| Author | Affiliation |
|---|---|
| Shan W. Liu, MD, SD | Massachusetts General Hospital, Harvard Medical School, Department of Emergency Medicine, Boston, Massachusetts |
| Azita G. Hamedani, MD, MPH | University of Wisconsin, Department of Medicine and Public Health, Madison, Wisconsin |
| David F.M. Brown, MD | Massachusetts General Hospital, Harvard Medical School, Department of Emergency Medicine, Boston, Massachusetts |
| Brent Asplin, MD | Fairview Medical Group, St. Paul, Minnesota |
| Carlos A. Camargo, Jr, MD, DrPH | Massachusetts General Hospital, Harvard Medical School, Department of Emergency Medicine, Boston, Massachusetts Harvard School of Public Health, Department of Epidemiology, Boston, Massachusetts |
ABSTRACT
Introduction:
The American College of Emergency Physicians (ACEP) Task Force on Boarding described high-impact initiatives to decrease crowding. Furthermore, some emergency departments (EDs) have implemented a novel initiative we term “vertical patient flow,” i.e. segmenting patients who can be safely evaluated, managed, admitted or discharged without occupying a traditional ED room. We sought to determine the degree that ACEP-identified high-impact initiatives for ED crowding and vertical patient flow have been implemented in academic EDs in the United States (U.S.).
Methods:
We surveyed the physician leadership of all U.S. academic EDs from March to May 2010 using a 2-minute online survey. Academic ED was defined by the primary site of an emergency residency program.
Results:
We had a response rate of 73% (106/145) and a completion rate of 71% (103/145). The most prevalent hospital-based initiative was inpatient discharge coordination (46% [47/103] of respondents) while the least fully initiated was surgical schedule smoothing (11% [11/103]). The most prevalent ED-based initiative was fast track (79% [81/103]) while the least initiated was physician triage (12% [12/103]). Vertical patient flow had been implemented in 29% (30/103) of responding EDs while an additional 41% (42/103) reported partial/in progress implementation.
Conclusion:
We found great variability in the extent academic EDs have implemented ACEP’s established high-impact ED crowding initiatives, yet most (70%) have adopted to some extent the novel initiative vertical patient flow. Future studies should examine barriers to implementing these crowding initiatives and how they affect outcomes such as patient safety, ED throughput and patient/provider satisfaction.
INTRODUCTION
Emergency department (ED) crowding continues to burden patients and providers.1 ED crowding has led to delays in care, increased mortality, and decreased patient satisfaction.2–6 The cause of ED crowding is multifactorial and is generally thought to be secondary to input, throughput and output factors.7 Many initiatives to reduce ED crowding at every level have been described in the literature and include efforts such as ambulance diversion (input), increasing staffing (throughput), and boarding of patients in inpatient hallways.1,8,9
Among the many initiatives described to address ED crowding, the American College of Emergency Physicians (ACEP) Task Force on Boarding in particular highlighted high-impact initiatives, such as inpatient discharge coordination (inpatient concerted efforts to discharge patients before noon), inpatient full capacity protocols (moving admitted ED patients to inpatient areas such as hallways when ED is at full capacity), cancelling elective surgeries, surgical schedule smoothing (spreading elective surgery days over the entire week), fast track unit, bedside registration, observation unit, ED bed expansion, and physician triage.10 While these ACEP initiatives may be high-impact, some may be difficult to implement because they require systemwide interventions or considerable funds for construction. One key area that is more operationally within the control of the ED is improving ED throughput efficiency through streamlining front-end operations. Certain EDs have adopted front-end solutions addressing crowding, such as immediate bedding (i.e. patients go immediately to treatment room before triage and registration), triage protocols, and implementation of fast-track areas.8 In particular, some EDs identify patients who can be safely evaluated, managed, admitted or discharged, without occupying ED rooms. In this novel front-end initiative, which we term “vertical patient flow,” patients typically sit upright in chairs awaiting treatment or tests. Vertical patient flow has potential to combine many of the best aspects of ACEP’s high-impact solutions (evaluation of low acuity, fast-track type patients and physician triage), and can also allow for billing of physician services. However, little research exists describing this initiative, despite being highlighted by the Institute of Healthcare Improvement as a lean healthcare component.11
A survey of EDs in 4 states of the United States (U.S.) found ACEP’s high-impact solutions were more likely used by hospitals that were overcapacity.12 However, we do not know the extent to which these initiatives, especially vertical patient flow, have been implemented across academic EDs (defined as the primary site of an emergency residency program) which have higher median annual volume.13 Furthermore, while studies have examined physicians working in triage, none focus on patients who do not occupy ED rooms.14–18
We sought to determine the degree that ACEP-identified high-impact interventions for ED crowding and a newer initiative termed vertical patient flow have been implemented in academic EDs in the U.S.
METHODS
Study Design
We conducted an electronic survey of physician leadership (division chief or department chair) of every U.S. academic ED from March to May 2010. Academic ED was defined by the primary site of an emergency residency program according to the Accreditation Council for Graduate Medical Education (ACGME). We identified physician leaders of these sites from the Society for Academic Emergency Medicine (SAEM) residency list and phone calls to individual programs.
Study Protocol and Measurements
We created an online survey instrument that was piloted on 10 emergency medicine physicians at our institutions and revised following feedback. The revised survey was then e-mailed to ED physician leaders (survey is available online). Non-responders were e-mailed up to 3 more times at 2- and 4-week intervals after initial mailing. Data collected included hospital name, number of hospital and ED beds, annual ED volume, average ED length of stay (LOS), percent of ED patients admitted, and the degree to which various hospital and ED crowding initiatives had been implemented. To improve response rates, we limited survey length to 2 minutes and focused on high-impact solutions outlined by the ACEP Boarding Task Force.10 We also asked respondents whether, how, and to what degree vertical patient flow had been implemented.
We treated questions not completed as a non-response, rather than a negative response, resulting in fewer responses to certain individual questions than the total number of respondents. We corrected errors (e.g. contact information or abnormal responses for ED size) using data, if available, from hospital websites.
Data Analysis
We administered the survey using Surveymonkey.com (Palo Alto, California) and calculated descriptive statistics using Microsoft Excel (2007). We used the Wilcoxon rank-sum test, chi-square, and Fisher exact tests where appropriate to compare responder and non-responders using Stata version 11).
This project was exempted by the university institutional review board. Survey participants were informed that responses were confidential and only aggregate results would be used.
RESULTS
We identified 152 academic sites eligible for inclusion in the study. We excluded 2 sites as correct email addresses could not be located despite phone calls. We also excluded 5 sites where there were discrepancies between what respondents self-reported as their primary institution and the site identified through SAEM. Of 145 (73%) academic ED physician leaders, 106 responded to the survey, of which 103 completed it (97%, [103/106] or 72% [103/145] of total surveys). The median annual visit volume among respondents was 67,085 (interquartile range [IQR] 52,037–85,440). Geographic location was as follows: 31% Northeast, 24% South, 29% Midwest and 16% West; 100% of respondents were urban. Using data extracted from the National Emergency Department Inventory-USA, there were no statistically significant differences between respondents and non-respondents with regards to annual volume, urban versus rural hospitals, or geographic location. The median reported staffed hospital beds was 590 (IQR 450–748), the median annual ED volume was 73,000 (IQR 55,000–86,000) visits and median ED LOS was 4.5 (IQR 3.7–6.0) hours. A median of 24% (IQR 21–29.5) of ED patients reportedly were admitted to the hospital.
Table 1 shows the proportion of respondents who initiated certain hospital- and ED-crowding solutions. The most prevalent hospital-based initiative was inpatient discharge coordination (46%) while the least fully initiated was surgical schedule smoothing (11%), as reported by respondents. The most prevalent ED-based initiative reported was fast track (79%) while the least was physician triage (12%).
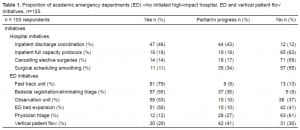
Proportion of academic emergency departments (ED) who initiated high-impact hospital, ED and vertical patient flow initiatives, n=103.
Seventy percent of respondents reported either full (29%) or partial/in progress (41%) implementation of vertical patient flow (Table 1). Two-thirds (48/72) of EDs using vertical patient flow stated that implementation occurred by design (i.e. intentionally, as opposed to ad hoc). Of those implementing vertical patient flow by design, 65% (31/48) reported doing so daily. Of the EDs using vertical patient flow, 61% (44/72) reported evaluating urgent patients (i.e. emergency severity index [ESI] of 3, 4, and 5) in this manner, while the remaining 39% (28/72) reserved it for the lowest-acuity patients (i.e., ESI 4 and 5).
EDs using vertical patient flow most frequently reported that physicians (85%, [61/72]) staffed these patients, while a large portion also reported using nurse practitioners (42%, [30/72]) and physician assistants (47%, [34/72]; answers were not mutually exclusive). Half (36/72) of vertical patient flow EDs reported using dedicated space for such patients, 46% reported returning them to the waiting room (46%, [33/72]), and 26% reported leaving them in triage rooms (26%, [19/72]) to await further testing, intervention, and results (answers were not mutually exclusive).
DISCUSSION
We found great variability in the extent academic EDs have implemented ACEP’s high-impact ED crowding initiatives, yet most have adopted the novel initiative vertical patient flow to some extent. Regarding hospital-based initiatives, not surprisingly, inpatient discharge coordination was the most frequently adopted, as opposed to implementing a full-capacity protocol or cancelling/changing elective surgical scheduling. These latter strategies require substantial institutional support, and their financial impact can vary among institutions. Among ED-based initiatives, fast-track units were most widely adopted. Initiatives requiring extensive planning, capital investment, and construction, such as an observation unit or expanding the ED, were less likely to be initiated.
Our findings are most directly comparable to Handel’s12 study, which examined implementation of ACEP’s crowding solutions across all EDs in 4 states. We found 89% of all academic EDs have implemented (46% initiated and 43% partial/in progress) inpatient-discharge coordination, as opposed to 69% in Handel’s study.12 We found 88% have implemented fast track units and 63% have implemented observation units, as opposed to 51% and 24% found in Handel’s study. This greater adoption of crowding solutions among academic EDs may reflect the higher annual visit volume (and likely accompanying degree of crowding) or geographical representation.
Despite being a novel concept, vertical patient flow seems to have been adopted in many academic EDs. It uses the aspects of fast track and physician triage, siphoning off lower-acuity patients from traditional ED rooms. Also, pure physician triage models require staffing with expensive providers; vertical patient flow allows billing for physicians services. Staff acceptance of vertical patient flow may be greater than for physician triage given the ability to provide the full spectrum of care (rather than just front-end triage) and less overt infringement on triage nursing responsibilities. Furthermore, vertical patient flow requires little construction or political cooperation from other hospital services. However, discharging patients without allowing patients to undergo a full nursing evaluation or wear a gown may increase misdiagnosis.
While no study has focused on vertical patient flow, research shows physician triage decreases ED LOS.14–18 While the two policies are not synonymous (i.e. if nurse practitioners are evaluating vertical patient flow patients or if physicians are in the front-end of the ED but not triaging), the physician triage literature illuminates how vertical patient flow may also decrease ED LOS. Specifically, Partovi et al14 found that having additional faculty members at triage reduced ED LOS by 82 minutes. They noted that 46 patients were seen and discharged by physicians directly from triage compared to 4 patients on non-faculty triage days, which likely contributed to the decreased ED LOS finding. White et al15 also found that a supplemented triage and rapid treatment system was associated with a LOS decrease despite increases in overall patient volume. Holroyd et al16 found that having a triage liaison physician decreased ED LOS by 36 minutes compared to control days. Subash et al17 also found that their intervention of team triage (physician and nurse triage) reduced demands for space as more patients are “treated and streeted” and never wait in a cubicle. They found that more patients were treated and discharged within 20 minutes in their intervention group compared with their control group (19% vs. 3%). Rowe et al18 pooled data from Holroyd and Subash and found that a triage liaison resulted in shorter ED LOS compared to nurse-led triage by nearly 37 minutes.
ED crowding will only become more of an issue in the future and consequently a factor in medical litigation. Pitts et al19 analyzed data from the National Hospital Ambulatory Medical Care Surveys and found that ED visits increased by 1.9% per year, a rate 60% faster than the population’s growth. Furthermore, mean occupancy grew even more at 3.1% per year.19 As ED crowding has been associated with lower quality of care, it may be increasingly be related to medical legal cases. 2–6 In the case of Scruggs v. Danville Regional Medical Center of Virginia, the patient was deemed as “non-urgent” based on a nursing triage. The physician evaluated the patient 11.5 hours later; 30 minutes after that the patient was found to be in respiratory and cardiac arrest. He later sued the hospital for failing to provide an adequate medical screening exam.20 Crowding was not even mentioned in the judge’s decision. It is not even clear that proving an ED is crowded helps or hurts in a lawsuit.21Blaming crowding for less-than-ideal outcomes may make the hospital or ED physician appear to have fallen below the standard of care; plaintiff attorneys may question why additional resources were not recruited. On the other hand, jurors may be more sympathetic to physicians who can demonstrate needing to multitask on numerous sick patients simultaneously. While there has been no legal precedent to use crowding as a defense, there may be cases in the future where “too crowded” is used.21 In the meantime, this indicates that finding methods to manage ED crowding will only grow in importance.
LIMITATIONS
While both survey response and completion rates were high (73% and 71%), non-respondents could have possibly answered in ways that would change our results. In addition to inherent recall bias, the responses reflected 1 site respondent. Given that this survey has not been conducted before, our instrument was not validated. However, we piloted our instrument and revised it accordingly. Our results may not generalizable to many EDs given our focus on academic EDs. Our results also assume academic EDs are crowded and have some level of hospital cooperation to implement these initiatives. Our survey did not specifically ask nor did we get a sense from respondents whether their ED was crowded or whether they lacked hospital cooperation. However, a substantial number (42%, 42/106) of respondents listed ways beyond the ACEP policies that they attempted to implement to improve ED flow, suggesting crowding is likely prevalent. Furthermore, our survey could not determine if strategies were ultimately abandoned or effective. Also, physician leaders reported 2009 data; it is possible responses may differ from the present situation. Finally, we could have included other ED crowding initiatives solutions, but thought increasing survey length would decrease response rates.
CONCLUSION
Established high-impact hospital and ED initiatives have been implemented to a variable extent in the academic institutions in our survey sample despite being recommended by ACEP. While there has been momentum to see crowding as a problem requiring hospital-wide solutions, our data show initiatives requiring extensive institutional support and capital investment, such as an observation unit or expanding the ED, were less likely to be initiated. The novel front-end strategy vertical patient flow has been initiated in most academic hospitals and seems to combine the benefits of described crowding solutions without requiring much institution-wide support or capital investment; whether it is a high-impact solution is unclear. Future studies should examine the barriers to implementing these crowding initiatives and how they affect outcomes such as patient safety, ED LOS, and patient/provider satisfaction. However, until there is widespread adoption of high-impact crowding solutions, ED crowding will continue to burden hospitals.
Footnotes
Supervising Section Editor: Jeffrey Druck, MD
Submission history: Submitted March 3, 2012; Revisions received July 24, 2012; Accepted November 21, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.11.12171
Address for Correspondence: Shan Liu, MD, SD, Department of Emergency Medicine, Massachusetts General Hospital, 55 Fruit Street, Zero Emerson, Room 358, Boston, MA 02114. Email: sliu1@partners.org.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136. [PubMed]
2. Schull MJ, Vermeulen M, Slaughter G, et al. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med. 2004;44:577–585. [PubMed]
3. Pines JM, Hollander JE. Emergency Department Crowding Is Associated With Poor Care for Patients With Severe Pain. Ann Emerg Med. 2008;51:1–5. [PubMed]
4. Pines JM, Localio AR, Hollander JE, et al. The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Acad Emerg Med. 2006;13:873–878. [PubMed]
5. Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust. 2006;184:213–216. [PubMed]
6. Pines JM, Iyer S, Disbot M, et al. The Effect of Emergency Department Crowding on Patient Satisfaction for Admitted Patients. Acad Emerg Med. 2008;15:825–831. [PubMed]
7. Asplin BR, Magid DJ, Rhodes KV, et al. A conceptual model of emergency department crowding.Ann Emerg Med. 2003;42:173–180. [PubMed]
8. Wiler JL, Gentle C, Halfpenny JM, et al. Optimizing emergency department front-end operations.Ann Emerg Med. 2010;55:142–160. [PubMed]
9. Viccellio A, Santora C, Singer AJ, et al. The association between transfer of emergency department boarders to inpatient hallways and mortality: a 4-year experience. Ann Emerg Med. 2009;54:487–491. [PubMed]
10. ACEP Boarding Task Force Emergency Department Crowding: High-Impact Solutions. Available at: http://www.acep.org/content.aspx?id=32050. Accessed June 5, 2012.
11. Institute for Healthcare Improvement Getting Lean in the ED. Available at:http://www.ihi.org/IHI/Topics/Flow/EmergencyDepartment/ImprovementStories/GettingLeanintheED.htm. Accessed February 6, 2011.
12. Handel D, Ginde A, Raja A, et al. Implementation of crowding solutions from the American College of Emergency Physicians Task Force Report on Boarding. Int J Emerg Med. 2010;3:279–286.[PMC free article] [PubMed]
13. Sullivan AF, Richman IB, Ahn CJ, et al. A profile of US emergency departments in 2001. Ann Emerg Med. 2006;48:694–701. [PubMed]
14. Partovi SN, Nelson BK, Bryan ED, et al. Faculty triage shortens emergency department length of stay. Acad Emerg Med. 2001;8:990–995. [PubMed]
15. White BA, Brown DF, Sinclair J, et al. Supplemented Triage and Rapid Treatment (START) Improves Performance Measures in the Emergency Department. J Emerg Med. 2012;42:322–328.[PubMed]
16. Holroyd BR, Bullard MJ, Latoszek K, et al. Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial. Acad Emerg Med.2007;14:702–708. [PubMed]
17. Subash F, Dunn F, McNicholl B, et al. Team triage improves emergency department efficiency.Emerg Med J. 2004;21:542–544. [PMC free article] [PubMed]
18. Rowe BH, Guo X, Villa-Roel C, et al. The role of triage liaison physicians on mitigating overcrowding in emergency departments: a systematic review. Acad Emerg Med. 2011;18:111–120.[PubMed]
19. Pitts SR, Pines JM, Handrigan MT, et al. National trends in emergency department occupancy, 2001–2008: effect of inpatient admissions versus emergency department practice intensity. Ann Emerg Med. 2012;60:679–686. [PubMed]
20. Everett Wayne Scruggs v. Danville Regional Medical Center of Virginia, L.L.C., Case No. 4:08CV00005 (W.D. Va. Sept. 5, 2008). Available at:http://www.vawd.uscourts.gov/OPINIONS/KISER/8-5MEMOOPINION.PDF. Accessed July 24, 2012.
21. Editor, Does proving an ED was crowded help or hurt in a lawsuit? ED Legal Letter. Mar 1, 2009.


