| Author | Affiliation |
|---|---|
| Gavin Budhram, MD | Baystate Medical Center, Tufts University School of Medicine |
| Tala Elia, MD, RDMS | Baystate Medical Center, Tufts University School of Medicine |
| Niels Rathlev, MD | Baystate Medical Center, Tufts University School of Medicine |
Introduction
Methods
Results
Discussion
Limitations
Conclusions
ABSTRACT
Introducion:
With the rapid expansion of emergency ultrasound, resident education in ultrasound has become more clearly developed and broadly integrated. However, there still exists a lack of guidance in the training of physicians already in practice to become competent in this valuable skill. We sought to employ a step-wise, goal-directed, incentive-based credentialing program to educate emergency physicians in the use of emergency ultrasound. Successful completion of this program was the primary outcome.
Methods:
The goal was for the physicians to gain competency in 8 basic ultrasound examinations types: aorta, focused assessment with sonography in trauma, cardiac, renal, biliary, transabdominal pelvic, transvaginal pelvic, and deep venous thrombosis. We separated the 2.5 year training program into 4 distinct blocks, with each block focusing on 2 of the ultrasound examination types. Each block consisted of didactic and hands-on sessions with the goal of the physician completing 25 technically-adequate studies of each examination type. There was a financial incentive associated with completion of these requirements.
Results:
A total of 31 physicians participated in the training program. Only one physician, who retired prior to the end of the 2.5 year period, did not successfully complete the program. All have applied for and received hospital privileging in emergency ultrasound and incorporated it into their daily practice.
Conclusion:
We found that a step-wise, incentive-based ultrasound training program with a combination of didactics and ample hands-on teaching was successful in the training of physicians already in practice.
INTRODUCTION
Emergency ultrasound (EUS) has grown rapidly over the last 10–15 years, and is now a commonplace tool in academic and community emergency departments (ED). Literature describing the role of ultrasound in improved patient outcomes, decreased ED length of stays, decreased costs, and decreased procedural complications is ubiquitous.1–6 As the use of EUS has increased, however, so has the need to assure that practicing clinicians are properly trained to competently obtain and interpret ultrasound images, as well as to integrate ultrasound effectively into patient care.
Much has been previously published on the training of emergency medicine residents in ultrasound. A combination of didactics and hands-on teaching has proven effective. 7–12 There is, however, a general lack of guidance for those seeking to train physicians already in practice and without any previous ultrasound experience. The training of practicing clinicians is inherently different than residents. Residents do not practice according to long-established patterns, so implementing a new diagnostic tool is less challenging. Years of clinical practice patterns can be difficult to change. Second, residents have dedicated time incorporated into their program for learning new skills. Practicing clinicians are often unwilling to devote additional time when not working in the ED, and secondary incentives may be needed. Even for those physicians eager to learn ultrasound, it can be challenging to incorporate this new skill under the pressures of a crowded and busy shift. Finally, residency is geared toward the successful acquisition of a comprehensive skill for the practice of emergency medicine, and ultrasound is taught along with a complement of other skills.
A common training tool for practicing clinicians is a 1–3 day ultrasound course, which includes lectures and hands-on practice.13–15 These courses, however, often leave clinicians without guidance after the course is complete. Enthusiasm tends to wane and ultrasound skills deteriorate with time. It is generally accepted that strong and enthusiastic ultrasound leadership is needed to provide continued education over time.7,16
To our knowledge there have been no detailed, published descriptions of successful EUS training programs for practicing clinicians. In this paper, we describe a successful step-wise, goal-oriented, incentive-based ultrasound credentialing program for emergency physicians (EP) that emphasizes hands-on teaching, quality assurance, and physician feedback. The primary outcome measure is successful completion of all requirements of each training block by each physician.
METHODS
This is a descriptive study of a departmental educational program rather than a research study, and as such was exempt from institutional review board approval at our institution.
Study Setting and Population
The training program took place in a busy academic ED with 110,000 annual patient visits per year and a separate pediatric ED. The group of 33 EPs included 2 dedicated ultrasound faculty members and 6 fellowship-trained pediatric EPs. Physicians were 1–35 years post-residency completion. The emergency medicine residency consists of 12 residents per year in a 1–2–3 format. For purposes of the EUS training program, we excluded the ultrasound faculty and residents.
Four Sonosite M-turbo (Sonosite Inc, Bothell WA) emergency ultrasound machines were available 24 hours per day, each with curvilinear, linear, and phased array probes. Four endocavitary probes were also available for transvaginal pelvic examinations. An on-site wireless archiving system, developed by an EM faculty member, was used to catalog examinations for review and quality assurance purposes.
Program Description
To avoid overwhelming physicians with the technical aspects of multiple ultrasound examination types at once, we divided the training into 4 6-month discrete blocks. Two examination types were taught during each block. The blocks were as follows:
Aorta and focused assessment with sonography in trauma (FAST)
Cardiac and Renal
Biliary and Transabdominal (TA) pelvic
Transvaginal (TV) pelvic and deep venous thrombosis (DVT)
At the start of each block physicians were provided a didactic lecture introducing each examination type. These were followed by hands-on teaching sessions 3–4 times per month, in which physicians had the opportunity to practice each examination with direct supervision and teaching. Sessions were typically 2–3 hours in length and consisted of an ultrasound faculty member as well as 2–5 attendees. Patients in the ED were used for training and informed that scans were purely for educational purposes. Physicians had the opportunity to attend lectures and receive hands-on training for other examination types outside of the current block, but were not held to deadlines or incentives for those examination types until the commencement of that block.
Each physician was expected to perform 25 technically adequate examinations for each study type. These examinations were typically performed on ED patients, mostly during the course of a regular clinical shift. Physicians did perform some scans during non-clinical hours on ED patients, typically during weekly trainings sessions with ultrasound faculty, although these scans usually accounted for less than a third of their exam totals. If scans were performed in conjunction with residents, both participants were required to manipulate the transducer for the examination to count towards credentialing. Studies that were judged to be “technically inadequate” in terms of image quality were not included in their totals, and physicians were targeted for reeducation if they submitted multiple technically inadequate exams in a specific exam type.
We sought to make the process of recording and submitting images as easy as possible to enhance compliance. Still images and video clips were saved for each training exam. These were automatically and wirelessly transmitted to a central archive in the ED. Physicians were able to electronically enter their interpretation alongside their images, a process taking only a few seconds per exam. Training examinations were reviewed on a biweekly basis and direct feedback was electronically provided. Monthly updates on the number of ultrasound examinations each faculty member had successfully completed were tabulated and distributed by email.
At the completion of each block, competency in image acquisition was assessed at a bedside hands-on session with one of the ultrasound faculty. Skill in image interpretation was assessed with a 25-question quiz, including at least 10 abnormal or pathologic findings. Physicians were provided a written explanation for the questions that they missed.
Administrative Considerations
Several concerns were raised by the department of radiology regarding an EUS training program for EPs. Chief among these were the number of studies required for competency. The EPs cited published articles demonstrating that competence in bedside ultrasound can be obtained with limited training.17–22 The 2008 ACEP Ultrasound Policy Statement, which requires a minimum of 25 studies, were also cited.23 Their second concern was the potential decrease in study volume for ultrasound examinations performed in their department as a result of the EP training program. The EPs cited an article demonstrating negligible impact of an EUS program on radiology departmental volumes.24
An outline of the credentialing pathway was submitted and approved by the hospital credentialing committee before initiation of the program. We presented a written plan for the training program to the faculty members by email and again at the monthly faculty meeting. They were given a chance to disagree or voice concerns. All faculty members verbally agreed to abide by the conditions of the training program prior to beginning. Upon successful completion of each training block, physicians applied for and obtained hospital credentialing for that examination type and were eligible to begin billing for those studies.
Monetary Incentives
Faculty salaries are a combination of “base salary” (guaranteed) and “variable compensation” (not guaranteed). A total of 90% of the salary is guaranteed as base compensation, with the remaining 10% being “variable,” and dependent on various productivity and educational goals. For the 2.5-year ultrasound training period, the variable component included ED productivity and 3 weighted performance measures: timely and successful completion of each ultrasound module, compliance with national pneumonia treatment guidelines, and time to patient-physician contact after triage assessment. Meeting ultrasound requirements accounted for 6.66% of the total variable compensation package per year. During the period of the training program, total variable compensation was estimated to be $27,240 per physician per year, with $1,860 resultant from ultrasound goals. We believe that this incentive component was an important factor in assuring 100% compliance with training requirements. During the 2.5 years of training, only one faculty member failed to complete a module therefore forfeiting the incentive payment. This individual retired from practice shortly thereafter.
Cost
The approximate costs of the EUS training program are summarized in Table 1. Although variable compensation payments to physicians totaled about $125,550 and equaled 30.2% of the program costs, these incentive payments are part of each physician’s total salary package and continue for other quality measures even after completion of the EUS training program. The two ultrasound faculty were provided a total of 9 hours per week of release time for ultrasound training, with each hour requiring $6,000 of administrative funding per year. Training materials were obtained for a total of approximately $12,000. Major items included a transvaginal pelvic model ($5000), 3 transvaginal ultrasound workshops with paid live models ($4565) and central and peripheral vascular access models ($3000). The department of obstetrics and gynecology agreed to split the cost of the pelvic model since it could also be used to train their residents.
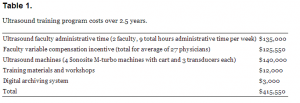
Ultrasound training program costs over 2.5 years.
Other Considerations
There were 6 full-time pediatric EM faculty who did not participate in training for the aorta, biliary, transvaginal pelvic, and DVT examinations because they believed these examinations to have limited utility in their daily practice. Other performance measures were more heavily weighted to achieve their target variable compensation. This allowance was agreed to prior to initiation of the program. All EPs treating adult patients participated in the training for each application.
To supplement training in the transvaginal pelvic examination, a Blue Phantom endocavitary training model (Blue Phantom, Redmond WA) was used. In addition, 3 workshops were held in which 3–4 female standardized patients were employed as models for transvaginal ultrasound. Standardized patients were obtained from an agency providing medical models. Faculty members that performed examinations on standardized patients had these examinations count towards their total number.
RESULTS
Baseline characteristics of the physician population before the first block are described in Table 2. Seventy-nine point two percent (23/29) of physicians had been out of training for >5 years and 62.1% (18/29) described themselves as “not comfortable with any applications of emergency ultrasound.” In those who had been out of residency >6 years, 78% (18/23) were uncomfortable with any ultrasound applications. In the group of physicians who had been out of training for 0–5 years, all stated they were comfortable with at least 1–2 applications and two thirds were comfortable with at least three. No physicians in the group were comfortable with all 8 applications of EUS.
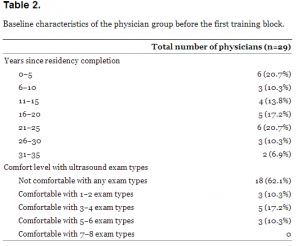
Baseline characteristics of the physician group before the first training block.
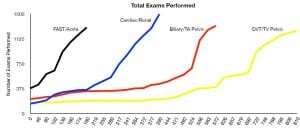
All physicians participating in a training block successfully completed the training and credentialing requirements of that block, with the exception of one who retired in the middle of a block. Results are shown in Table 3. The training period spanned 810 days, and total number of examinations were counted at regular intervals with the exception of the last month of each block when results were reported weekly. Exams were counted until each physician performed the requisite 25 studies per examination type. Several physicians had been partially credentialed for some exam types before initiation of the program, either during their residency or during less formal training at our institution. Exams previously performed at our institution had been assessed for technical adequacy and accuracy of interpretations. These exams are noted on “Day 0” of the program. The figure shows a graphical representation of each ultrasound examination type and total time needed for completion as a function of days since the beginning of the training period.
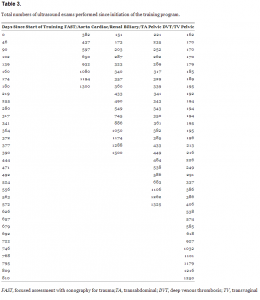
Total numbers of ultrasound exams performed since initiation of the training program.
Total numbers of ultrasound exams performed since initiation of the training program.
For the first block, 29 EPs were eligible for credentialing in the FAST examination and 23 for credentialing in the aorta examination. Four had previously finished credentialing requirements in the FAST exam and five in the aorta examination before the program began. The EPs completed a total of 1300 training examinations in 180 days.
For the second block, 1 physician left the group and another went on sabbatical. Three new physicians were added to the group. This yielded a total of 30 physicians eligible for credentialing in the cardiac examination and 30 in the renal examination. Five had previously completed requirements for credentialing in the cardiac examination and five in the renal examination. The block was extended by 1month as it became clear that a significant proportion of physicians would not be able to finish on time, so the total length of the block was 210 days. The physicians completed a total of 1500 training examinations during this time.
For the third block, one EP retired. This yielded a total of 24 EPs eligible for credentialing in the biliary examination and 29 for the transabdominal pelvic examination. Five had previously completed requirements for credentialing in the transabdominal pelvic examination and 6 in the biliary examination. The third block was 210 days. The physicians completed a total of 1325 examinations during this time.
For the fourth block, 2 physicians were hired, 1 left, and 1 returned from sabbatical. This yielded a total of 25 physicians for the transvaginal pelvic examination and 25 for the DVT examination. The last block was again extended by 2 months as it became clear that a significant proportion of physicians would not be able to finish on time, so the total length of the block was 240 days. The physicians completed a total of 1250 training examinations during this time.
During the 2-year training program, several physicians left or joined the group. Of the physicians who joined, all except for one were previously trained in EUS by their residency programs. This physician had been previously credentialed in trauma and aorta sonography and fortunately joined just as the group finished this first block. She was able to complete her training with the rest of the group. Physicians who left were provided with a letter from the ultrasound director detailing the numbers of ultrasounds completed.
In general, physicians spent an average of 1.5 hours in lecture and 3.5 hours in hands-on training for each training block.
DISCUSSION
As EUS becomes increasingly prevalent in the specialty of emergency medicine, it is important that EPs are appropriately trained in this skill. We describe the successful implementation of a structured, step-wise and incentive-based educational program geared towards EPs already in practice. Although our program was implemented in an academic ED, we believe the basic tenets of this model could be exported to community practice settings. These include structured goals and deadlines, physician incentives, adequate equipment, and appropriate time and resources for the ultrasound faculty.
At our hospital, 10% of total annual compensation is “variable,” and individual departments are allowed to apportion this towards the achievement of various productivity, educational, and quality measures. During the 2.5-year EUS training period, our department chose to define the accomplishment of ultrasound goals as a small component of the overall variable compensation package and employed this as a monetary incentive. Although it appears generous at first glance, this incentive was possible because it did not require the generation of new funds but rather a re-allocation of funds that were already budgeted for physician compensation. The authors realize that similar monetary incentives, although effective, may not be available at other institutions as compensation packages will vary. It is possible, however, that non-monetary incentives may be substituted. These might include preferential considerations in shift scheduling, vacation time, or release time for continuing medical education.
Incentives and deadlines were a key part of our training program. As demonstrated in the figure, exam totals for each examination type remained relatively stable until formal training for each block began. Even though EPs had ready access to lectures and hands-on training for other examinations throughout the entire 2.5-year period, we believe they were not motivated to accrue ultrasound exams until deadlines and incentives for each block were introduced.
A significant upswing of recorded examinations was usually noted towards the end of each block. This was partially explained by a predictable tendency to procrastinate. At this point, verbal encouragement from the ultrasound faculty, admonishment from the department chair, the possibility of losing monetary incentives, and the demonstration that other physicians were able to achieve the goals all played key roles in the successful completion of each block.
For several of the training blocks, it was necessary to extend the deadline by 1–2 months after it became evident that more than 20% would not be able to finish in time. We met with these individuals separately and provided additional hands-on training sessions. All were eventually able to meet the training requirements within the extended timeframe. Rather than penalizing a large minority of the group, we believed that a better overall outcome could be achieved by slightly extending the training period.
While initial ultrasound learning is clearly the most time and labor-intensive portion of the educational process, continuing education is crucial. We achieve this through weekly resident conferences that incorporate ultrasound material, ongoing quality assurance and feedback, a circulated “case of the week,” and bi-monthly ultrasound-dedicated conferences. Further education also included “advanced” ultrasound applications, such as thoracic, ocular, regional anesthesia, and critical care.
Two years after completion of the program, EPs in our ED perform approximately 3,700 clinically-indicated ultrasound examinations per year, averaging 0.86 scans/physician/shift (range 0.07–2.26). The department generates bills for these examinations, resulting in approximately $400,000 in hospital revenue and $64,000 in ED revenue per year. Since initiation of the program 3.5 years ago, EUS has generated $1,385,900 in hospital revenue and $224,177 in ED revenue. The total cost of the training program, $415,550, was remunerated within 1.5 years. To date, the return on investment (ROI) is 2.87. Ultrasound scans performed by newly credentialed physicians account for 73% of this activity.
There were several important lessons learned during our implementation of this program. First, for different reasons, several individuals required extra attention during the process. A few were initially intimidated by the technology and needed more coaching to approach the machine and use it daily. Some were more spatially challenged and required extra training sessions. Second, the importance of having the physicians agree to abide by conditions of the training program prior to its start became increasingly apparent towards the end of each block. Physicians who procrastinated in obtaining their training examinations were reminded of their agreement, and this provided more incentive to finish. Finally, this was a very labor-intensive undertaking for the ultrasound faculty, and it was imperative that they were adequately compensated and provided additional academic time to fulfill their duties.
LIMITATIONS
There were several potential areas of improvement with our training program. After the introduction of each block, EPs recorded a significant number of scans but that rate rapidly declined after the initial enthusiasm waned. Several routinely submitted their examinations just before the deadline. This contributed to some examinations being done with sub-standard technique and left limited time for feedback and correction. We attempted to compensate for this by adding more hands-on sessions and encouraging attendance through targeted emails.
We did not require them to re-take quizzes if they scored below a certain percentage. Although no physician scored below 70% on any quiz, a better policy might be to ask low-scoring physicians to take a second quiz with ultrasound images from different patients but with similar normal or abnormal findings. Since they were provided written explanations of answers after the first test, a second test could be used to demonstrate that they learned from their mistakes.
Our training program was not designed to track patient-oriented outcomes, although these would have been good quality measures to report. We did examine a sampling of 20 first-trimester pregnant patients that presented to the ED with vaginal bleeding or pelvic pain. These patients received both a bedside pelvic ultrasound as well as a formal study. In this group, time to diagnosis of intrauterine pregnancy (and exclusion of ectopic pregnancy) by bedside ultrasound took 32 minutes, while the formal study required an additional 111 minutes.
Since completion of the program 2 faculty members have left the institution and 3 others have joined. Before hiring the new members, it was made clear that ultrasound proficiency was a pre-requisite for working in the department. The new faculty members had all finished residency within the last 5 years and had already completed ultrasound training and demonstrated proficiency in most examination types before joining the group. Training in transvaginal pelvic ultrasound is variable in residency training programs, and 2 new hires were notably lacking in this skill. They were separately provided with didactics and hands-on training and were required to complete 25 training examinations before they could make clinical decisions based on their examinations. This time was uncompensated.
Our program had very strong support from hospital leadership and the departmental chairman. Institution of a successful incentive-based training program at other facilities without this support would be much more difficult since a significant up-front investment is required.
CONCLUSIONS
We believe this training program can be realistically implemented by clinicians in practice despite the constraints of busy clinical schedules. Using this model, we were able to train and credential 31 EPs over a 2.5-year period with nearly 100% successful completion. Although our program was fairly rigorous and time-consuming for both the physicians and ultrasound faculty, we felt it to be a worthwhile investment. We believe the end result is better ultrasound training and knowledge retention, ultimately producing better patient care.
Footnotes
Address for Correspondence: Gavin Budhram, MD, Baystate Medical Center, Tufts University School of Medicine. Email: gavin. budhram@gmail.com 11 / 2013; 14:602 – 608
Submission history: Revision received November 19, 2012; Submitted April 17, 2013; Accepted April 17, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Plummer D, Brunette D, Asinger R Emergency department echocardiography improves outcome in penetrating cardiac injury. Ann Emerg Med. 1992; 21:709-712
2. Durston WE, Carl ML, Guerra W Ultrasound availability in the evaluation of ectopic pregnancy in the ED: comparison of quality and cost-effectiveness with different approaches. Am J Emerg Med. 2000; 18:408-417
3. Blaivas M, Harwood RA, Lambert MJ Decreasing length of stay with emergency ultrasound examination of the gallbladder. Acad Emerg Med. 1999; 6:1020-1023
4. Randolph AG, Cook DJ, Gonzales CA Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996; 24:2053-2058
5. Mateer JR, Valley VT, Aiman EJ Outcome analysis of a protocol including bedside endovaginal sonography in patients at risk for ectopic pregnancy. Ann Emerg Med. 1996; 27:283-289
6. Burgher SW, Tandy TK, Dawdy MR Transvaginal ultrasonography by emergency physicians decreases patient time in the emergency department. Acad Emerg Med. 1998; 5:802-807
7. Mateer J, Plummer D, Heller M Model curriculum for physician training in emergency ultrasonography. Ann Emerg Med. 1994; 23:95-102
8. Shackford SR, Rogers FB, Osler TM Focused abdominal sonogram for trauma: the learning curve of nonradiologist clinicians in detecting hemoperitoneum. J Trauma. 1999; 46:553-562
9. Smith RS, Kern SJ, Fry WR Institutional learning curve of surgeon-performed trauma ultrasound. Arch Surg. 1998; 133:530-535
10. Heller MB, Mandavia D, Tayal VS Residency training in emergency ultrasound: fulfilling the mandate. Acad Emerg Med. 2002; 9:835-839
11. McCarter FD, Luchette FA, Molloy M Institutional and individual learning curves for focused abdominal ultrasound for trauma: cumulative sum analysis. Ann Surg. 2000; 231:689-700
12. Noble VE, Nelson BP, Sutingco AN Assessment of knowledge retention and the value of proctored ultrasound exams after the introduction of an emergency ultrasound curriculum. BMC Med Educ. 2007; 7:40
13. Heegeman DJ, Kieke B Learning curves, credentialing, and the need for ultrasound fellowships. Acad Emerg Med. 2003; 10:404-405
14. Walcher F, Kirschning T, Brenner F [Training in emergency sonography for trauma. Concept of a 1-day course program]. Anaesthesist. 2009; 58:375-378
15. Mandavia DP, Aragona J, Chan L Ultrasound training for emergency physicians–a prospective study. Acad Emerg Med. 2000; 7:1008-1014
16. Costantino TG, Satz WA, Stahmer SA Predictors of success in emergency medicine ultrasound education. Acad Emerg Med. 2003; 10:180-183
17. Jang T, Aubin C, Naunheim R Minimum training for right upper quadrant ultrasonography. Am J Emerg Med. 2004; 22:439-443
18. Kuhn M, Bonnin RL, Davey MJ Emergency department ultrasound scanning for abdominal aortic aneurysm: accessible, accurate, and advantageous. Ann Emerg Med. 2000; 36:219-223
19. Tayal VS, Graf CD, Gibbs MA Prospective study of accuracy and outcome of emergency ultrasound for abdominal aortic aneurysm over two years. Acad Emerg Med. 2003; 10:867-871
20. Ma OJ, Mateer JR, Ogata M Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995; 38:879-885
21. Mandavia DP, Hoffner RJ, Mahaney K Bedside echocardiography by emergency physicians. Ann Emerg Med. 2001; 38:377-382
22. Rosen CL, Brown DF, Sagarin MJ Ultrasonography by emergency physicians in patients with suspected ureteral colic. J Emerg Med. 1998; 16:865-870
23. ACEP emergency ultrasound guidelines-2001. Ann Emerg Med. 2001; 38:470-481
24. Soremekun OA, Noble VE, Liteplo AS Financial impact of emergency department ultrasound. Acad Emerg Med. 2009; 16:674-680


