| Author | Affiliation |
|---|---|
| Shahram Lotfipour, MD, MPH | University of California, Irvine School of Medicine, Department of Emergency Medicine |
| Shawn K. Kaku, MD | University of California, Irvine School of Medicine, Department of Emergency Medicine |
| Federico E. Vaca, MD, MPH | University of California, Irvine School of Medicine, Department of Emergency Medicine |
| Chirag Patel, MD | University of California, Irvine School of Medicine, Department of Surgery |
| Craig L. Anderson, PhD, MPH | University of California, Irvine School of Medicine, Department of Emergency Medicine |
| Suleman S. Ahmed, BS, BA | University of California, Irvine |
| Michael D. Menchine, MD, MPH | University of California, Irvine School of Medicine, Department of Emergency Medicine |
ABSTRACT
Introduction:
To determine the prevalence of adverse events in elderly trauma patients with isolated blunt thoracic trauma, and to identify variables associated with these adverse events.
Methods:
We performed a chart review of 160 trauma patients age 65 and older with significant blunt thoracic trauma, drawn from an American College of Surgeons Level I Trauma Center registry. Patients with serious injury to other body areas were excluded to prevent confounding the cause of adverse events. Adverse events were defined as acute respiratory distress syndrome or pneumonia, unanticipated intubation, transfer to the intensive care unit for hypoxemia, or death. Data collected included history, physical examination, radiographic findings, length of hospital stay, and clinical outcomes.
Results:
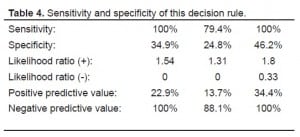
Ninety-nine patients had isolated chest injury, while 61 others had other organ systems injured and were excluded. Sixteen patients developed adverse events [16.2% 95% confidence interval (CI) 9.5–24.9%], including two deaths. Adverse events were experienced by 19.2%, 6.1%, and 28.6% of those patients 65–74, 75–84, and ≥85 years old, respectively. The mean length of stay was 14.6 days in patients with an adverse event and 5.8 days in patients without. Post hoc analysis revealed that all 16 patients with an adverse event had one or more of the following: age ≥85, initial systolic blood pressure <90 mmHg, hemothorax, pneumothorax, three or more unilateral rib fractures, or pulmonary contusion (sensitivity 100%, CI 79.4–100%; specificity 38.6%, CI 28.1–49.9%).
Conclusion:
Adverse events from isolated thoracic trauma in elderly patients complicate 16% of our sample. These criteria were 100% sensitive and 38.5% specific for these adverse events. This study is a first step to identifying variables that might aid in identifying patients at high risk for serious adverse events.
INTRODUCTION
Increasing age has been found to be an independent risk factor for a poor outcome after traumatic injury.1 Elderly patients (defined as 65 years and older) have up to four-fold greater morbidity and mortality compared with injury severity score-matched younger patients, especially due to thoracic and head injuries.1–11 The Glasgow Coma Scale assesses the severity and probability of survival in an elderly trauma patient with head injury, yet there is currently no reliable method to prospectively determine severity of thoracic injuries in elderly patients with blunt thoracic trauma. Further, little is known about the incidence of complications from isolated thoracic injury in the elderly, as well as the variables that may predict them.
As thoracic injury is second only to head injury as a factor contributing to death in the elderly trauma victim, reliable assessment is essential.9 Rib fractures are the most common injury found in elderly blunt chest trauma patients, and each additional rib fracture increases the odds of dying by 19% and of developing pneumonia by 27%.11,12Elderly trauma patients also have a higher incidence of respiratory complications and infections.13 Without reliable factors associated with complications and mortality, fear of adverse events [(including pneumonia, acute respiratory distress syndrome (ARDS), unanticipated intubation, transfer to the intensive care unit (ICU) for hypoxemia, and death secondary to pulmonary sequelae], may dictate an overly conservative approach to management, resulting in routine admission for observation.
The goal of this study was to determine if the conservative approach to elderly trauma victims with thoracic injury can be modified. To accomplish this, we first describe the incidence of adverse events in elderly trauma patients with isolated thoracic injuries, and then identify a set of patient variables that are associated with adverse events.
METHODS
Our project was reviewed by the local institutional review board. We identified subjects from an American College of Surgeons Level I Trauma Center patient registry. The trauma registry prospectively collects data on all trauma team activations including age; sex; mechanism of injury; abbreviated injury scale (AIS) for head and neck, face, thorax, abdomen/pelvis extremity and external injury; number of days in the hospital; and whether the patient was transferred to another facility. AIS describes the severity of injury to one body region on a six-point scale: 1 minor, 2 moderate, 3 serious, 4 severe, 5 critical, 6 unsurvivable.14
Using the trauma registry, we identified 160 patients age ≥65 with AIS of 1–5 in the thoracic region between January 1998 and December 2002. Patients with serious injury to other body areas (AIS ≥3) were excluded to limit confounding the cause of adverse events. Ninety-nine patients had isolated chest injury, and their charts underwent a structured review by one researcher who was blinded to the purpose of the study. The data was recorded using a Microsoft Access 2000 structured data form.
Outcome Variables
The outcome variables of interest were the following adverse events: pneumonia, ARDS, unanticipated endotracheal intubation, need to transfer the patient to the ICU for hypoxemia, and death from pulmonary sequelae. The cause of death was determined from the death certificate.
Candidate Predictor Variables
To find the variables associated with the adverse events of interest, 60 candidate predictor variables were collected in the categories of historical information, radiography, physical examination, and laboratory findings.
Historical information: Age; sex; weight; height; body mass index; mechanism of injury; the presence of a seatbelt sign; tobacco use (current, past use, or never); need for home oxygen; past medical history of coronary artery disease; heart failure; cardiac valvular disease; arrhythmia; pacemaker or defibrillator; coronary artery bypass graft; asthma; chronic obstructive pulmonary disease; diabetes; kidney disease; liver disease; cancer; and current use of aspirin, warfarin, clopidogrel (Plavix), or steroids.
Radiography: Identification by plain radiograph or computed tomography of hemothorax; pneumothorax; pulmonary contusion; flail chest; widened mediastinum; long bone, pelvic, clavicle, scapula, sternum, cervical, thoracic, lumbar spine, or rib fractures; spinal cord injury; and where appropriate, whether injuries were unilateral or bilateral.
Physical exam information: Systolic blood pressure (SBP) in the field; emergency department (ED) vital signs including initial Glasgow Coma Scale score, SBP, heart rate, and respiratory rate with or without assistance, oxygen saturation on room air and/or with supplementation and the amount of supplemental oxygen given both at the time of arrival to the ED as well as 24 hours later; presence of injury as well as the AIS score for the head/neck, face, thorax, abdomen/pelvis, extremity, and external injury.
Laboratory information: Alcohol level; toxicology screen results; presence of an abnormal ECG; presence of sinus tachycardia; anion gap; lactate level; and presence of metabolic acidosis.
RESULTS
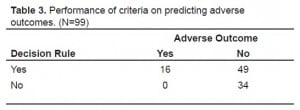
Characteristics of the sample are summarized in Table 1 (viewable under related files at:http://repositories.cdlib.org/uciem/westjem/vol10/iss2/art4/). Mean age was 75 years. Most (75%) were victims of a motor vehicle crash, and many had co-morbid medical conditions. Sixteen of the 99 patients developed one of the five pre-defined adverse events [16.2% 95% Confidence Interval (CI) 9.5–24.9%] including two deaths [Table 2(viewable under related files at:http://repositories.cdlib.org/uciem/westjem/vol10/iss2/art4/)]. Adverse events were experienced by 19.2%, 6.1%, and 28.6% of those patients 65–74, 75–84, and ≥85 years old, respectively. All 99 patients were admitted and 68.7% went to the ICU. The mean length of hospital stay was 5.8 days in patients without an adverse event and 14.6 days with an adverse event. Post hoc data analysis revealed that the presence of any one of the following were identified in all 16 cases that developed an adverse event: age ≥ 85, initial SBP < 90 mm Hg, hemothorax, pneumothorax, three or more unilateral rib fractures, or pulmonary contusion on chest radiograph (Table 3). The sensitivity and specificity of this decision rule is shown in Table 4.


DISCUSSION
According to the US Census Bureau, during the last century the number of people over age 65 has increased 11-fold, and this number will double over the next 25 years.8,15 The elderly population has the highest hospitalization rate after injury.9,15 Currently, the approximately 13% of the U.S. population over 65 accounts for almost one-third of all deaths from injury, and incurs a higher population-based death rate than any other age group.9 This makes the ability to effectively treat and manage elderly patients of extreme importance, especially as this group continues to grow.
Unfortunately, we lack the data to predict complications in this patient group. In fact, prior studies have not characterized the risk of complications in isolated thoracic trauma patients. Without the ability to predict complications, physicians have adopted conservative management, often admitting even in the absence of visible injuries.17 We found that 16.2% of elderly thoracic trauma patients developed an adverse event, most commonly pneumonia and rarely respiratory failure or death, which suggests the possibility of developing prediction instruments to identify groups at high and low risk. However, the small proportion of people who developed delayed complications highlights the difficulty in developing such an instrument. Generally, one would require 10–15 adverse events per candidate predictor variable. We had far fewer than this. On the basis of this study depending on the number of variables in the model and the confidence interval desired one can calculate the sample size needed to determine a reliable set of criteria. If we can assume that 16% will get complications, the decision rule to be 95% accurate and accept a lower limit of the 90% CI, then we would require a prospective study that finds 150 elderly thoracic trauma patients with adverse outcomes, which would require 1000 elderly thoracic trauma patients for enrollment.
In the second part of our study, we identified a set of patient variables that may predict complications. The presence of these variables – age ≥ 85, initial systolic blood pressure < 90 mm Hg, hemothorax, pneumothorax, three or more unilateral rib fractures, or pulmonary contusion – were 100% sensitive and 38.5% specific for predicting the development of one of the predefined outcome variables. This sensitive set of criteria may aid in modifying the current conservative approach, because the absence of these findings may identify patients at a sufficiently lower risk for a serious adverse event who may require only limited observation. While these criteria are intriguing, the small numbers of patients who suffered adverse events with the large number of candidate predictor variables should cause readers to interpret the results with extreme caution. We intend these results to imply that developing a set of criteria is worthwhile and feasible.
LIMITATIONS
Our study has several important limitations. The major limitation was the small number of adverse events and the large number of candidate variables used to determine a set of low-risk criteria. As such, this study can only be viewed as a first, exploratory step to identify criteria capable of predicting delayed complications. It should be noted that the criteria that we report: 1) age ≥85; 2) initial SBP < 90 mm Hg; 3) hemothorax, pneumothorax; 4) three or more unilateral rib fractures; and 5) pulmonary contusion have significant face validity. Still, we would admonish readers to consider these results as definitive. Our data were collected at a single institution, yielding a small sample with limited external generalizability. In addition, the small sample size yields a point estimate of sensitivity with wide confidence intervals. External validation with a large data set, then prospective validation will be required before these results should be used to supplant usual care in the management of elderly thoracic trauma patients.
CONCLUSION
This study reports that 16.2% of elderly thoracic trauma patients suffer a delayed adverse event. A post hoc set of predictor variables, if absent, identified patients less likely to develop an adverse event. These were: 1) age≥85, 2) initial SBP < 90, 3) hemothorax, pneumothorax, 4) three or more unilateral rib fractures, 5) pulmonary contusion. This represents the first step in the lengthy process of validating a decision rule. In its current form readers should not adopt these criteria to make significant clinical decisions. If these criteria are validated in a much larger data set, perhaps a national trauma registry, these criteria could be used to aid in the management of elderly trauma patients and help modify the current conservative approach to their treatment.
Footnotes
We would like to thank Dr. Michael E. Lekawa and Ms. Stephanie Lush for providing the data from the University of California, Irvine Medical Center Trauma registry.
Supervising Section Editor: Teresita M. Hogan, MD
Submission history: Submitted October 28, 2007; Revision Received March 29, 2009; Accepted April 01 2009.
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Michael D. Menchine, MD, MPH. Department of Emergency Medicine. 101 The City Drive, Rte 128-01 Orange, CA 92868
Email: mmenchin@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Evans L. Age and fatality risk from similar severity impacts. Journal of Traffic Medicine. 2001;29:10–19.
2. Holcomb JB, McMullin NR, Kozar RA, Lygas MH, Moore FA. Morbidity from rib fractures increases after age 45. J Am Coll Surgeons. 2003;196:549–555.
3. Khattak AJ, Pawlovich MD, Souleyreete RR, Hallmark SL. Factors related to more severe older driver traffic crash injuries. J Transp Eng. 2002. May–Jun. pp. 243–249.
4. Kulshrestha P, Munshi I, Wait R. Profile of chest trauma in a level 1 trauma center. J Truama. 2004;57:576–581.
5. Li G, Braver ER, Chen L. Fragility versus excessive crash involvement as determinants of high death rates per vehicle-mile of travel among older drivers. Accident Anal Prev.2001;35:227–235.
6. Linman ST, Kuzucu A, Tastepe AI, Ulasan GN, Topcu S. Chest injury due to blunt trauma. Eur J Cardio-Thorac. 2003;23:374–378.
7. Stawicki SP, Grossman MD, Hoey BA, et al. Rib fractures in the elderly: a marker of injury severity. J Am Geriatr Soc. 2004;52:805–808. [PubMed]
8. Victorino GP, Chong TJ, Pal JD. Trauma in the elderly patient. Arch Surg-Chicago.2003;138:1093–1098. [PubMed]
9. Wang SC, Schneider L. An aging population: fragile, handle with care. Proceedings of the National Highway Traffic Safety Administration. 1999
10. Zhang J, Lindsay J, Clarke K, Robbins G, Mao Y. Factors affecting the severity of motor vehicle traffic crashes involving elderly drivers in Ontario. Accident Anal Prev.2000;32:117–125.
11. Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. J Trauma. 2000;48:1040–1046. [PubMed]
12. Shorr RM, Rodriguez A, Indeck MC, Crittenden MD, Hartunian S, Cowley RA. Blunt chest trauma in the elderly. J Trauma. 1989;29:234–237. [PubMed]
13. Schiller WR, Knox R, Chleborad W. A five-year experience with severe injuries in elderly patients. Accident Anal Prev. 1995;27:167–174.
14. Association for the Advancement of Automotive Medicine. The Abbreviated Injury Scale (AIS) 1985 revision. AAAM; Des Plaines, IL: 1985.
15. Bergman M, Farrer S, Joy L. Dramatic changes in US aging highlighted in new census, NIH Report. U.S Census Bureau web site. Available at:http://www.census.gov/Press-Release/www/releases/archives/aging_population/006544.html. Accessed October 2007.
16. Hall MJ, Owings MF. Hospitalizations for Injury: United States, 1996. Advanced Data.2000;318:1–12.
17. DeMaria EJ. Evaluation and treatment of the elderly trauma victim. Clin Geriatr Med. 1993;9:461–71. [PubMed]


