuous measure, proportion of condom use in the last 60 days, with possible values ranging from 0 to 100% condom use. Furthermore, we subsequently computed a dichotomous measure. Participants who indicated using condoms during every episode of vaginal intercourse in the past 60 days (100%) were defined as consistent condom users. Participants who indicated not using condoms during every episode of vaginal intercourse (0–99%) were defined as inconsistent condom users.
Unprotected Vaginal Sex
We assessed unprotected vaginal sex by subtracting the number of times a participant used condoms in the past 60 days from the number of times they reported having vaginal sex in the past 60 days.
Number of Sexual Partners
We assessed number of sexual partners by asking participants: “In the past 60 days, how many guys have you had vaginal sex with?” This measure was then dichotomized into participants who reported one sexual partner in the past 60 days and participants who reported two or more sexual partners.
Sex Under the Influence of Drugs or Alcohol
We assessed number of vaginal sex episodes while the participant and their sex partner were intoxicated by the following two questions: “In the past 60 days, how many times did you have sex while high on alcohol or drugs?” and “In the past 60 days, how many times did you have sex while your partner was high on alcohol or drugs?”
Statistical Methods
First, we used descriptive statistics to summarize sociodemographic variables, prevalence of sexual violence and high risk sexual behaviors. Subsequently, we conducted bivariate analyses consisting of Chi-square and independent Student’s t-tests to examine associations between RV and potential confounding variables. Finally, we estimated multivariable population-averaged generalized estimating equation (GEE) models to examine the longitudinal relationship between RV and high risk sexual behaviors.56 We used the exchangeable correlation structure for the working correlation matrix based on an evaluation of the quasi-likelihood information criterion. A separate GEE model was constructed for each high risk sexual behavior considered.
Fitted GEE regression coefficients parameters can be interpreted as the odds or odds ratios (in logistic models analyzing dichotomous outcome variables) and means or mean differences (in linear regression models analyzing continuous outcome variables) over the entire 12-month period for an “average” participant. We computed the 95% confidence intervals around the adjusted odds ratios and adjusted mean differences and the corresponding P-value. To obtain adjusted means and mean differences, we repeatedly re-estimated models from bootstrap samples where samples were drawn with replacement at the level of the participant. For each model, we calculated adjusted means and standard errors from the collection of bootstrap results.57,58 We computed percent relative difference for continuous variables as the difference (D) between the adjusted means for victimized participants divided by the adjusted mean for non-victimized participants. Percent relative difference provides a common metric for measuring the magnitude of the difference across the various measures relative to the baseline measure. We performed analyses using Stata statistical software, version 10.
RESULTS
Descriptive and Bivariate Analyses
Three hundred sixty-seven participants between the ages of 15 and 21 participated in this study and provided baseline data (Table 1). The mean age of the participants was 17.8 (standard deviation [SD] =1.7) years. Most (67.9%) had not yet graduated from high school while the remaining 32% had completed high school and/or technical school. A total of 35.4% no longer attended school at the time of baseline assessment. Among this sample 53.4% reported that their family received some form of public assistance (i.e. welfare, Section 8 housing, food stamps). Most participants (82.3%) reported being in a current relationship with the average length of the relationship 15.11 months (SD=16.0). Ninety-two (25.1%) participants reported a history of RV at baseline. Of the participants who reported no RV at baseline, 26 (9.5%) reported RV incidence over the 12-month follow-up period. Of the participants who reported RV at baseline, 55 (59.8%) reported being re-victimized over the following 12-month period. Specifically, 14 (15.2%) reported being re-victimized at the 6-month follow up; eight (8.7%) reported being re-victimized at the 12-month follow up; and 33 (35.9%) reported being re-victimized at both the 6- and 12-month follow up.

We present descriptive statistics and bivariate associations between the predictor variable, history of RV, and demographic, as well as other potential confounding variables, in Table 1. We included only variables associated with history of RV at p≤.20 in bivariate analyses in the multivariate GEE models as confounders.59 Furthermore, we present bivariate comparisons between RV history and sexual risk taking at each of the three time points (baseline, 6-months and 12-months) in Table 2.

Multivariate Analyses
We present results of GEE models constructed for continuous and dichotomous measures of sexual behaviors over the entire 12-month time period in Table 3. Analyses of continuous behavioral outcomes suggest that over the entire time period participants with a history of RV compared to participant without a history of RV reported significantly lower proportion condom use in the past 60 days (adjusted mean 21.45 vs. 31.57; p=.008), greater frequency of having sex while they were intoxicated (adjusted mean 2.30 vs. 1.30; p=.005) and greater frequency of having sex while their partner was intoxicated (adjusted mean 3.25 vs. 1.95; p=.005). Frequency of unprotected vaginal sex in the past 60 days was only marginally significant (p=.088).
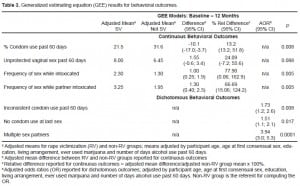
Analyses of dichotomous behavioral outcomes suggest that over the entire 12-month time period, participants with a history of RV compared to participant without a history of RV were 1.7 times more likely to report using condoms inconsistently (95%CI =1.15, 2.60; p=.008), 1.5 times more likely to report using no condoms at last sex (95%CI = 1.08, 2.11; p=.017), and 3.94 times more likely to report having multiple partners (95%CI = 2.96, 5.26; p=.0001).
DISCUSSION
In this sample of sexually active African-American adolescents one in four females reported a history of RV. These findings corroborate rates of RV reported in prior research with African-American adolescent females.18,60,61 Furthermore, results of this study show that African-American adolescent females seeking services at local STI clinics and who have a history of RV report an earlier age of consensual sex and are engaging in more risky sexual behaviors as they age than their counterparts who do not report a history of RV, thereby placing themselves at increased risk for contracting STIs, including HIV. These findings extend prior cross-sectional research reporting similar findings by underscoring the enduring adverse effects of RV on victims’ sexual risk taking over time.18,20,31,38,40, 60,61 Specifically, in this sample, African-American adolescent females with a history of RV reported less condom use with their sex partner, more frequent substance use during sexual intercourse, and multiple sex partners over a 12-month period. While we found no association in this sample between history of RV and testing positive for an STI, all of the risk behaviors aforementioned have been previously identified as antecedents to STI acquisition among African-American adolescent females.18
Understanding the relation between history of RV and risk behaviors has been hindered in previous research due to the cross-sectional nature of the study designs. As a result, two general explanations of this association have been offered in the literature: 1) following experiences of RV, women are more likely to engage in a pattern of risk behaviors and 2) engaging in risk behaviors may increase women’s risk of experiencing RV.62 Although both explanations have received some support in the literature with regard to the association between RV and substance use behaviors, less is known about the temporal association between RV and sexual risk taking.63–65 The longitudinal nature of our analyses, although not allowing for cause-effect conclusions to be drawn, lend some support to the explanation that experiences of RV are associated with a pattern of high risk sexual behaviors over time. This pathway is also consistent with a model designed to explain violence-related health problems which states that violent assaults, including sexual assaults, can lead to various adverse health outcomes, including acute physical injury, increased stress, psychological and emotional problems and subsequently high risk health behaviors.66 For victims of RV particularly, studies have shown that the psychological sequelae may include low self-esteem, passivity, depression, post-traumatic stress disorder and feelings of powerlessness and helplessness.67–70
Taken together, these psychological problems, if unresolved through professional counseling, are likely to contribute to victims’ participation in high risk sexual behaviors, such as being less likely to communicate about sex and negotiate safer sex practices which may subsequently lead to inconsistent condom use out of fear that such assertiveness may provoke aggression and possibly repeat victimization.31,71 Moreover, following experiences of RV, sexual activity may become less pleasurable.72 It is reasonable to assume that for victims of RV who view sexual activity as aversive, substance use may become a coping mechanism, allowing them to engage in sexual intercourse while alleviating negative emotions associated with RV.18,62 Unfortunately, this negative coping mechanism of using substances during sex may further exacerbate adolescent females’ risk for contracting an STI including HIV, as using substances during sex has been related to an increased risk of condom failures.39 Condom failures, such as breakage and slippage, may be more important than other risk behaviors such as unprotected vaginal sex when examining predictors of STI acquisition. Findings from a recent study showed that biologically-confirmed STIs were not related to unprotected vaginal sex among a sample of adolescent females; however, after adjusting the measure of unprotected vaginal sex to account for imperfect condom use (i.e., controlling for breakage, leaking, and slippage), the association was significant.73 In the present study, we did not find a relation between victimization and STIs; however, it may be possible that other factors could account for an indirect relation. Future research should examine more complex models that include indirect effects and measures of condom failures to account for STI outcomes. This line of research could help shed light on the complex relations among experiences of RV, sexual risk behaviors and STI/HIV outcomes.
Lastly, consistent with prior findings, our study suggests that victims of RV are more likely to report multiple sex partners than those without a history of RV.18,74,75 It is possible that because victims of RV initiate sexual activity earlier than non-victims, this may lead to exploring sexual behavior with a greater number of sexual partners during the course of adolescence. Additionally, several studies have found an association between history of RV and prostitution among 13–18-year-old predominantly African-American adolescents.76 Thus, transactional sex experiences may contribute to the higher number of sex partners reported by victims of RV in this sample.
LIMITATIONS
This study has several noteworthy limitations. First, the conceptualization of RV used in this study is rather limited in scope, including only severe sexual violence (i.e. forced vaginal and anal intercourse) and not other forms of sexual violence, such as attempted rape, digital penetration or penetration with a foreign object. Therefore, it is possible that participants categorized as “not victimized” included some who may have experienced types of RV other than those assessed by this measure. Future studies should broaden this definition to assess the effects of a full range of RV on sexual risk taking over time. Second, this study did not assess the victim-perpetrator relationship; therefore, no comparisons could be made between RV perpetrated by a sexual partner vs. RV perpetrated by a family member or a stranger. Moreover, no data were available regarding the frequency, severity or chronology of victimization. Finally, although this study adds to the literature by assessing RV and risk behavior longitudinally, no cause-effect conclusions can be drawn from these findings.
CONCLUSION
It is critically important to identify and intervene with girls who have experienced RV in an attempt to avoid a trajectory of sexual risk-taking and further re-victimization. To that end, policies and guidelines should be considered at several critical structural levels including: 1) healthcare, 2) law enforcement and 3) community education.
First, healthcare agencies, especially those serving adolescent female populations, should adopt screening guidelines for providers as standard practice. Having said that, it should be acknowledged that screening for RV, although a logical recommendation, could be complex in its implementation, especially among adolescent populations. For example, adolescent females may be accompanied to the clinic by the perpetrator in cases where RV or other types of violence are ongoing. In such cases, screening a victim may be ineffective at best and dangerous at worst. Furthermore, in the absence of being fully autonomous, adolescents’ ability to take advantage of available services targeting RV may be dependent on family members, who may or may not know about the victimization, and their level of support. However, despite its complexities, when implemented with caution, screening remains one of the best methods to protect adolescent females from ongoing RV and/or the sequelae of having experienced RV in the past. Agencies may consider implementing an overall health screening protocol that is conducted in private with only the patient and healthcare provider(s) in the consulting room. A thorough health screen would incorporate questions about both sexual risk behaviors, focusing particularly on condom use practices, frequency of sex while under the influence of substances and number of sex partners, as well as history of RV. Drawing on clinical judgment, providers may follow up with questions about current RV, should patients’ answers to previous inquiries be affirmative. Policies and guidelines must also be considered in the training of healthcare providers and their support staff. Resources should be readily available to make referrals; however, health agencies should consider implementing policies that place the adolescent female victim in a collaborative relationship with in-house staff who actively seek to connect her to targeted services for victims of RV in an effort to increase the likelihood of safe follow through. Additionally, training providers and staff to establish rapport with victims and adhere to strict confidentiality standards is a crucial consideration likely to impact both the probability of eliciting truthful responses as well as the safety of the patient. Finally, healthcare providers should also be linked to and collaborate with law enforcement agencies in instances where victims decide to report the victimization.
Second, policies and guidelines should address the needs of law enforcement agencies in an effort to expand services offered to victims of RV. Additional resources would allow enhanced training of law enforcement staff to work closely and collaboratively with healthcare agencies toward establishing sex crime reporting procedures designed to assure young women that they will be met with respect, sensitivity and timely consideration in reporting their experience(s) of victimization.
Third, policies and guidelines should be implemented in community educational settings to raise awareness of RV and associated consequences for adolescent females. Specifically, the implementation of existing sexual risk reduction and pregnancy prevention programs should incorporate sexual assault awareness into their protocols and offer treatment referrals to participants. Similarly, intervention programs for victims targeting the enduring effects of RV on sexual risk taking and the risk for re-victimization are needed and should be implemented within existing treatment plans addressing the needs of RV victims. As such, well designed intervention programs can serve a dual purpose: first, to raise awareness among both female and male adolescents in an attempt to prevent RV; and second, to serve as an additional safe environment where victims can feel comfortable reporting their experiences of RV. For many adolescent female victims of RV, such a setting may represent the first step toward prevention of increased sexual risk taking as well as possible re-victimization.
Footnotes
Supervising Section Editor: Monica H. Swahn, PhD, MPH
Submission History: Submitted January 5, 2011; Revision received February 18, 2011; Accepted February 25, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem.
Address for Correspondence: Delia L. Lang
Emory University, 1518 Clifton Rd. #548 Atlanta, GA 30322
Email: dlang2@emory.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Maman S, Campbell J, Sweat MD, et al. The intersections of HIV and violence:Directions for future research and interventions. Soc Sci and Med. 2000;50:459–78. [PubMed]
2. United Nations Declaration on Violence Against Women. United National General Assembly. 1997.
3. Tjaden NJ, Thoennes N. Extent, Nature, and Consequences of Rape Victimization. Washington, DC: National Institute of Justice, and Atlanta: Centers for Disease Control and Prevention; 2006.
4. Rand MR. Criminal Victimization. Rockville (MD): U.S. Department of Justice; 2007. 2008. Dec, Report No.: NCJ 224390.
5. Gellert GA, Durfee MJ. HIV infection and child abuse. N Engl JMed. 1989;321(10):685. [PubMed]
6. Zierler S, Feingold LI, Laufer D, et al. Adult survivors of childhood sexual abuse and subsequent risk of HIV infection. Am J Public Health. 1991;81(5):572–5. [PMC free article] [PubMed]
7. Wingood GM, DiClemente RJ. Child sexual abuse, HIV sexual risk, and gender relations of African-American women. Am J Prev Med. 1997;13(5):380–4. [PubMed]
8. Wyatt GE. The relationship between child sexual abuse and adolescent sexual functioning in Afro-American and white American women. Ann N Y Acad Sci. 1988;528:111–122. [PubMed]
9. Johnson PJ, Hellerstedt WL. Current or past physical or sexual abuse as a risk marker for sexually transmitted disease in pregnant women. Perspectives on Sexual and Reproductive Health.2002;34(2):62–7. [PubMed]
10. Martin SL, Matza LS, Kupper LL, et al. Domestic violence and sexually transmitted diseases: The experience of prenatal care patients. Public Health Reports. 1999;114:262–8. [PMC free article][PubMed]
11. Molitor F, Ruiz JD, Klausner JD, et al. History of forced sex in association with drug use and sexual HIV risk behaviors, infection with STDs, and diagnostic medical care: Results from the Young Women Survey. J Interpersonal Violence. 2000;15:262–278.
12. Wyatt G, Myers HF, Williams JK, et al. Does a history of trauma contribute to HIV risk for women of color? Implications for prevention and policy. Am J Public Health. 2000;92:660–5.[PMC free article] [PubMed]
13. Hogben M, Gange SJ, Watts DH, et al. The effect of sexual and physical violence on risky sexual behavior and STDs among a cohort of HIV seropositive women. AIDS Beh. 2000;4:353–361.
14. Fiscella K, Kitzman HJ, Cole RE, et al. Does child abuse predict adolescent pregnancy? Pediatrics.1998;101:620–9. [PubMed]
15. Miner MH, Flitter JM, Robinson BE. Association of sexual victimization with sexuality and psychological function. J Interpersonal Violence. 2006;21:503–524.
16. Senn TE, Carey MP, Vanable PA. Childhood and adolescent sexual abuse and subsequent sexual risk behavior: Evidence from controlled studies, methodological critique, and suggestions for research. Clinical Psychological Review. 2008;28:711–735.
17. Silverman JG, Raj A, Mucci LA, et al. Dating violence against adolescent girls and associated substance use, unhealthy weight control, sexual risk behavior, pregnancy, and suicidality. JAMA.2001;286:572–9. [PubMed]
18. Upchurch DM, Kusunoki Y. Associations between forced sex, sexual and protective practices, and sexually transmitted diseases among a national sample of adolescent girls. Women’s Health Issue. 2004;14(3):75–84.
19. Decker MR, Silverman JG, Raj A. Dating violence and sexually transmitted disease/HIV testing and diagnosis among adolescent females. Peds. 2005;116:e272–6.
20. Raj A, Silverman JG, Amaro H. The relationship between sexual abuse and sexual risk among high school students: Findings from the 1997 Massachusetts Youth Risk Behavior Survey. Maternal and Child Health J. 2000;4:125–134.
21. Malik S, Sorenson SB, Aneshensel CS. Community and dating violence among adolescents: perpetration and victimization.//idotecHeaft/i. 1997;21:291–302. [PubMed]
22. Foshee L, Linder GF, Bauman KE, et al. The Safe Dates Project: theoretical basis, evaluation design, and selected baseline findings. Am J Prev Med. 1996;12:39–47. [PubMed]
23. Wingood GM, DiClemente RJ, Harrington KF, et al. Efficacy of an HIV prevention program among female adolescents experiencing gender-based violence. Am J Public Health. 2006;96:1085–1090.[PMC free article] [PubMed]
24. Ackard D, Neumark-Sztainer D. Date violence and date rape among adolescents: Associations with disordered eating behaviors and psychological health. Child Abuse & Neglect. 2002;26:455–73.[PubMed]
25. Molidor C, Tolman R. Gender and contextual factors in adolescent dating violence. Violence Against Women. 1998;4:180–194. [PubMed]
26. O’Keefe M, Treister L. Victims of dating violence among high school students. Are the predictors different for males and females? Violence Against Women. 1998;4:195–223. [PubMed]
27. Coker AL, McKeown RE, Sanderson M, et al. Severe dating violence and quality of life among South Carolina high school students. Am J Prev Med. 2000;19:220–6. [PubMed]
28. El-Bassel N, Gilbert L, Krishnan S, et al. Partner violence and sexual HIV-risk behaviors among women in an inner-city emergency department. Violence Viet. 1998;13:377–393.
29. Gielen AC, McDonnell KA, O’Campo P. Intimate partner violence, HIV status and sexual risk-reduction. AIDS Behav. 2002;6:107–16.
30. Kalichman SC, Williams EA, Cherry C, et al. Sexual coercion, domestic violence, and negotiating condom use among low-income African-American women. Women’s Health. 1998;7:371–8.
31. Wingood GM, DiClemente RJ. Rape among African-American women: sexual, psychological and social correlates predisposing survivors to risk of STD/HIV. J Women’s Health. 1998;7:77–84.
32. Wingood GM, DiClemente RJ, Hubbard McCree D, et al. Dating violence and African-American adolescent females’ sexual health. Peds. 2002;107(5):E72–5.
33. Wingood GM, DiClemente RJ. The effects of an abusive primary partner on the condom use and sexual negotiation practices of African-American women. Am J Public Health. 1997;87:1016–8.[PMC free article] [PubMed]
34. Luster T, Small SA. Sexual abuse history and number of sex partners among female adolescents.Family Planning Perspectives. 1997;29:204–211. [PubMed]
35. Nagy S, DiClemente RJ, Adcock AG. Adverse factors associated with forced sex among southern adolescent girls. Peds. 1995;96:944–6.
36. Campbell JC, Baty ML, Ghandour RM, et al. The intersection of intimate partner violence against women and HIV/AIDS: a review. International J Injury Control & Safety Promotion.2008;15(4):221–231.
37. Stock JL, Bell MA, Boyer DK, et al. Adolescent pregnancy and sexual risk-taking among sexually abused girls. Family Planning Perspectives. 1997;29:200–3. [PubMed]
38. Shrier LA, Pierce JD, Emans J, et al. Gender differences in risk behaviors associated with forced or pressured sex. Archives of Ped and Adolesc Med. 1998;152:57–63.
39. Boyer D, Fine D. Sexual abuse as a factor in adolescent pregnancy and child maltreatment. Family Planning Perspectives. 1992;24:4–19. [PubMed]
40. Salazar LF, Crosby RA, DiClemente RJ. Exploring the mediating mechanism between gender-based violence and biologically confirmed Chlamydia among detained adolescent girls. Viol Against Women. 2009;15:258–275.
41. Berman S, Hein K. Adolescents and STDs. In: Holmes K, Sparling P, Mårdh P-A, et al., editors.Sexually Transmitted Diseases. 3rd ed. New York: McGraw-Hill; 1999. pp. 129–142.
42. Fortenberry JD, Brizendine EJ, Katz BP, et al. Subsequent sexually transmitted infections among adolescent women with genital infection due to Chlamydia trachomatis, Neisseria gonorrhoeae, or Trichomonas vaginalis. Sex Transm Dis. 1999;26:26–32. [PubMed]
43. Burstein GR, Gaydos CA, Diener-West M, et al. Incident Chlamydia trachomatis infections among inner-city adolescent females. JAMA. 1998;280:521–6. [PubMed]
44. DiClemente RJ, Wingood GM, Sionean C, et al. Association of adolescents’ history of Sexually Transmitted Disease (STD) and their current high-risk behavior and STD status. A case for intensifying clinic-based prevention efforts. Sex Transm Dis. 2002;29:503–9. [PubMed]
45. Ellen JM, Aral SO, Madger LS. Do differences in sexual behaviors account for the racial/ethnic differences in adolescents’ self-reported history of a sexually transmitted disease? Sex Transm Dis.1998;25:125–9. [PubMed]
46. Boyer CB, Safer M, Wibbelsman CJ, et al. Associations of sociodemographic, psychological, and behavioral factors with sexual risk and sexually transmitted diseases in teen clinic patients. J Adolesc Health. 2000;27:102–111. [PubMed]
47. Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report, Year-End Edition.Atlanta: US Department of Health and Human Services; 1999. pp. 1–44.
48. Sexually Transmitted Disease Surveillance. Centers for Disease Control and Prevention; Atlanta: US Department of Health and Human Services; 1998. 1999.
49. Eng TR, Butler WT. The Hidden Epidemic: Confronting Sexually Transmitted Diseases.Washington, DC: National Academy Press; 1997.
50. DiClemente RJ, Wingood GM, Harrington KF, et al. Efficacy of an HIV prevention intervention for African-American adolescent females: A randomized controlled trial. JAMA. 2004;292:171–9.[PubMed]
51. Hallfors DD, Iritani BJ, Miller WC, et al. Sexual and drug behavior patterns and HIV and STD racial disparities: The need for new directions. Am J Public Health. 2007;97:125–132. [PMC free article][PubMed]
52. Zierler S, Feingold LI, Laufer D, et al. Adult survivors of childhood sexual abuse and subsequent risk of HIV infection. Am J Public Health. 1991;81(5):572–5. [PMC free article] [PubMed]
53. Senn TE, Carey MP, Vanable PA, et al. Childhood sexual abuse and sexual risk behavior among men and women attending a sexually transmitted disease clinic. J Consult Clin Psychol.2006;74(4):720–731. [PMC free article] [PubMed]
54. Catania JA, Gibson DR, Chitwood DD, et al. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior.Psychol Bull. 1990;108(3):339–362. [PubMed]
55. Hardin JW, Hilbe JM. Generalized Estimating Equations. New York, NY: Chapman & Hall/CRC; 2003.
56. Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika.1986;73:13–22.
57. Efron B. Nonparametric estimates of standard error: The jackknife, the bootstrap, and other methods. Biometrika. 1981;68:589–599.
58. Hosmer DW, Lemeshow SL. Applied Logistic Regression. New York, NY: John Wiley & Sons; 1989.
59. Wyatt GE. The sociocultural context of African-American and white American women’s rape. J Social Issues. 1992;48:77.
60. Zierler S, Witbeck B, Mayer K. Sexual violence against women living with or at risk for HIV infection. Am J Prev Med. 1996;12:304. [PubMed]
61. Brener ND, McMahon PM, Warren CW, et al. Forced sexual intercourse and associated health-risk behaviors among female college students in the United States. J Consulting and Clin Psychol.1999;67(2):252–9.
62. Kilpatrick DG, Acierno R, Resnick HS, et al. Best CL. A two-year longitudinal analysis of the relationships between violent assault and substance use in women. J Consulting and Clin Psychol.1997;65:834–847.
63. Finkelson L, Oswalt R. College date rape: Incidence and reporting. Psychol Reports.1995;77:526.
64. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. [PubMed]
65. Resnick HS, Acierno R, Kilpatrick DG. Health impact of interpersonal violence: 2 medical and mental health outcomes. BehavMed. 1997;23:65–78.
66. Briere J, Runtz M. Childhood sexual abuse: Long-term sequelae and implications for psychological assessment. J Interpersonal Violence. 1993;8:312–330.
67. Kilpatrick DG, Edmunds CN, Seymour AK. Rape in America: A report to the nation. Arlington, VA: National Victim Center; 1992.
68. Hartman CR, Burgess AW. Treatment of victims of rape rauma. In: Wilson JP, Raphael B, editors.International handbook of traumatic stress syndromes. New York: Plenum Press; pp. 507–516.
69. Dutton MA. Empowering and healing the battered woman: A model for assessment and intervention. New York: Springer; 1992.
70. Sales JM, Salazar LF, Wingood GM, et al. The mediating role of partner communication skills on HIV/STD-associated risk behaviors in young African- American females with a history of sexual violence. Arch Pediatr Adolesc Med. 2008;162(5):432–8. [PubMed]
71. Wyatt GE, Riederle MH. Reconceptualizing issues that affect women’s sexual decision-making and sexual functioning. Psychol Women Q. 1994;18:611.
72. Crosby RA, Salazar LF, DiClemente RJ, et al. Accounting for failures may improve precision: Evidence supporting improved validity of self-reported condom use. Sex Transm Dis. 2005;32:513–5. [PubMed]
73. Breitchman JH, Zucker KJ, Hood JE, et al. A review of the long-term effects of child sexual abuse.Child Abuse and Neglect. 1992;16(1):101–118. [PubMed]
74. Fergusson D M, Horwood LJ, Lynskey MT. Childhood sexual abuse, adolescent sexual behaviors and sexual revictimization. Child Abuse & Neglect. 1997;21:789–803. [PubMed]
75. Cunningham RM, Stiffman AR, Dore P, et al. The association of physical and sexual abuse with HIV risk behaviors in adolescence and young adulthood: implications for public health. Child Abuse and Neglect. 1994;18:233–45. [PubMed]


