| Author | Affiliation |
|---|---|
| Alfred Sacchetti, MD | Our Lady of Lourdes Medicine Center, Camden, New Jersey |
| Jennifer Williams, BSN | Our Lady of Lourdes Medicine Center, Camden, New Jersey |
| Steven Levi, MD | Our Lady of Lourdes Medicine Center, Camden, New Jersey |
| Devender Akula, MD | Our Lady of Lourdes Medicine Center, Camden, New Jersey |
ABSTRACT
Introduction:
Emergency department (ED) cardioversion (EDCV) and discharge of patients with recent onset atrial fibrillation or atrial flutter (AF) has been shown to be a safe and effective management strategy. This study examines the impact of such aggressive ED management on hospital charges.
Methods:
A random sample of 300 AF patients were identified from an ED electronic data base and screened for timing of onset of their symptoms. Patients were considered eligible for EDCV if either nursing or physician notes documented an onset of symptoms less than 48 hours prior to ED presentation and the patient was less than 85 years of age. An explicit chart review was then performed to determine patient management and disposition. Cardioversion attempts were defined as ED administration of procainamide, flecainide, propafenone, ibutilide, amiodarone or direct current cardioversion (DCCV). Total hospital charges for each patient were obtained from the hospital billing office. Differences across medians were analyzed utilizing through Wilcoxon rank sum tests and chi square.
Results:
A total of 51 patients were included in the study. EDCV was attempted on 24 (47%) patients, 22 (92%) were successfully cardioverted to normal sinus rhythm (NSR). An additional 12 (23%) spontaneously converted to NSR. Twenty (91%) of those successfully cardioverted were discharged from the ED along with 4 (33%) of those spontaneously converting. Pharmacologic cardioverson was attempted in six patients and was successful in three (50%), one after failed DCCV attempt. Direct current cardioversion was attempted in 21 (88%) and was successful in 19 (90%), two after failed pharmacologic attempts. Median charges for patients cardioverted and discharged from the ED were $5,460 (IQR $4,677–$6,190). Median charges for admitted patients with no attempt at cardioversion were $23,202 (IQR $19,663–$46,877). Median charges for patients whose final ED rhythm was NSR were $5,641 (IQR $4,638–$12,339) while for those remaining inAF median charges were $30,299 (IQR $20,655 – $69,759).
Conclusion:
ED cardioversion of recent onset AF patients results in significant hospital savings.
INTRODUCTION
Atrial fibrillation and atrial flutter (AF) are common emergency department (ED) cardiac arrhythmias.1,2 The initial management of newly recognized AF of greater than 48 hours is generally considered to be rate control with anticoagulation to prevent embolic sequelae. AF of less than 48 hours may be managed similarly, but also may be managed with cardioversion back into normal sinus rhythm. Such rhythm control of recent onset AF in the ED has been demonstrated to be both safe and effective, although controversy still exists as to whether cardioversion is the most appropriate management strategy in this patient population.2–4
This study examines the impact on hospital resources of these two different approaches to recent onset atrial fibrillation.
METHODS
A random number generator was used to select a sample of 300 patients with a primary diagnosis of either atrial fibrillation or atrial flutter from the ED electronic records of an urban community teaching hospital. The study hospital maintains a general ED which treats approximately 57,000 adults and children annually. The hospital has an active cardiac program, which includes an open heart surgery service, interventional cardiac catheterization facilities and 3 cardiac electrophysiology (EP) laboratories. The medical staff includes 7 practicing cardiac electrophysiologists distributed among 4 different private practices.
The ED records of the identified AF patients were examined for individuals considered eligible for ED Cardioversion (EDCV). Eligible patients were defined as those less than 85 years of age whose initial ED electrocardiogram demonstrated either atrial fibrillation or atrial flutter and whose record contained a nursing or emergency physician note stating specifically that the onset of the patient’s arrhythmia symptoms were less than 48 hours prior to ED presentation.
An explicit chart review was performed of these patient’s records to classify the patients by 3 dichotomous categories, EDCV attempted: yes or no, ED disposition: discharge to home or admission to hospital and Final ED cardiac rhythm: Normal Sinus Rhythm (NSR) or AF. A cardioversion attempt was defined by an ED record containing administration of procainamide, flecainide, propafenone, ibutilide, amiodarone or electrical synchronized cardoversion. Additional clinical information was collected to define the patient’s clinical characteristics at the time of presentation. Abstracted data included, patient age, systolic blood pressure, past medical history of hypertension, past history of atrial arrhythmia, history of shortness of breath, chest pain, or neurologic symptoms associated with the onset of the arrhythmia and initial myoglobin and troponin I levels.
All patient management in this study was at the discretion of the attending emergency physician caring for that particular patient, although any EP was free to obtain cardiology input on their patients. There is no ED policy addressing the management of recent onset atrial fibrillation.
The total hospital charges associated with each ED presentation were obtained from the hospital’s central billing office.
EDCV ‘s were performed under the direction of the single attending emergency physician. Procedural sedation was directed by the same attending emergency physician with either bolus propofol administration or remifentanil infusion.
Differences across medians were analyzed utilizing through Wilcoxon rank sum tests, additional analysis was through chi square.
This study was approved by the hospital’s Institutional Review Board.
RESULTS
A total of 51 patients were included in this study over a 30 month period. Patients in the different treatment groups were clinically similar with no statistically significant differences in age, systolic blood pressure, history of hypertension, history of atrial arrhythmia, history of shortness of breath, chest pain, or neurologic symptoms on presentation or initial myoglobin and troponin I levels. There was no evidence that the patients in any treatment group were less stable that those in any other group.
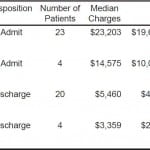
ED cardioversion was attempted in 24 (47%) patients and was successful in 22 (92%), with 20 (91%) discharged from the ED. Cardioversion was attempted through Direct Current Cardioversions (DCCV) in 21 (88%) patients and was successful in 19 (90%). Pharmacologic cardioversion was attempted in 6 (24%) patients and was successful in 3 (50%). Three (12%) patients underwent both pharmacologic and DC cardioversion, 1 after a failed DCCV and 2 after a failed pharmacologic attempt. Another 13 (25%) spontaneously converted to sinus rhythm with 4 (30%) discharged. Median charges for patients cardioverted and discharged from the ED were $5,460 (IQR $4,677–$,190). Median charges for admitted patients with no attempt at cardioversion were $23,202 (IQR $19,663–$46,877). The table summarizes the relation between charges and ED management. Median charges for patients who’s final ED rhythm was NSR were $5,641 (IQR $4,638–$12,339) while for those remaining in AF median charges were $30,299 (IQR $20,655 – $69,759) regardless of patient disposition.
DISCUSSION
The optimal ED management of recent onset atrial fibrillation remains unclear.2,4 Advocates for rate control believe that once an emergency physician controls the patient’s rate, the decisions concerning the timing of the rhythm control are best left to the admission cardiologists caring for the patient.4 Proponents of rhythm control in the ED state that the longer a heart remains in atrial fibrillation the more the atrium become conditioned to accept this rhythm. The concept that a-fib begets a-fib would support a more aggressive approach to conversion of these patients as rapidly as possible.5 Immediate cardioversion also eliminates the need for anticoagulation and reduces the risk of stroke for those remaining in atrial fibrillation.6,7 It is also believed that the sooner after the onset of atrial fibrillation the cardioversion is attempted the more likely the procedure is to be successful and the greater the chance that the patient will maintain normal sinus rhythm following discharge.8,9
The safety of this approach to the management of recent onset AF has already been established in a number of prior reports on this topic and EDCV is considered standard management in many EDs.1,2,5,10 This current study was not designed to re-examine this question.
This is the first study to examine the economic implications of the aggressive ED management of recent onset atrial fibrillation/flutter. The incidence of atrial fibrillation related ED visits have increased by 88% from 1993 though 2003 with 65% resulting in ED admissions at a cost of over $6.65 billion dollars. 1 ED Cardioversion and Discharge could produce substantial savings if more universally applied to this population.
An unexpected finding in this study was the resource savings produced by simply attempting EDCV regardless of the results. Admitted patients remaining in atrial fibrillation or flutter following cardioversion attempts still exhibited hospital charges $8,628 lower than those admitted with no EDCV attempt.
LIMITATIONS
Because this was a retrospective study, patient treatments were not randomized. Even though we attempted to control for this in the structured data abstraction process, it is still possible that different treatment paths were selected based on the patient’s presentation.
CONCLUSION
The use of ED Cardioversion in patients with recent onset of AF is associated with decreased hospital charges. These findings would support the cost effectiveness of aggressive ED management of patients with this condition.
Table. Hospital Charges for Study Groups
EDCV, Emergency Department Cardioversion; IQR, Inter-Quantile Range
Footnotes
Supervising Section Editor: Amal Mattu, MD
Submission history: Submitted September 13, 2011; Revision received December 22, 2011; Accepted January 16, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.1.6893
Address for Correspondence: Alfred Sacchetti, MD, Department of Emergency Medicine, Our Lady of Lourdes Medicine Center, Camden, NJ 08103
Email: sacchettia@lourdesnet.org
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Barrett TW, Martin AR, Storrow AB, et al. A clinical prediction model to estimate risk for 30-day adverse events in emergency department patients with symptomatic atrial fibrillation. Ann Emerg Med. 2011;57:1–12. [PMC free article] [PubMed]
2. Stiell IG, Clement CM, Brison RJ, et al. Variation in management of recent-onset atrial fibrillation and flutter among academic hospital emergency departments. Ann Emerg Med. 2011;57:13–21.[PubMed]
3. Dankner R, Shahar A, Novikov I, Agmon U, Ziv A, Hod H. Treatment of stable atrial fibrillation in the emergency department: a population-based comparison of electrical direct-current versus pharmacological cardioversion or conservative management. Cardiology. 2009;112:270–8.[PubMed]
4. Roy D, Talajic M, Nattel S, et al. Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med. 2008;358:2667–2677. [PubMed]
5. Stiell IG, Clement CM, Perry JJ, et al. An aggressive protocol for rapid management and discharge of emergency department patients with recent-onset episodes of atrial fibrillation and flutter. CJEM.2010;12:181–191. [PubMed]
6. Stead LG, Vaidyanathan L. Evidence-based Emergency Medicine/Systematic Review Abstract. Rhythm control with electrocardioversion for atrial fibrillation and flutter. Ann Emerg Med.2009;54:745–7. [PubMed]
7. Stewart S, Hart CL, Hole DJ, et al. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley Study. Am J Med. 2002;113:359–364.[PubMed]
8. Zahir S, Lheureux P. Management of new-onset atrial fibrillation in the emergency department: is there any predictive factor for early successful cardioversion? Eur J Emerg Med. 2005;12:52–6.[PubMed]
9. Fundaró C, Galli A, Paglia S, et al. Atrial fibrillation in emergency department: prevalence of sinus rhythm 1 week after discharge. Emerg Med J. 2011 Mar 25; [Epub ahead of print]
10. von Besser K, Mills AM. Is discharge to home after emergency department cardioversion safe for the treatment of recent-onset atrial fibrillation? Ann Emerg Med. 2011 Dec;58:517–20. [PubMed]