| Author | Affiliation |
|---|---|
| Andrew L. Makowski, MD | St. Joseph’s Hospital, Department of Emergency Medicine, Milwaukee, Wisconsin |
Introduction
Methods
Results
Discussion
Limitations
Conclusions
ABSTRACT
Introduction:
The Emergency Medicine (EM) Residency Review Committee stipulates that residents perform 3 cricothyrotomies in training but does not distinguish between those done on patients or via other training methods. This study was designed to determine how many cricothyrotomies residents have performed on living patients, the breadth and prevalence of alternative methods of instruction, and residents’ degree of comfort with performing the procedure unassisted.
Methods:
We utilized a web-based tool to survey EM residents nearing graduation and gathered data regarding the number of cricothyrotomies performed on living and deceased patients, animals, and models/simulators. Residents indicating experience with the procedure were asked additional questions as to the indication, supervision, and outcome of their most recent cricothyrotomy. We also collected data regarding experience with rescue airway devices, observation of cricothyrotomy, and comfort (“0–10” scale with “10” representing complete confidence) regarding the procedure.
Results:
Of 296 residents surveyed, 22.0% performed a cricothyrotomy on a living patient, and 51.6% had witnessed at least one performed. Those who completed a single cricothyrotomy reported a significantly greater level of confidence, 6.3 (95% confidence interval [CI] 5.7–7.0), than those who did none, 4.4 (95% CI 4.1–4.7), p<<0.001. Most respondents, 68.1%, had used the recently deceased to practice the technique, and those who had done so more than once reported higher confidence, 5.5 (95% 5.1–5.9), than those who had never done so, 4.1 (95% CI 3.7–4.5), p<<0.001. Residents who practiced cricothyrotomy on both simulators and the recently deceased expressed more confidence, 5.4 (95% CI 5.0–5.8), than those who used only simulators, 4.0 (95% CI 3.6–4.5), p<<0.001. Neither utilization of models, simulators, or animals, nor observance of others’ performance of the procedure independently affected reported confidence among residents.
Conclusion:
While prevalence of cricothyrotomy and reported comfort with the procedure remain low, performing the procedure on living or deceased patients increased residents’ confidence in undertaking an unassisted cricothyrotomy upon graduation in the population surveyed. There is evidence to show that multiple methods of instruction may yield the highest benefit, but further study is needed.
INTRODUCTION
While the vast majority of patients requiring emergent airway management in the emergency department (ED) can be intubated endotracheally, those who cannot often require cricothyrotomy to provide a secure airway when other routes fail. The incidence of failed airway has been reported to be as low as 0.5%, but there exist patients who simply are unable to be intubated due to severe head or neck trauma, angioedema, or other anatomic obstacles.1,2 The development of adjunct airway devices such as gum elastic bougies, intubating laryngeal mask airways (ILMAs), and video-assisted devices has rescued many potential airway failures, but each device has its limitations. Resident education has evolved to incorporate use of these “rescue devices,” and a 2004 survey of emergency medicine (EM) program directors (PDs) revealed that 90% of programs had at least 3 different devices available in the ED. While a multitude of different adjuncts were in use, cricothyrotomy was by far the most prevalent alternative technique reported, with 86.4% of PDs indicating use in their programs.3
Most adjunct devices possess the advantage that residents can use them during routine endotracheal intubations to gain proficiency in their use. This has the benefit of allowing trainees to better appreciate the subtleties of each instrument, its indications, and its drawbacks under more controlled circumstances. Cricothyrotomy is unique in that not only is it performed rarely, but it cannot be practiced as part of routine airway management.3,4 This has left educators with a need to find unique ways to teach a procedure that is essential to know but seldom performed. While the advent of models and simulators has afforded residents opportunities to hone their skills in the lab, even high fidelity models cannot reproduce the tissue consistency, bleeding, and anatomic variation that exist in human models.3,5 Canine labs have been used, but anatomic differences between dogs and humans, expense, and concern over sacrifice of the animal are significant drawbacks.6,7,8 Using the recently deceased to teach cricothyrotomy has been advocated by many as a way to provide residents with more realistic training experiences, but this approach raises concerns regarding the best means to respect the deceased and next of kin and the necessity of and method by which consent may be obtained.9,10,11
Despite these challenges, cricothyrotomy is still taught in residency programs, and graduates are expected to be able to perform the procedure regardless of whether or not they have performed any in training.1,2,3 Surgical airway remains the final step in the American Society of Anesthesiologist’s Practice Guidelines for Management of the Difficult Airway, and emergency physicians have faced litigation for failing to perform a cricothyrotomy when intubation and rescue devices have failed.12,13,14 The Residency Review Committee (RRC) for EM stipulates that a resident shall complete at least 3 cricothyrotomies by graduation, but procedure logs do not distinguish among those performed on models/simulators, animals, the deceased, or living patients.15 Thus, the actual number of cricothyrotomies being performed by residents on living patients remains unknown.
This purpose of this study is to develop a better understanding of how residents are instructed to perform cricothyrotomy (cric), the frequency with which they observe and perform the procedure, and their degree of comfort in undertaking the procedure unassisted upon graduation.
METHODS
We surveyed EM residents scheduled to graduate in 2011 from Accreditation Council for Graduate Medical Education (ACGME) approved residencies regarding their experience with cricothyrotomy using a web-based application. This study was approved by the hospital institutional review board and deemed to be exempt from formal informed consent. The survey was piloted using a cohort of PGY1 and PGY2 residents who were not part of the population to be studied, and we used their responses and feedback to generate the final instrument.
We identified PDs via contact information on the ACGME website and e-mailed them a description of the study, a hyperlink to view a sample survey, and an e-mail to forward to their residents requesting their participation. PDs who failed to indicate whether or not they had forwarded the request to their residents were e-mailed a second time in June. We excluded only programs not graduating residents in 2011. Data collection began on May 17 and ended on June 30, 2011.
Previous research and mathematical modeling suggest that given a total population of 1,500, alpha=0.01, and margin of error=0.03, approximately 185 surveys would need to be returned to yield data on which reliable conclusions could be drawn.16 Nevertheless, oversampling was employed to increase homogeneity and to minimize effects of geography, PD participation, and other potential sampling errors upon results.
We briefed potential subjects electronically on the mechanics of data collection and the enrollment process before they began the survey. No identifying data regarding the respondent’s name, program, geographic location, or patient names were gathered. All residents answered questions regarding their level of training, opportunities to observe the procedure, and use of adjunct airway devices. Further questions asked respondents to identify the total number of cricothyrotomies they had performed personally on living and deceased humans, models/simulators, and animals, and to rate their level of comfort (“0–10” with “10” indicating complete comfort) in performing an emergent cricothyrotomy unassisted by another physician. Those who had indicated they had performed at least one cricothyrotomy on a living patient were shown additional questions regarding the circumstances and supervision of their most recent cricothyrotomy and asked to identify their level of training and previous surgical airway experience at the time the procedure occurred. Where appropriate, we included free-text response boxes to capture any additional comments respondents wished to make. No incentives, financial or otherwise, were offered to residents or PDs in exchange for participation. A portion of the survey is reproduced in Table 1.
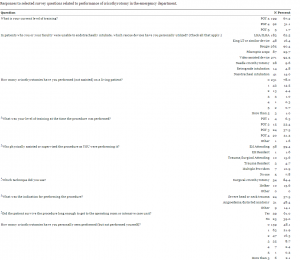
Responses to selected survey questions related to performance of cricothyrotomy in the emergency department.
Data were compiled electronically, extracted, and analyzed via SPSS (Version 18). We used one-way analyses to compare reported levels of comfort among groups. Post hoc comparisons using the Tukey HSD test were used to determine differences among pair wise groups. We considered statistically significant results with p values of 0.05 or less.
RESULTS
Contact information for 137 of the 138 directors of programs scheduled to graduate residents in 2011 was available on the ACGME website. Thirty-eight PDs (28%) responded to the participation request and all but one of them agreed to forward the e-mail to residents. A total of 296 graduating residents participated in the survey. According to the ACGME website, 1,498 trainees were expected to complete EM training programs in 2011, yielding a response rate of approximately 20%.15 All 296 participants completed the questions regarding their training, instruction, and previous experience with cricothyrotomy, but 3 failed to rate their comfort with the procedure and 7 did not complete the last question regarding the number of crics they had witnessed. This yielded a survey completion rate of 97.6%.
Video-assisted devices and gum elastic bougies were the most commonly used rescue devices, and a breakdown of residents’ frequency of adjunct device use is available in Table 1. The average degree of comfort, with “10” representing complete comfort, in performing a cricothyrotomy unassisted by another physician was 4.8 (95% CI 4.5–5.1) and the statistical mode was 3. A histogram of responses can be found in Figure 1.
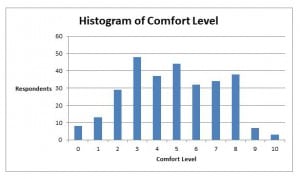
Histogram of EM residents’ reported comfort with performing a cricothyrotomy unassisted by another practitioner upon graduation; “10” represents complete confidence.
Models and simulators were the most commonly used methods of instruction with 83.1% of residents having practiced at least one cric on a model. A majority of trainees, 61.8%, had also practiced the procedure on recently deceased humans, and 46.6% had done so more than once. Animal models were used by 55.7% of respondents, and 3% reported having used “other” methods of instruction, but the nature of these alternative methods remains unknown. Table 2 illustrates the relative frequencies of cricothyrotomies on living patients, the deceased, animals, and models/simulators.
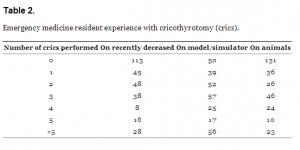
Emergency medicine resident experience with cricothyrotomy (crics).
Roughly half the participants, 51.6%, had witnessed at least one cric and 29.8% had seen more than one. Watching others perform the procedure was not shown to affect confidence, though there was a trend toward increased comfort among those who witnessed more than one procedure versus those who did not witness any, p=0.09. (Table 3) The clinician performing the procedure was most likely to be a trauma or general surgery resident, and a chart depicting the number of crics trainees witnessed other clinicians perform can be found in Figure 2. Rehearsing the procedure any number of times on animals was not found to affect reported confidence.
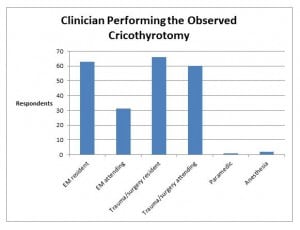
Background of clinicians who performed cricothyrotomies that residents observed but did not perform themselves.
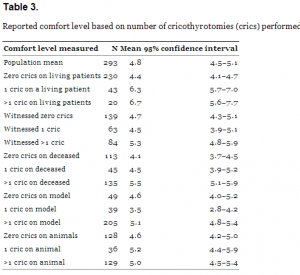
Reported comfort level based on number of cricothyrotomies (crics) performed.
Sixty-five respondents (22%) reported having performed at least one cricothyrotomy on a living person, and 64 of the 65 completed additional questions about the most recent procedure undertaken. EM attendings provided supervision the majority of the time, and in 7.8% of cases the procedure was unsupervised. (Table 1) Those who undertook a single cricothyrotomy on a living person reported a higher level of comfort with performing the procedure unassisted postgraduation than those who had done zero, and the difference was significant, p<<0.001. No difference in comfort was found between those having performed one cric and those who performed more than one. (Table 3)
A surgical technique was used in the overwhelming majority of cases. Angioedema/distorted anatomy and severe head or neck trauma were the most common reasons for failed airways. Inability to open the jaw, inability to ventilate, tissue edema, and Ludwig’s Angina were included as open responses by the remaining 14.1%. (Table 1)
Twenty-seven percent of patients on whom trainees had performed their most recent cricothyrotomies suffered complications. Six attempts were complicated by massive bleeding, 3 by vomiting/aspiration, and 2 by bradycardia. Six attempts involved either incorrect placement of the airway, incorrect location of the incision, or failure to pass the airway. Esophageal injury and “other trauma” were each listed as complications on one patient. Some respondents indicated more than one complication occurred in the same attempt. Sixty-one percent of patients survived the procedure long enough to get to the ICU or operating suite, and survival among trauma patients was 54% versus 65% among those who underwent surgical airway for non-traumatic indications.
As shown in Table 1, most trainees performed their most recent cricothyrotomy as a PGY 3 or PGY 4. Four respondents had experience with cricothyrotomy prior to residency–2 as a paramedic, one in combat while serving after internship, and one during a previous general surgery residency. It was unclear if the former surgical resident performed any additional crics during EM training, but the other 3 respondents did not. Regardless, all responses were included and analyzed in an intent-to-treat fashion.
Those having practiced more than one cric on the newly dead reported a higher degree of confidence with the procedure than those who did none, p<< 0.001. Performing the procedure only once did not result in a significant increase in confidence. While there was no significant difference in comfort levels regardless of the number of crics trainees performed on models or simulators, there was a trend toward decreased confidence among those who rehearsed the procedure only once versus those had not done so at all, p=0.06. (Table 3) When comparing these 2 groups, it was found that both performed the same number of total crics (by any means), and the same proportion of each group had experience with living patients (16%) and with animal labs. The subset that had never used a simulator, however, had performed more crics on the recently deceased. Graduates who reported practicing on models as well as the recently deceased also reported more confidence with the procedure, 5.4 (95% CI 5.0–5.8), than whose who used only models/simulators, 4.0 (95% 3.6–4.5), p<<0.001.
The vast majority of cricothyrotomies were performed by third- and fourth-year residents. A t-test (2-tailed distribution, equal variances assumed) also showed a trend toward a higher level of confidence among PGY 4/5s, 5.1 (95% CI 4.7–5.7) versus PGY 3s, 4.7 (95% CI 4.3–5.0), p=0.08, regardless of the number of cricothyrotomies performed. Pearson chi-squared analyses showed no effect of post-graduate year or previous cricothyrotomy experience with either living or deceased patients on patient survival.
DISCUSSION
Over the last several decades, improvements in rapid sequence intubation, changes in airway management in patients with suspected c-spine fractures, and the introduction of adjunct devices have reduced the frequency with which cricothyrotomy is performed.1,5,17 The use of adjuncts was highly prevalent in the population surveyed, but there will always be patients who, for one reason or another, cannot be intubated and will require a surgical airway. For this reason, the RRC for EM requires each resident to complete at least 3 cricothyrotomies prior to graduation to demonstrate proficiency.
Yet, this is the first published study attempting to clarify how many cricothyrotomies residents are performing on living patients requiring emergent airways, dog or other animal labs, models/simulators, and the recently deceased. The use of each of these methods of instruction is well documented in the literature, but their use relative to each other and residents’ ultimate degree of comfort with respect to cricothyrotomy were previously unknown.7,12,18
Previously reported rates of cricothyrotomy due to failed airway are quite low.1,4,19 Thus, it was somewhat surprising to find that 22% of graduating residents indicated they had performed a cricothyrotomy, though a portion of these had done so exclusively outside their EM training programs. Since cricothyrotomy is rare and because the nature of the study was clearly stated in the survey’s title and description, residents who have performed the procedure may have been those more likely to respond, overestimating the prevalence of cricothyrotomy among upcoming graduates. If this is true, then creating sufficient learning opportunities for trainees to gain proficiency becomes all the more important.
Not surprisingly, residents who had performed a cric on a living person rated their comfort with performing the procedure unassisted significantly higher than those who did not. Of the 223 crics observed, 129 were performed by non-ED staff. The fact that watching others perform the procedure failed to significantly raise residents’ reported comfort underscores the importance of ensuring EM trainees have a role in difficult airway management in the ED.3,17 Particularly in non-teaching institutions, it is usually impractical to await the arrival of a consultant before securing a surgical airway when one is needed.
Models and simulators, while being the most frequently reported method of instruction, did not clearly increase residents’ reported comfort. There was a trend toward decreased comfort among those who attempted only one procedure on a model versus those who attempted none. These 2 cohorts had performed the same total number of crics, and no difference between them could be found other than the group who had never used a simulator had performed a greater number of crics on the newly dead. Thus, the statistical trend observed is more likely to be a function of the more confident cohort having had more use of the recently deceased than less experience with simulators, since overall instruction on the recently deceased was found to increase residents’ comfort and instruction on models was not.
More than half of residents reported using animals in their training programs, but their use was not found to affect reported confidence. This survey did not ascertain what other procedures were performed on the animal, and a more dedicated study of the pooled benefit from all procedures done would need to be done to better assess the worthiness of sacrificing the animal for the sake of resident education.
The use of the recently deceased to teach residents how to perform rare procedures has long been an area of controversy.8,10,11,20,21 A 1994 survey of adult and pediatric critical care and EM PDs found that EM teaching programs were the most likely to use the recently deceased. Sixty-three percent of those programs reported use of the deceased, and in this study, 62% of residents reported practicing the procedure on the newly dead.11 Proponents of this practice cite the inability of models to simulate tissue layering and texture, the profuse bleeding often encountered, or the structural differences present that may impede passage of an airway.6,8,22 Indeed, a study of EMS personnel trained exclusively on mannequins showed less success in emergency intubation than those trained on people and animals.22 A separate but inherently related ethical issue is whether or not consent should be obtained prior to any such interventions, and several papers have demonstrated the feasibility of obtaining permission from next of kin.9,21–24 Residents in this study who practiced cricothyrotomy on the recently deceased reported higher degrees of comfort than those who did not. In addition, those using models as well as the newly dead reported greater comfort than those who used models alone. It is certainly possible that as higher fidelity simulators and virtual reality become available, training on non-humans may become more effective. Until that time, however, there is evidence that use of the newly dead offers residents the next best option in obtaining proficiency with cricothyrotomy.
Studies of largely elective cricothyrotomies found complication rates of 6–11%, and a 2010 meta-analysis of prehospital surgical crics found an overall success rate of 90.5%.25,26 In 1987, Erlandson reported a survival rate of 54% and complication rate of 23%, but more than half the patients in their data set were in cardiac arrest prior to cric.25 The mortality rate among trauma patients in this study is similar to that found in the literature, but residents reported a greater than expected number of complications during performance of their most recent cricothyrotomy.27 This may indicate that a sicker population was sampled, that too much time was spent using adjunct devices before resorting to a cric, that physicians’ clinical skills have deteriorated as experience with cricothyrotomy has declined, that the procedure is being done as a peri-mortem event for teaching purposes, or that other non-quantifiable factors are present.8,12 Further study regarding the nature and causes of complications is needed.
LIMITATIONS
The nature of this study contained several important limitations. First and foremost, permission to contact residents directly via e-mail distribution lists could not be obtained from any organization. Of the 137 PDs contacted, 37 responded indicating that the survey had been forwarded to residents. It remains unknown how many other PDs forwarded the e-mail without notifying the primary investigator of the decision to do so. Second, because not all graduates could be reached, it is possible that surveying a larger proportion of them may have altered the results, particularly regarding those data that showed trends toward significance but did not achieve it. However, previous research regarding appropriate sampling of populations indicates that the number of surveys returned was well above the minimum needed given a total population of 1,500.16
Third, surveying residents regarding a rare procedure will likely capture more who have done the procedure than who have not, thereby over-estimating the incidence of cricothyrotomy on living patients. Fourth, despite the anonymity of the electronic tool used to gather the data, some respondents may have been disinclined to admit using the recently deceased or animals to rehearse the procedure if they believe the act to be morally dubious. Fifth, data on long-term survival or neurologic outcome of patients was not gathered and thus the ultimate “success” of the crics done on living patients cannot be determined.
Lastly, the majority of residents had trained using models, animals, as well as the deceased, and it is not possible to evaluate adequately and independently each teaching method with regard to resident confidence or ability to perform the procedure quickly, successfully, and unsupervised as is required upon graduation. Further study with a larger population focusing on single methods of instruction may better clarify this question.
CONCLUSIONS
The vast majority of the graduating EM residents surveyed have never performed a cricothyrotomy on a living patient during training and do not rate their comfort with performing the procedure unassisted very highly. Undertaking cricothyrotomies on living as well as on recently deceased patients significantly increased reported levels of confidence, whereas instruction involving either models or animals, or watching others perform the procedure failed to do so. Given the rarity of cricothyrotomy in contemporary practice, a multi-faceted approach that increases resident involvement in surgical airways and expands training beyond use of models and simulators alone seems prudent.
Acknowledgments
The author would like to thank Dr. James M. Sinacore, Ph.D., Department of Preventive Medicine and Epidemiology, Loyola University Chicago, for help with statistical analysis.
Footnotes
Address for Correspondence: Andrew Makowski, MD. St. Joseph’s Hospital, Department of Emergency Medicine, 5000 W. Chambers St., Milwaukee, WI 53210. Email: Andrew_makowski@yahoo.com. 11 / 2013; 14:654 – 661
Submission history: Revision received May 14, 2013; Accepted July 1, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.


