| Author | Affiliation |
|---|---|
| Rob Stephenson, PhD | Emory University, Rollins School of Public Health, Hubert Department of Global Health, Atlanta, GA |
| Alex de Voux, MS | Emory University, Rollins School of Public Health, Department of Epidemiology, Atlanta, GA |
| Patrick S. Sullivan, DVM, PhD | Emory University, Rollins School of Public Health, Department of Epidemiology, Atlanta, GA |
ABSTRACT
Introduction:
A growing body of literature suggests that men who have sex with men (MSM) represent a high risk group for human immunodeficiency virus (HIV) infection in Africa, but are often overlooked in the development of HIV interventions and programming. Little attention has been paid to the presence of intimate partner violence (IPV) among MSM in African settings. This paper examines reporting of IPV among a sample of predominantly white, gay internet-recruited MSM in South Africa and examines associations between IPV and sexual risk-taking.
Methods:
Internet-using MSM were recruited through selective placement of banner advertisements onFacebook.com. Eligibility criteria were over 18-years-old, residence in South Africa and self-reporting of recent male-male sexual behavior. There were 777 eligible respondents, of which 521 MSM with complete data are included in the final analysis. Ninety percent of the sample reported a White/ European race, and 96% self-identified as gay.
Results:
The prevalence of IPV, both experienced and perpetrated, was relatively high, with 8% of men reporting having experienced recent physical IPV and 4.5% of men reporting recent experiences of sexual IPV. Approximately 4.5% of MSM reported recently perpetrating physical IPV, while the reporting of perpetration of recent sexual IPV was much lower at 0.45%. Reporting of experiencing and perpetration of physical IPV was significantly associated with race, level of education and reporting recent unprotected anal sex. Reporting of experiencing recent sexual IPV was significantly associated with reported experiences of homophobia.
Conclusion:
There is a limited amount of data on IPV within same-sex relationships in South Africa, and the results presented here suggest that the prevalence of IPV within this White/European and gay population is cause for concern. Collection of IPV data through surveys administered via social networking sites is feasible and represents a way of reaching otherwise marginalized population groups in IPV research; although in this instance Black Africans and MSM who did not identify as gay were severely under-represented.
INTRODUCTION
South Africa is unique within the African context as the human immunodeficiency virus (HIV) epidemic was first identified among primarily white men who self-identified as gay in the 1980s, with the emergence of a second independent heterosexual epidemic in the early 1990s among the black population.1,2 Despite South Africa’s constitution and supportive legal framework, homosexuality is still highly stigmatized and considered to be “un-African.”1 In South Africa, HIV prevalence rates among men who have sex with men (MSM) have been reported to be approximately 15.3% (with a range of estimates between 12.4% to 18.3%), which is higher than the national adult prevalence rate.3In South Africa, intimate partner violence (IPV) has been shown to be an important risk factor for disease and injury, and women who experience IPV have been shown to be at an increased risk of HIV infection. 4–5 However, we find no previous research that has examined the prevalence of IPV among MSM in South Africa or has examined associations between IPV and sexual risk-taking among MSM. This paper uses data collected via surveys administered through a social network site to examine the prevalence of IPV among a sample of predominantly White/European gay-identifying MSM in South Africa and to examine the associations between reporting of IPV and reporting of sexual risk-taking. A secondary aim of this paper is to examine the feasibility of using an online questionnaire, which is marketed using a popular social networking site, to collect data on reports of both experiences as well as perpetration of intimate partner violence and sexual risk-taking behavior among MSM in South Africa.
METHODS
Internet-using MSM were recruited through selective placement of banner advertisements onFacebook.com. The banner ads included a range of images, including groups of men, individual men of a range of ethnic and racial backgrounds, and rainbow-themed images. Participants who clicked on the banner advertisements were taken to an internet-based survey. Eligibility criteria for the survey were over 18-years-old, residence in South Africa and self-report of sex with a man in the previous six months. The survey collected information on the participant’s demographic and socioeconomic characteristics (age, race, education and employment), the number of friends, colleagues or acquaintances who they felt identified as gay or bisexual, their knowledge of the routes of HIV transmission and their HIV testing behavior and sero-status. In addition, participants were asked if they had experienced or perpetrated physical IPV or sexual IPV in the 12 months prior to the survey. Men were asked if they had ever been physically hurt by their current male partner (“In the last 12 months has any partner been physically violent to you? This includes pushing, holding you down, hitting you with his fist, kicking, attempting to strangle, attacking with a knife, gun or other weapon?”), and if their current male partner had ever used physical force to coerce them to have sex when they did not want to (“In the last 12 months has any partner ever forced you to have sex when you were unwilling?). Men were also asked if they had perpetrated either physical or sexual violence against any male partner. Participants also responded to the shortened version of the Gay Identity Scale, a scale developed to measure the six stages of gay identity formation and validated with MSM in the United States (U.S.).6 Finally, respondents answered 13 questions on their experience of homophobia: the responses are summed to create a scale (0–13), with a higher score representing a greater perceived experience of homophobia. The questionnaire was reviewed by South African residents for language and cultural appropriateness. All surveys were conducted in English. Using logistic regression the reporting of experiencing physical or sexual IPV; perpetrating physical or sexual IPV and recent unprotected anal sex were modeled as outcomes. The analysis examines the likelihood of reporting either the experience or perpetration of physical and/or sexual IPV and the likelihood of reporting recent (last 12 months) unprotected anal sex as a function of a number of background characteristics, including experiences of homophobia, score on the gay identity scale, race, age, level of education, employment status and HIV serostatus.
RESULTS
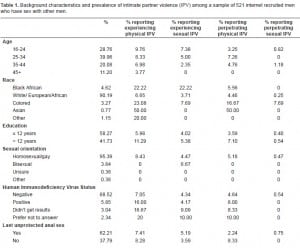
Eight hundred twenty-four individuals responded to the advertisement, of which 521 had complete data (answered all questions relevant to this analysis) and were included in the sample for data analysis. We excluded respondents from data analysis if their sex was female (n=8) or missing (n=28), if their sexual orientation was heterosexual (n=50) and if their country of residence was not South Africa (n=161) or missing (n=65).
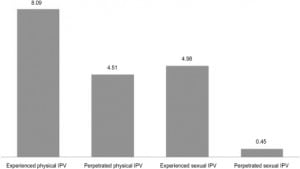
The final sample used for analysis was predominantly white (90.2%) and young (25–34 yrs) with 12 or fewer years of education. The vast majority self-identified as homosexual (95.4%) and reported to be HIV negative, although a high percentage of men reported not using a condom the last time they had anal sex. Figure 1 shows the prevalence of IPV reported among the men; 8.09% reported that they experienced physical IPV, while 4.51% reported experiencing sexual IPV. When we looked at the reporting of the IPV perpetration, 4.98% reported perpetrating physical IPV, while 0.45% reported perpetrating sexual IPV.
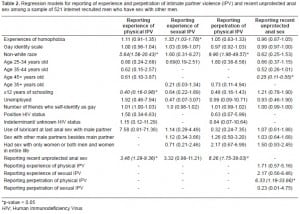
MSM who reported lower levels of education were less likely to report experiencing physical IPV (Table 2). MSM who reported a higher score on the scale measuring the experience of homophobia were significantly more likely to report experiencing sexual IPV. MSM who reported recent unprotected anal sex were more likely to report the experience and perpetration of physical IPV. MSM who reported that they had recently perpetrated physical IPV were more than six times more likely to also report a recent episode of unprotected anal sex.
DISCUSSION
The results presented here suggest that the prevalence of IPV among white, gay MSM in South Africa is similar to that among MSM in the U.S.7 However, the prevalence of violence here is significantly lower than has been reported among heterosexual females in South Africa, with estimates of intimate partner violence up to 55%.8 In this cohort of men 8.09% reported experiencing physical IPV and 4.98% reported experiencing sexual IPV which is lower than 11.75% and 7.32% reported among MSM in the U.S.7 This sample of men were predominantly white (90.2%); however, despite the small number of non-white men we still see a statistically significant positive association with report of physical IPV and race. Further investigation is required to understand the intersection between race and IPV among MSM in South Africa, as the results here are based on a small, predominantly white sample, and should be treated with caution.
The results identified a strong association between IPV and unprotected anal sex, although with cross-sectional data it is impossible to identify the nature of the relationship. Studies of IPV among heterosexual populations have identified similar relationships, and it has been argued that men who perpetrate violence may be more likely to participate in other risk-taking behavior, which may include sexual risk-taking.9 This has been hypothesized to be a pathway between violence and poor sexual health. However, further work is needed with this population to understand the nature of the relationship between IPV and sexual risk-taking.
MSM who reported experiencing homophobia were also more likely to report sexual IPV. MSM who perceive themselves to experience homophobia may be more socially isolated and have less access to social support systems, including friends, family and formal resources. This social isolation, or fear of revealing their sexual orientation, may make these MSM more vulnerable to sexual violence if potential perpetrators know that they have limited support systems. Alternatively, MSM may have experienced sexual IPV as part of a homophobic attack, and thus may also be more likely to report perceived homophobia.
The results demonstrate feasibility of using an online survey to collect data on IPV and sexual risk-taking behavior, although given the demographic biases in the sample, this method seems to be more appropriate for White, gay-identifying MSM. This method provides an alternative way of reaching White, gay-identifying MSM, since it is discreet and poses no threat for discrimination due to sexual orientation. The survey was conducted via Facebook, and in the future, online surveys must consider other websites commonly used by MSM in South Africa, which may yield a more diverse sample.
LIMITATIONS
The key limitations to the present results are a small sample size and selection bias by using an internet-based questionnaire. This has resulted in a predominantly White, gay-identifying sample, which is not representative of the South African MSM population.
CONCLUSION
The results presented here suggest that the prevalence of IPV among White, gay-identifying MSM in South Africa is a public health concern and is related to sexual risk-taking behavior, although levels of IPV are lower than have been reported in the female heterosexual population.8 It also suggests that online-based surveys are a feasible way of obtaining sensitive public health information from White, gay-identifying MSM, but other data collection mechanisms may need to be explored to reach Black Africa, and non-gay identifying MSM. There seems to be a complex interaction between the experience and perpetration of IPV, sexual risk-taking behavior and experiences of homophobia that warrants further research. More substantial surveillance and data is required within the South African MSM population in order to develop effective public health interventions.
Footnotes
Supervising Section Editor: Abigail Hankin, MD, MPH
Submission history: Submitted: January 6, 2011; Revision received March 1, 2011; Accepted March 3, 2011.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem.
Address for Correspondence: Rob Stephenson, PhD
Hubert Department of Global Health, Rollins School of Public Health, 1518 Clifton Rd., Atlanta, GA, 30322
Email : rbsteph@sph.emory.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Lane T, et al. They see you as a different thing: the experiences of men who have sex with men with healthcare workers in South African township communities. Sex Transm Infect. 2008;84(6):430–3.[PMC free article] [PubMed]
2. Maartens G, et al. Independent epidemics of heterosexual and homosexual HIV infection in South Africa–survival differences. QJM. 1997;90(7):449–54. [PubMed]
3. Baral S. International AIDS Conference. Mexico City: 2008. A systematic review of HIV epidemiology and risk factors among MSM in Sub-Saharan Africa 2000–2008.
4. Norman R, et al. Interpersonal violence: an important risk factor for disease and injury in South Africa. Popul Health Metr. 8(1):32. [PMC free article] [PubMed]
5. Jewkes R, et al. Factors associated with HIV sero-status in young rural South African women: connections between intimate partner violence and HIV. Int J Epidemiol. 2006;35(6):1461–8.[PubMed]
6. Brady S, Busse WJ. The gay identity questionnaire: a brief measure of homosexual identity formation. J Homosex. 1994;26(4):1–22. [PubMed]
7. Stephenson R, Khosropour C, Sullivan P. Reporting of intimate partner violence among men who have sex with men in an online survey. West J Emerg Med. 2010;11(3):242–6. [PMC free article][PubMed]
8. Dunkle KL, Jewkes RK, Brown HC, et al. Prevalence of patterns of gender-based violence and revictimization among women attending antenatal clinics in Soweto, Sout Africa 2004. [PubMed]
9. Garcia-Moreno C, Watts C. Violence against women: Its importance for HIV/AIDS prevention.AIDS. 2000;24(3):S253–S265. [PubMed]


