| Author | Affiliation |
|---|---|
| Mathew Foley, MD, MS | Kings County Hospital Center, Brooklyn, NY State University New York Downstate Medical Center, Brooklyn, NY |
| Nizar Kifaieh, MD | Kings County Hospital Center, Brooklyn, NY State University New York Downstate Medical Center, Brooklyn, NY |
| William K. Mallon, MD | Los Angeles County Hospital, Los Angeles, CA University of Southern California Medical Center, Los Angeles, CA |
ABSTRACT
Introduction:
The economic benefits of reducing emergency department (ED) crowding are potentially substantial as they may decrease hospital length of stay. Hospital administrators and public officials may therefore be motivated to implement crowding protocols. We sought to identify a potential cost of ED crowding by evaluating the contribution of excess ED length of stay (LOS) to overall hospital length of stay.
Methods:
We performed a retrospective review of administrative data of adult patients from two urban hospitals (one county and one university) in Brooklyn, New York from 2006–2007. Data was provided by each facility. Extrapolating from prior research (Krochmal and Riley, 2005), we determined the increase in total hospital LOS due to extended ED lengths of stay, and applied cost and charge analyses for the two separate facilities.
Results:
We determined that 6,205 (5.0%) admitted adult patients from the county facility and 3,017 (3.4%) patients from the university facility were held in the ED greater than one day over a one-year period. From prior research, it has been estimated that each of these patient’s total hospital length of stay was increased on average by 11.7% (0.61 days at the county facility, and 0.71 days at the university facility). The increased charges over one year at the county facility due to the extended ED LOS was therefore approximately $9.8 million, while the increased costs at the university facility were approximately $3.9 million.
Conclusion:
Based on extrapolations from Krochmal and Riley applied to two New York urban hospitals, the county hospital could potentially save $9.8 million in charges and the university hospital $3.9 million in costs per year if they eliminate ED boarding of adult admitted patients by improving movement to the inpatient setting.
INTRODUCTION
Emergency department (ED) crowding continues to be a major problem for our healthcare system. In 2006 the Institute of Medicine (IOM) reported that one area warranting special attention at Academic Medical Centers (AMCs) was “the need to address AMC emergency department crowding and its adverse effect on quality of care and patient safety.”1
While the IOM focuses on improving patient care, other studies look at financial impact and specifically how decreasing crowding will produce an increase in hospital revenue and a decrease in expenditures.2–6 Krochmal and Riley3 outline how hospital lengths of stay (LOS) are extended for patients with an extended ED LOS and predicts the financial impact of these implications. These authors calculated that an increased ED LOS increases hospital costs by $6.8 million over three years.3 Therefore, decreasing ED crowding by decreasing the ED LOS per patient has a significant potential to decrease costs.
Using Krochmal and Riley’s3 findings, we sought to project charge and cost savings for two New York City hospitals if ED crowding were reduced by decreasing ED LOS for admitted patients.
METHODS
This is a retrospective review of administrative data from two separate urban hospitals in Brooklyn, New York. During the study period, neither hospital had an ED crowding protocol in place. The relationship between clinical throughput data and patient charge/cost data was drawn using previously published estimates regarding the impact of ED LOS on hospital LOS. We extrapolated data from Krochmal and Riley, 3 who evaluated the association of an ED LOS greater than one day with the total hospital LOS. We then calculated potential costs and charges accrued by increasing hospital LOS due to increased ED LOS .
The first hospital is a county institution with 627 inpatient beds and an annual ED census of 125,000 patients. The other hospital is university-based with 406 inpatient beds and an annual ED census of 88,000 patients. Neither hospital had a formal ED holding or observation unit. A holding unit is a predetermined, staffed location in the ED to hold admitted patients until an inpatient location is ready. An observation unit is a predetermined, staffed location in the ED where a person is observed for a predetermined amount of time before discharge from the hospital. Data collected from each institution included annual ED census, ED admissions per month, average number of ED admissions per day, average ED output times per month, average hospital LOS, and cost or charge per medical/surgical bed per day. We collected ED data for the county hospital from the Misys-Computerized Patient Record/Computerized Physician Order Entry (CPR/CPOE) system software (Misys Healthcare Systems, Raleigh, NC, USA) from July 2006 to March 2007. We obtained ED data for the university hospital from October 2006 to October from that institution’s Performance Improvement (PI) committee. The PI committee collected its data using NaviCare software (Hill-Rom Services, Inc. Batesville, IN, USA). The average hospital LOS and cost/charge data were collected by respective hospital officials.
In order to assess the financial impact of ED crowding on an institution and its costs/charges, we examined clinical throughput and fiscal variables at these two hospitals. We calculated the ED LOS for patients admitted to the hospital from when a patient entered the ED (signing in at triage) until the patient physically exited the ED. The ED LOS includes the output time for each admitted patient. The output time is a measure of the length of time an admitted patient (inpatient) is physically located in the ED while waiting for an inpatient bed. The hospital (inpatient) LOS is defined from when the admission order is placed by the ED physician until the time of discharge. Therefore, ED LOS is a subset of the hospital LOS, and includes the ED output time, as in Krochmal and Riley’s3 study. We used these variables to calculate an extended ED LOS of admitted patients.
Krochmal and Riley3 defined an extended ED LOS of an admitted patient as one that remained in the ED at midnight. This calculation was used because inpatient days at the institution that Krochmal and Riley3 studied are counted by the midnight census regardless of patient location (ED or inpatient bed). Total inpatient LOS included the time the patient spent boarding in the ED after being admitted.
We obtained fiscal variables from each hospital’s respective ED administrator. Unfortunately, each hospital quantifies the expense of an inpatient bed differently. The county hospital in our study reports the expense of an adult inpatient bed by charges per day, while university hospital reports this by the cost of this occupied bed for one day. We used only the cost/charges of adult medical/surgical floor beds and not intensive care unit (ICU) beds, despite the fact that some patients were admitted to the ICU. We did not use the cost/charges of pediatric inpatient beds as pediatric admissions were excluded.
We subsequently used previously published calculations to determine cost/charge endpoints.3 The number of patients who stayed in the ED greater than one day, as per the Krochmal and Riley3definition, was found to have an average increase in hospital LOS of 11.7%. We calculated the number of patients who stayed in the ED greater than one day at each hospital based on their output time. This was calculated by collecting the average output time and multiplying by the average number of admissions per hour during the same time frame to obtain the quantity of admitted patients located in the ED at midnight each day.
The number of admitted patients located in the ED at midnight represents the number of patients who had an extended ED LOS. We multiplied this figure by 365 to represent the total number of patients admitted to the hospital in one year who had an extended ED LOS and were therefore predicted to have an extended hospital LOS.
Krochmal and Riley3 concluded that there was a 11.7% increase in hospital LOS due to an ED LOS greater than one day.3 We obtained the average inpatient LOS at each hospital from each institution’s administrators and calculated the average increase in hospital stay for a patient who had an extended ED LOS based on Krochmal and Riley’s3 conclusions. Therefore, we calculated the extended hospital LOS due to an extended ED LOS by adding 11.7% of the average hospital LOS to the average hospital LOS.
The total number of patients admitted to the hospital in one year who were predicted to have an extended hospital LOS was multiplied by the average hospital stay at each site. We also multiplied the total number of patients admitted to the hospital in one year who were predicted to have an extended hospital LOS by the predicted extended hospital LOS based on the Krochmal and Riley3conclusions. The difference between these two figures resulted in the total increase of unnecessary hospital inpatient days due to an extended ED LOS.
Lastly, the total number of increased hospital inpatient days – due to an extended ED LOS over a one-year period – was multiplied by either the cost of a medical/surgical bed per day at the university-based institution or the charge for a medical/surgical bed per day at the county hospital.
RESULTS
The county hospital had an average adult patient output time of 11.4 hours for 2007 along with an average of 1.49 admissions per hour. An average of 17 adult admitted patients were present in the ED at midnight daily for a total of 6,205 adult admitted patients for the year 2007. The average hospital LOS was 5.2 days and is calculated to be 5.81 days for those with an extended ED LOS. Since the average charge for a medical/surgical floor bed per day is $2,590, it is calculated that the hospital was charging an extra $1,580 per patient who had an extended stay in the ED. Therefore, an average 11.7% increase in hospital LOS for the 6,205 adult patients with an increased ED LOS would amount to $9,803,280 in excess charges for 2007 (Table 1).
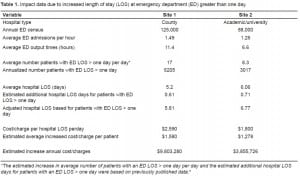
The university hospital had an average adult patient output time of 6.6 hours for the time period studied along with an average of 1.26 admissions per hour. It is calculated that an average of 8.3 adult admitted patients would be present in the ED at midnight daily or a total of 3,017 patients per year. The average hospital LOS was 6.06 days and is calculated to be 6.77 days due to an extended ED LOS. Since the average cost for a medical/surgical floor bed per day is $1,800, it is calculated that it cost the hospital an extra $1,278 per patient who had an extended ED LOS. Therefore, an average 11.7% increase hospital LOS for the 3,017 adult patients with an increased ED LOS would amount to $3,855,726 in excess costs for the university hospital in 2007 (Table 1).
DISCUSSION
This study suggests that hospitals could avoid significant patient charges/costs by reducing ED LOS. According to our model, the county hospital could have saved $9.8 million in charges and the university hospital could have saved $3.85 million in costs over one year if ED boarding were eliminated. Furthermore, payers are less likely to pay fees following extended inpatient stays, which means that much of these charges and costs may not be recouped.
While ED crowding and its morbidity and mortality is well documented, the cost of ED crowding has yet to be elucidated. The documentation of increased morbidity and mortality has not stimulated the implementation of ED crowding solutions, but the financial drain to hospitals due to ED crowding may provide this stimulus. Many factors that contribute to ED crowding, including ambulance diversion and patients leaving without being seen, are suspected to be fiscally detrimental to a hospital. While all of these factors need to be explored, this study is the second, after the Krochmal and Riley study,3 that examines the effect of ED crowding on the expense of increased hospital length of stay.
While the Krochmal and Riley3 study estimates direct costs to the hospital due to increased ED LOS, other studies have found potential loss of revenue due to ED crowding. Bayley et al.4 sought to determine the additional cost of an extended ED LOS for chest pain patients awaiting non-ICU monitored beds, a relevant point because more than six million patients present to the ED with chest pain each year.7 This study found that 91% of admitted patients waited more than three hours for an inpatient bed, which amounts to a potential revenue loss of $204 per patient.
Falvo et al.5 also found a significant loss of potential hospital revenue and ED functional treatment capacity due to increased length of ED stays of admitted patients. This study concluded that “transferring admitted patients from the ED to an inpatient unit within 120 minutes would have increased the functional treatment capacity of the ED by 10,397 hours” over one year. Furthermore, by reducing admission process delays during their 12-month study, “the hospital could potentially have accommodated another 3,175 patient encounters in its existing treatment spaces.” Lastly, the authors concluded that in 12 months $3,960,264 in net revenue for the hospital could have been generated by providing emergency services to new patients in ED beds used to board inpatients. The findings of both Falvo et al.5 and Bayley et al.4 are relevant to the two New York City hospitals presented in our study because the average output times for these NY hospitals (11.4 and 6.6 hours respectively) are longer than the benchmark output times used in the aforementioned studies (three hours and 120 minutes).
Significant revenue can also be lost due to ED ambulance diversion, a result of ED crowding and decreased patient flow. In a Canadian study by Schull et al.8 ED crowding was directly linked to ambulance diversion. Authors found that the length of ambulance diversion increased with the number of admitted patients boarded in the ED (6.2 minutes per patient) and also increased with ED patient boarding time (11.3 minutes per hour). It has also been demonstrated that ambulance diversion can affect hospital revenue. Falvo et al.6 found that during a 12-month period, a 450-bed nonprofit community teaching hospital with 62,588 patient visits to the ED “may have lost $3,881,506 dollars in net revenue as a result of ambulance diversions and patient elopements.” Authors concluded that “significant revenue may be foregone as a result of throughput delays that prevent the ED from utilizing its existing bed capacity for additional patient visits.”
A proposed solution to ED crowding is a Full Capacity Protocol (FCP). An FCP is a plan that uses additional hospital resources and atypical bed space to decompress overcrowded EDs. The State University of New York at Stony Brook has had an FCP in place since 2001.9 Its protocol calls for admitted patients who are boarding in the emergency room, when the ED is at full capacity, to be boarded in the acute care beds located in the hallways of the inpatient floor, – up to a maximum of two additional patients per inpatient unit. A boarding patient is defined as a patient who has been admitted to the hospital from the ED, who is no longer an active patient in the ED, and who is waiting to occupy a cleaned, unoccupied room. The theory behind this protocol is that ED crowding is a hospital problem and not just an ED problem, and that the entire hospital should participate in a solution.
Since 2001, only a few hospitals have adopted an FCP due to multiple administrative roadblocks– all despite an FCP’s potential to decrease costs, augment revenue, and increase patient satisfaction and safety. Among the most strident opponents have been nursing associations and hospital administrations.
The California Nurses Association openly opposed California State Assembly bills AB2207 in 2008 and AB911 in 2009, which require hospitals to regularly assess the condition of the ED based on a national score and develop an FCP. AB2207 would have allowed boarded ED patients to be moved to hallways of inpatient units in the most severe and dangerous instances of ED crowding. Nursing associations objected to these protocols – and continue to do so – claiming that if these protocols were to be implemented, inpatient nurses would have too many patients to care for and might be required to provide that care in hallways.
Hospital administrations, on the other hand, oppose FCPs for largely unknown reasons. The California Hospital Association also openly opposed AB2207 and currently opposes AB911. It is speculated that hospital administrators believe that boarding patients in ED hallways is a better financial option than reserving inpatient rooms for those patients admitted through the ED. However, since an economic analysis of FCPs has not been completed, the magnitude of the financial impact of an FCP is unknown. It is additionally speculated that boarding patients in the ED is logistically easier for the hospital administration than making other arrangements for these patients. Again, there is no research or evidence to support this theory.
In addition to opposition from nursing associations and hospital administrations, FCPs have been slow to gain widespread adoption because, aside from one abstract, there have been no published prospective studies that assess the benefits of implementing an FCP. Published out of a hospital in Vancouver, Canada, the abstract prospectively studied the effects of implementing an Overcapacity Care Protocol (as it is called in Canada).2 The abstract outlined two benefits to implementing the Overcapacity Care Protocol: a decrease in the average ED LOS for all admitted patients by five hours, and an increase in ambulance arrivals. In addition, during the period of the study the ED volume increased and the average LOS decreased by approximately 24 hours for all admitted patients. These are significant results and suggest that implementing a hospital-based ED crowding protocol can be beneficial by decreasing ED crowding, decreasing hospital costs, and decreasing ambulance diversion.
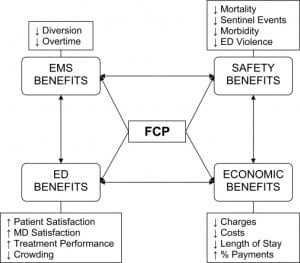
An FCP can provide various economic, patient safety, ED and emergency medical services (EMS) benefits. Patient safety benefits are well documented, include decreased mortality, decreased morbidity, decreased sentinel events, and decreased ED violence.10–11 The ED significantly benefits from FCPs by improving the working environment and increasing physician satisfaction, increasing patient satisfaction, and improving treatment performance.11–12 As described above, FCPs can affect EMS by decreasing ambulance diversions, and therefore decreasing EMS overtime (Figure 1). Since patient safety and patient satisfaction have not been enough to convince many hospital administrations to adopt hospital-based ED crowding protocols, perhaps potential cost savings and potential revenue earned will persuade the appropriate officials. While prospective studies of implementing hospital-based ED crowding protocols are crucial, there is currently a lack of any published prospective or retrospective studies.
LIMITATIONS
The calculations for the county hospital charges and university hospital costs cannot be compared. The county hospital provided average charges per medical/surgical bed, while the university hospital provided average costs per medical/surgical bed. It should be noted that charges are often misleading, and inflated compared to what the actual cost is to a hospital. Furthermore, these figures are conservative estimates because ICU bed costs and charges are not calculated. The average charge for an ICU bed at the county hospital is $4,060 per day and $2,760 per day at the university hospital. Lastly, the above calculations do not take into account that third-party payers are more likely to reimburse charges for patients with shorter stays in the hospital.
CONCLUSION
A strong argument can be made that the ED is the safety net for the American healthcare system.13Despite this argument, EDs around the country do not receive enough support from either the government or the hospitals in which they reside in order to function adequately. America’s “Emergency Department Crisis” is well documented, as there has been a decrease in the number of EDs and an increase in the number of visits to our national EDs over the past two decades.14Contrary to popular belief, ED crowding should not be attributed to the uninsured population.15Rather, it is a consequence of both increased visits and inefficient patient flow within the hospital. Decreasing ED crowding has the potential to save hospitals money and create more revenue streams for them. The estimates provided by studying the above two New York City hospitals consider just one factor of ED crowding: increased ED length of stay. This one factor has the potential to save each of these hospitals millions of dollars without considering the savings or revenue of other factors, such as decreasing ambulance diversion and improving ED bed use. Both the government and hospital administrations can and should aid in decreasing ED crowding. If viewed as a healthcare system and hospital problem – and not just an ED problem – decreasing ED crowding has the potential to significantly help our patients, increase hospital revenue, and decrease healthcare costs.
Footnotes
Supervising Section Editor: Stephen J. Wolf, MD
Submission history: Submitted: December 3, 2008; Revision received May 20, 2009; Accepted June 21, 2010.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem.
Address for Correspondence: Mathew Foley, MD, MS, Department of Emergency Medicine, Kings County Hospital Center, SUNY Downstate Medical Center
Email: airfoley@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Handel DA, Sklar DP, Hollander JE, et al. Institute of Medicine/Association of American Medical Colleges Panelist Group Society for Academic Emergency Medicine. Association of Academic Chairs in Emergency Medicine Panel. Executive summary: the Institute of Medicine report and the future of academic emergency medicine: the Society for Academic Emergency Medicine and Association of Academic Chairs in Emergency Medicine Panel: Association of American Medical Colleges annual meeting. Acad Emerg Med. 2007 Mar;14(3):261–7. [PubMed]
2. Innes G, Grafstein E, Stenstrom R, et al. Impact of an overcapacity care protocol on emergency department crowding. Acad Emerg Med. 2007;14(5):S85.
3. Krochmal P, Riley TA. Increased health care costs associated with ED overcrowding. Am J Emerg Med. 1994 May;12(3):265–6. [PubMed]
4. Bayley MD, Schwartz JS, Shofer FS, et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med. 2005 Feb;45(2):110–7. [PubMed]
5. Falvo T, Grove L, Stachura R, et al. The opportunity loss of boarding admitted patients in the emergency department. Acad Emerg Med. 2007 Apr;14(4):332–7. [PubMed]
6. Falvo T, Grove L, Stachura R, et al. The financial impact of ambulance diversions and patient elopements. Acad Emerg Med. 2007 Jan;14(1):58–62. [PubMed]
7. McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey 2003. Emergency Department Summary: Advance Data from Vital and Health Statistics, No. 358. Hyattsville, MD: National Center for Health Statistics; 2005.
8. Schull MJ, Lazier K, Vermeulen M, et al. Emergency department contributors to ambulance diversion: a quantitative analysis. Ann Emerg Med. 2003;41:467–476. [PubMed]
9. Viccellio P, Schroffel B, Schiavone F. Emergency Department Full Capacity Protocol. Stony Brook University Hospital and Medical Center. Available at:http://www.hospitalovercrowding.com/fullcapacity.htm. Accessed April 7, 2009.
10. Sprivulis PC, Da Silva JA, Jacobs IG, et al. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. MJA.2006;184:208–212. [PubMed]
11. Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. MJA. 2006;184:213–216. [PubMed]
12. Garson C, Hollander JE, Rhodes KV, et al. Emergency department patient preferences for boarding locations when hospitals are at full capacity. Ann Emerg Med. 2008;51:9–12. [PubMed]
13. Siegel B. “The emergency department: rethinking the safety net for the safety net. The ED is a key element of today’s health care system, and it needs to be given adequate support to expand beyond its traditional role,” Health Affairs. Mar 24, 2004. pp. W4–146. Web Exclusive, Health Affairs Website. Available at: http://content.healthaffairs.org/cgi/content/full/hlthaff.w4.146v1/DC1. Accessed July 6, 2008. [PubMed]
14. Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006;13:1300–1303. 355;[PubMed]
15. Hunt KA, Weber EJ, Showstack JA, et al. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006;48:18–20. [PubMed]


