| Author | Affiliation |
|---|---|
| Alicia S. Devine, MD | Department of Emergency Medicine, Eastern Virginia Medical School, Norfolk, VA |
| Corinne S. Jackson, MD | Department of Emergency Medicine, Eastern Virginia Medical School, Norfolk, VA |
| Lisa Lyons, MD | Department of Emergency Medicine, Eastern Virginia Medical School, Norfolk, VA |
| Jon D. Mason, MD | Department of Emergency Medicine, Eastern Virginia Medical School, Norfolk, VA |
ABSTRACT
Introduction:
To determine the incidence and frequency of follow-up instructions for incidental findings on computed tomography (CT) scanning of the abdomen and pelvis in trauma patients.
Methods:
We performed a retrospective chart review of all adult patients triaged to the trauma service at a Level I trauma center between July 1, 2003 and June 30, 2004. Included patients were 16 years of age and older who underwent abdomen and pelvic CT scans as part of their primary evaluation. We excluded patients under the age of 16 years, patients unable to complete radiographic studies due to deterioration in condition, patients with missing CT scan reports, and transferred patients who had CT scans done at outside facilities.
Results:
A total of 1,633 patients presented to the trauma service during the study period; 922 patients met inclusion criteria. Of these, 392 had incidental findings noted on the formal radiology report. Twenty patients with incidental findings either received additional workup during their hospital admission for their trauma injuries or were notified of the findings on discharge. Nine died prior to discharge. One hundred twenty-two patients with incidental findings had those findings noted in the history and physical or discharge summary with no documentation of follow-up. There was no documentation of any incidental findings in the electronic record for the majority of patients (242) with incidental findings.
Conclusion:
The majority of incidental findings discovered on abdomen and pelvic CT scanning of trauma patients are not documented; therefore, many patients may not receive the appropriate recommended follow up.
INTRODUCTION
Computed tomography (CT) scanning has replaced diagnostic peritoneal lavage and serial abdominal exams in the evaluation of patients who have sustained abdominal trauma. CT allows for the rapid identification of intra-abdominal injuries in patients with acute trauma with a high level of specificity and sensitivity and can assist the trauma surgeon in determining operative versus non-operative management.
In addition to providing information regarding the presence or absence of acute intra-abdominal trauma, CT scans also reveal pathology unrelated to the trauma that may or may not be clinically significant. These incidental findings may require additional evaluation on an emergent or urgent basis and should be communicated to the patient. Failure to notify patients of incidental findings could adversely impact their health and potentially give rise to legal action by patients for harm caused by this omission.
We reviewed the abdominal and pelvic CT scans of trauma patients presenting to a Level I trauma center over a one-year period to determine the incidence of incidental findings and the nature of the follow-up for these findings.
METHODS
This was a retrospective chart review of 1,633 patients triaged to the trauma service at a Level I trauma center at an urban teaching hospital between July 1, 2003 and June 30, 2004. Patients were identified through the trauma registry maintained at the hospital. The purpose was to identify findings noted on abdominal and pelvic CT scans that were unrelated to trauma and to classify those findings that required additional interventions or diagnostic studies. Included patients were those over 16 years of age who underwent CT scans of the abdomen and pelvis as part of the initial evaluation after arrival to the trauma bay. All mechanisms (i.e. blunt vs. penetrating trauma) were included. Exclusion criteria included: patients less than 16 years old; patients whose condition deteriorated, thus preventing completion of radiographic studies; patients transferred to the trauma center with CT scans performed at another facility; and patients managed primarily by the emergency physicians but who received a trauma team consult. All CT scans were reviewed by board-certified radiologists.
The electronic medical records (EMR) were reviewed for each patient who met inclusion criteria by three reviewers who were not blinded to the objectives of the study. Only those findings included in the final impression portion of the radiologist’s formal report that were not related to trauma were included; findings noted in the narrative portion of the dictation but not included in the final impression were excluded. Specific recommendations made by the radiologist interpreting the study were noted and included as well. In some instances, findings were made regarding the lower lung fields seen on the CT scan of the abdomen and pelvis and these were included. Excluded findings included: atelectasis; physiologic pelvic fluid; evidence of old trauma; surgical changes; and findings that could be related to trauma. Incidental findings that were to be excluded were determined prior to the start of the study.
For all patients with incidental findings not related to trauma, we reviewed the EMR to determine if any subsequent studies or further workup was performed during the hospital admission for the traumatic injuries. This included specialty consultation, further radiographic studies and clinical correlation. In addition, the discharge summaries for each patient were reviewed to determine if the patient was notified of the findings and/or given any discharge instructions that included outpatient follow-up recommendations. In those instances where the patient was discharged directly from the emergency department (ED), the dictated history and physical was reviewed as well as it often included the patient’s disposition as well as discharge instructions. This study was approved by our Institutional Review Board.
RESULTS
From July 1, 2003 to June 30, 2004, 1,633 trauma patients presented to our trauma center. Of these patients 1,045 had a CT scan of the abdomen and pelvis performed on initial presentation and had a report available in the EMR. One hundred twenty-three patients were less than 16 years old, leaving 922 patients who met inclusion criteria.
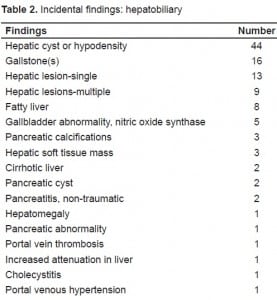
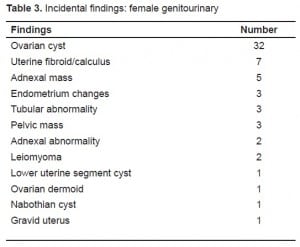
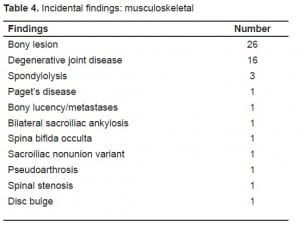
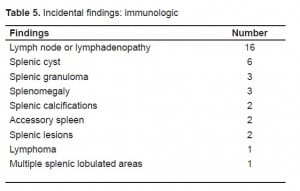
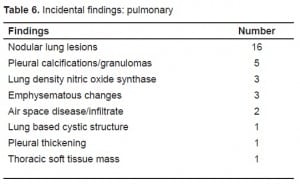
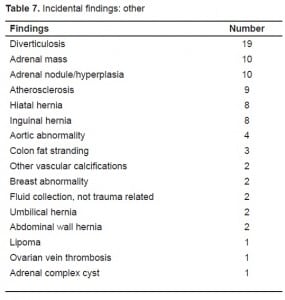
A total of 530 patients either had normal CT scans or CT scans consistent with acute trauma without incidental findings, while 392 had incidental findings on CT scan with or without evidence of trauma (Tables 1–7). In 62% (242/392) of patients with incidental findings noted on CT scan, no further documentation was found in the EMR regarding the incidental findings. Five percent of patients (20/392) either received specialty consult or additional studies related to their incidental findings while in the hospital, or were notified of their results according to the dictated discharge summaries. Nine patients received specialty consult while in the hospital (four urology consults, two OBGYN consults, two internal medicine consults and one vascular surgery consult); one patient had a testicular ultrasound performed; and the rest were given discharge instructions regarding follow up of their incidental findings. Thirty-one percent of patients (121/392) with incidental findings had these noted either in the dictated history and physical or discharge summary without mention of notifying the patient or recommending additional outpatient work-up. Nine patients died prior to discharge from the hospital.

DISCUSSION
Patients being evaluated for multisystem trauma frequently undergo CT scans to evaluate for injury. It is not uncommon for a single trauma patient to have a CT scan of the head, cervical spine, chest, abdomen and pelvis as part of the workup. CT scans are an excellent modality for detecting traumatic injuries, as well as for detecting other pathologic conditions present that are unrelated to the trauma. The issue then becomes how best to handle the additional information obtained.
In many cases, the incidental findings simply need to be verbalized to the patient for outpatient follow up with his primary care physician. In other cases, more emergent or urgent follow up is warranted with further imaging or specialist consultation.
Our findings are consistent with similar studies regarding incidental findings on CT scans. In one retrospective study performed in the ED, only 21% of incidental findings noted on abdominal CT scans to evaluate for renal stones were noted in the record and only 18% had any evidence of followup.1 In a Level I trauma center in San Diego, 34% of patients were found to have incidental findings on CT scan, and only 50% of patients with findings requiring attention prior to discharge had adequate documentation of the management of their incidental finding.2
A similar study to ours found that 43% of trauma patients had incidental findings on CT scans of the abdomen and pelvis and only 27% of those had documentation of the findings.3 Interestingly, the frequency of incidental findings on CT scans of brains of trauma patients is much lower, as evidenced by a retrospective review of 3,000 patients that found only 30 incidental abnormalities.4 In one study of patients undergoing CT scans for pulmonary embolism in the ED, 59% of patients who did not have a pulmonary embolism had incidental findings that ranged in severity from indeterminate to requiring immediate intervention.5
As technology advances, the capability of CT to identify incidental findings will continue to increase. Emergency medicine and trauma are not the only specialties to face this issue; cardiology and endocrinology have struggled with the appropriate way to address incidental findings.6,7,8
LIMITATIONS
There were 588 patients who either did not have a CT scan of the abdomen and pelvis performed or who had no EMR of the results of the CT scans available in the hospital databases. For the majority of incidental findings, there was no documentation of the findings in the dictated patient chart. It is possible that in some cases patients were verbally notified of these incidental findings and this was simply not documented in the record. We used only the EMRs and not the actual physical chart for our study. We limited our study to the frequency of incidental findings and did not make any classifications of the findings in terms of their clinical significance.
CONCLUSION
Incidental findings are a common occurrence with abdominal and pelvic CT scans performed for trauma patients. In our study most of these findings were not documented, and it is presumed that many of the patients were not informed of their findings. Communication of this information has a number of legal and ethical considerations. In many cases, the findings are clinically insignificant and likely will not have any impact on the patient. In other cases, it is clear that close follow up is warranted to ensure exclusion of serious, life-threatening processes such as malignancy. At other times, follow up could lead to unnecessary, costly and invasive testing.
While the immediate priority is to address the acute traumatic injuries, implementing additional safeguards into the system to ensure that patients are notified of incidental findings is important. Further research is necessary to determine the impact of these incidental findings. This includes outcomes of the patients who were notified and those who were not notified of their CT scan findings. In some cases the findings may be lifesaving, while in others it may lead to unnecessary and invasive procedures or increased radiation exposure.
Footnotes
Supervising Section Editor: Jeffrey Druck MD
Submission history: Submitted May 24, 2009; Revision Received August 4, 2009; Accepted September 14, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Corresponcence: Alicia S. Devine, MD, JD, Department of Emergency Medicine, Eastern Virginia Medical School, Raleigh Building Room 304, 600 Gresham Drive, Norfolk, VA 23507
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Messersmith WA, Brown DF, Barry MJ. The prevalence and implications of incidental findings on ED abdominal CT scans. Am J Emerg Med. 2001;19(6):479–81. [PubMed]
2. Paluska TR, Sise MJ, Sack DI, et al. Incidental CT findings in trauma patients: incidence and implication for care of the injured. J Trauma. 2007;62(1):157–61. [PubMed]
3. Munk MD, Peitzman AB, Hostler DP, et al. Frequency and follow-up of incidental findings on trauma computed tomography scans: experience at a level one trauma center. J Emerg Med. 2008. Epub ahead of print.
4. Eskandary H, Sabba M, Khajehpour F, et al. Incidental findings in brain computed tomography scans of 3000 head trauma patients. Surg Neur. 2005;63(6):550–53.
5. Richman P, Courtney M, Friese J, et al. Prevalence and significance of nonthromboembolic findings on chest computed tomography angiography performed to rule out pulmonary embolism: a multicenter study of 1,025 Emergency Department Patients. Acad Emerg Med. 2004;11(6):642–47.[PubMed]
6. Bovio S, Cataldi A, Reimondo G, et al. Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J Endocrinol Invest. 2006;29:298–302. [PubMed]
7. Budoff M, Fischer H, Gopal A. Incidental findings with cardiac CT evaluation-should we read beyond the heart. Catheterization and cardiovascular interventions. 2006;68:965–73. [PubMed]
8. Budoff MJ, Fischer H, Gopal A. Incidental findings with cardiac CT evaluation-should we read beyond the heart. Cath and Cardiovasc Interv. 2006;68:965–73.


